Analysis on drug resistance characteristics and risk factors for extensively drug resistant tuberculosis patients
-
摘要:
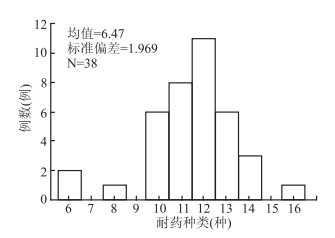
目的 分析广泛耐药结核病(extensively drug-resistant tuberculosis,XDR-TB)患者对一、二线抗结核药物耐药情况及危险因素。 方法 收集结核分枝杆菌培阳的住院结核患者,采用分枝杆菌微孔板法药敏检测试可信区间剂盒筛出XDR-TB患者,采用Logistic回归分析XDR-TB患者一、二线抗结核药耐药危险因素。 结果 利福平、异烟肼和利福喷丁耐药率100%,链霉素、利福布汀、乙硫异烟肼、左氧氟沙星和卷曲霉素耐药率90~100%,卡那霉素和对氨基水杨酸耐药率70~80%,阿米卡星耐药率60~70%,丙硫异烟肼耐药率50~60%,乙胺丁醇和莫西沙星耐药率40~50%,克拉霉素耐药率10~20%,氯法齐明耐药率5.2%。XDR-TB中有92.1%的患者对10种以上抗结核药物,耐药种类最少的患者耐6种抗结核药物。Logistic回归分析XDR-TB对一、二线抗结核药物耐药的危险因素包括年龄[20~40岁为(OR=6.318,95%CI:1.204~33.15,P=0.029;40~60岁为(OR=4.772,95%CI:0.973~23.392,P>0.05);60岁以上为(OR=41.366,95%CI:2.909~588.265,P=0.006)]和抗结核治疗史为复治(OR=28.013,95%CI:3.357~233.766,P=0.002)。 结论 XDR-TB患者耐药情况严重,但有药可治,耐药种类多,其危险因素主要来源于年龄和抗结核治疗史。 Abstract:Objective To analyze the drug resistance profile and risk factors for extensively drug resistant tuberculosis (XDR-TB) patients. Methods XDR-TB cases were identified by sixteen anti-TB drug susceptibility kits among inpatients with a diagnosis of laboratory-confirmed mycobacterium tuberculosis. Single-factor and Logistic analysis were used to analyze the risk factors for drug resistant of the first and second-line anti-TB drugs in XDR-TB patients. Results Resistant rate of rifampin, isoniazid and rifampicin were 100%, Resistant rate of streptomycin, rifampicin and dean, b sulfur isoniazid, levofloxacin and capreomycin were from 90% to 100%, resistant rate of kanamycin and amino salicylic acid were from 70% to 80%, resistant rate of amikacin from 60% to 70%, resistant rate of sulfur isoniazid was from 50% to 60%, resistant rate of ethambutol and moxifloxacin were from 40% to 50%, resistant rate of clarithromycin was from 10% to 20%, resistant rate of clofazimine 5.2%. 92.1% of XDR-TB patients were resistant to more than 10 anti-TB drugs, and the least of the patients were resistant to 6 anti-TB drugs.Logistic regression analysis showed the risk factors for XDR-TB first-and second-line anti-tb drugs included age[20-40 year (OR=6.318, 95% CI: 1.204-33.15, P=0.029;40-60 year (OR=4.772, 95% CI: 0.973-23.392, P=0.054); 60 year (OR=41.366, 95% CI: 2.909-588.265, P=0.006)] and anti-TB treatment history was retreatment(OR=28.013, 95% CI: 3.357-233.766, P=0.002). Conclusions XDR-TB patients have serious drug resistance, but there were some drug treatable drug resistance types, and the risk factors mainly come from age and anti-TB treatment history. -
Key words:
- XDR-TB /
- Drug resistance /
- Risk factors
-
表 1 38例XDR-TB患者一、二线抗结核药物耐药率
Table 1. Drug resistance rates of first and second-line anti-TB drugs in 38 XDR-TB patients
药物 耐药病例数(例) 耐药率(%) 药物 耐药病例数(例) 耐药率(%) S 37 97.4 Rfb 35 92.1 R 38 100.0 Km 27 71.7 H 38 100.0 Lfx 36 94.7 E 18 47.4 Cm 35 92.1 Rft 38 100.0 Eto 35 92.1 Am 25 65.8 Pas 29 76.3 Pto 20 52.6 Clx 7 18.4 Mfx 17 44.7 Cfz 4 5.2 表 2 单因素分析XDR-TB对一、二线抗结核药物耐药的危险因素
Table 2. The risk factors of XDR-TB resistance to first and second-line anti-TB drugs by single factor analysis
变量 XDR 非XDR χ2值 P值 性别 0.076 0.783 男 30 29 女 8 9 年龄(岁) 0.683 0.711 0~ 2 4 20~ 14 13 40~ 15 14 60~77 7 7 涂片 0.157 0.692 阴性 3 4 阳性 35 34 空洞 25.544 <0.001 无 9 31 有 29 7 病程(年) 16.152 0.012 0~ 0 10 1~ 18 11 5~ 3 7 10~ 8 4 15~50 9 6 抗结核史 30.389 <0.001 初治 2 25 复治 36 13 吸烟情况 0.054 0.817 不吸烟 16 17 吸烟 22 21 接触史 1.134 0.287 无 3 6 有 35 32 并发症 1.362 0.243 无 18 13 有 20 25 表 3 Logistic多因素分析XDR-TB对一、二线抗结核药物耐药的危险因素
Table 3. Risk factors for XDR-TB resistance to first and second-line anti-TB drugs by Logistic multivariate analysis
变量 β值 sx Wald值 自由度 P值 OR(95% CI)值 年龄(岁,X1) - - - 3 0.032 - 20~X1(1) 1.843 0.846 4.751 1 0.029 6.318(1.204~33.15) 40~X1(2) 1.563 0.811 3.712 1 0.054 4.772(0.973~23.392) 60~X1(3) 3.722 1.354 7.553 1 0.006 41.366(2.909~588.265) 初复治X6 0.093 0.607 0.024 1 0.002 28.013(3.357~233.766) -
[1] Alice L, Martín M, Rachel L. et al. Cytokine kinetics in the first week of tuberculosis therapy as a tool to confirm a clinical diagnosis and guide therapy[J]. PLOS ONE, 2015, 26(6): 1-15. DOI: 10.1371/journal.pone.0129552. [2] Li J, Shen X, Zhang YY, et al. Risk factors for second-line drug resistance in MDR-TB patients in Shanghai[A]. Papers Collection of The National Academic Conference Form Chinese Anti-tuberculosis Association 2011, 2011: 5. [3] Abubakar I, Moore J, Drobniewski F, et al. Extensively drug resistant tuberculosis in the UK: 1995-2007[J]. Thorax, 2009, 64(6): 512-515. DOI: 10.1136/thx.2008.108712. [4] 陆伟, 周扬, 陈诚, 等. 江苏省社区人群结核杆菌耐药状况及影响因素研[J]. 中华疾病控制杂志, 2013, 17(7): 560-563. http://zhjbkz.ahmu.edu.cn/article/id/JBKZ201307004Lu W, ZhouY, Chen C, et al. Prevalence and risk factors for drug resistance tuberculosis in Jiangsu Province: a population based study[J]. Chin J Dis Control Prev, 2013, 17(7): 560-563. http://zhjbkz.ahmu.edu.cn/article/id/JBKZ201307004 [5] 全国结核病耐药性基线调查报告, 中华人民共和国卫生部[M]. 人民卫生出版社. 2010.National baseline survey report on TB resistance, Ministry of health of the People's Republic of China[M]. People's Medical Publishing House. 2010. [6] 初乃惠. 抗结核药物研究进展[J]. 中国实用内科杂志, 2015, 35(8): 655-660. DOI: 10.7504/nk2015070105.Chu NH. Research progress of anti-tuberculosis drugs[J]. Chin J Pract Int Med, 2015, 35(8): 655-660. DOI: 10.7504/nk2015070105. [7] 解燕, 缪昌东, 张德坤. 2012-2014年泰州市痰培养阳性肺结核患者耐药结果分析[J]. 现代预防医学, 2016, 43(21): 4005-4008. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF201621043.htmXie Y, Miao CD, Zhang DK. Drug resistance of tuberculosis among patients with positive sputum culture, Taizhou City, 2012-2014[J]. Modern Preventive Medicine, 2016, 43(21): 4005-4008. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF201621043.htm [8] Kliiman K, Altraja A. Predictors of extensively drug resistant pulmonary tuberculosis[J]. Ann Intern Med, 2009, 150(11): 766-775. DOI: 10.7326/0003-4819-150-11-200906020-00004. [9] Saukkonen JJ, Cohn DL, Jasmer RM, et al. An official ATS statement: hepatotoxicity of antituberculosis therapy[J]. Am J Respir Crit Care Med, 2006, 174(8): 935-952. DOI: 10.1164/rccm.200510-1666ST. [10] 郭秀花. 医学统计学与SPSS软件实现方法[M]. 科学出版社, 2015.Guo XH. Medical statistics and SPSS software implementation method[M]. Science Press. 2015. [11] 马晓梅, 闫国立, 段广才, 等. 决策树模型在手足口病合并脑膜脑炎重症化危险因素中的应用[J]. 中华疾病控制杂志, 2018, 22(9): 961-964. DOI: 10.16462/j.cnki.zhjbkz.2018.09.021.Ma XM, Yan GL, Duan GC. et al. Application of decision tree in the analysis and prediction of risk factors of severe hand, foot and mouth disease combined with meningocephalitis[J]. Chin J Dis Control Prev, 2018, 22(9): 961-964. DOI: 10.16462/j.cnki.zhjbkz.2018.09.021. [12] Walter ND, Strong M, Belknap R, et al. Translating basic science insight into public health action for multidrug and extensively drug-resistant tuberculosis[J]. Respirology, 2012, 17(5): 772-791. DOI: 10.1111/j.1440-1843.2012.02176.x. [13] Cadosch D, Pia AZW, Kouyos R, et al. The role of adherence and retreatment in de novo emergence of MDR-TB[J]. Plos Computational Biology, 2016, 12(3): e1004749. DOI: 10.1371/journal.pcbi.1004749. [14] Lee CH, Wang JY, Lin HC, et al. Treatment delay and fatal outcomes of pulmonary tuberculosis in advanced age: a retrospective nationwide cohort study[J]. BMC Infect Dis, 2017, 17(1): 449-473. DOI: 10.1186/s12879-017-2554-y. [15] Irfan U, Arshad J, Zarfishan T, et al. Pattern of drug resistance and risk factors associated with development of drug resistant mycobacterium tuberculosis in Pakistan[J]. PLOS ONE, 2016, 11(1): e0147529. DOI: 10.1371/journal.pone.0147529. -





 下载:
下载: