-
摘要:
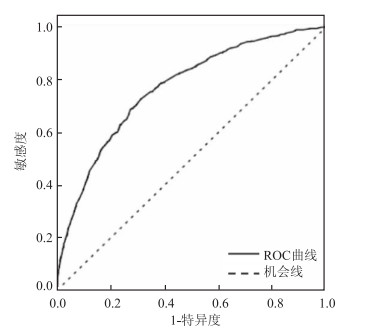
目的 分析影响子痫前期发病的危险因素,建立子痫前期风险评估模型,以期早期评估子痫前期的发生风险。 方法 以山西医科大学第一医院产科于2012年3月-2016年9月分娩的所有产妇为调查对象,进行面对面问卷调查。共收集合格问卷10 319份,排除其他妊娠期相关高血压疾病后,共纳入9 623例,随机抽取其中70%的对象作为训练样本,分析子痫前期的影响因素,建立Logistic回归分析模型,其余30%的对象作为测试样本,验证模型效果。 结果 用训练样本建立Logistic回归分析模型,Logit P=-2.517-0.696×孕前偏瘦+0.200×孕前超重+0.944×孕前肥胖-1.295×居住在城市-0.409×孕前补充过叶酸+1.323×双胎及多胎妊娠+1.708×既往妊娠期高血压病史。Homer-Lemeshow拟合优度检验P=0.377。模型AUC=0.767(95%CI:0.747~0.786,P < 0.001)。用测试样本进行验证模型,得到模型灵敏度81.68%,特异度75.05%,阳性似然比为3.27,阴性似然比为0.24。测试样本模型AUC=0.771(95%CI:0.763~0.790,P < 0.001)。 结论 建立了一个纳入可控因素,且简单、高效的子痫前期风险评估模型,模型拟合度好,灵敏度和特异度较高。 -
关键词:
- 子痫前期 /
- 叶酸 /
- Logistic回归分析模型 /
- ROC曲线
Abstract:Objective To analyze the risk factors affecting pre-eclampsia, to establish a pre-eclampsia risk assessment model, and to assess the risk of pre-eclampsia early. Methods A face-to-face questionnaire survey was conducted for all women who gave birth in the Department of Obstetrics, the First Hospital of Shanxi Medical University from March 2012 to September 2016. A total of 10 319 qualified questionnaires were collected to exclude 9 623 cases of other hypertensive diseases related to pregnancy. A total of 70% of the subjects were randomly selected as training samples to analyze the influencing factors of pre-eclampsia, and a Logistic regression model was established. The remaining 30% of the objects are used as test samples to verify the effect of the model. Results Logistic regression model was established with training samples. Logit P=-2.517-0.696×Pre-pregnancy lean +0.200×Pre-pregnancy overweight +0.944×Pre-pregnancy obesity -1.995×Residential in city -0.409×Folic acid supplemented before pregnancy +1.323×Twin and multiple pregnancy +1.708×History of previous pregnancy hypertension. Homer-Lemeshow test P=0.377. Model AUC=0.767 (95%CI: 0.747-0.786, P < 0.001). Using the test sample to verify the model, the model sensitivity was 81.68%, the specificity was 75.05%, the positive likelihood ratio was 3.27, and the negative likelihood ratio was 0.24. The test sample model AUC=0.771 (95%CI=0.763-0.790, P < 0.001). Conclusion This study establishes a simple and effective pre-eclampsia risk assessment model with controllable factors. The model has good fit and sensitivity and specificity. -
Key words:
- Preeclampsia /
- Folic acid /
- Risk factors Risk assessment model /
- ROC curve
-
表 1 训练样本子痫前期影响因素的单因素分析
Table 1. Univariate analysis of preeclampsia influencing factors in training samples[n(%)]
变量 子痫前期 非子痫前期 χ2值 P值 孕妇年龄(岁) -3.290c 0.001 < 20 519(82.91) 5 303(86.78) 20~ 6(0.96) 68(1.11) ≥35 101(16.13) 740(12.11) 孕前BMI(kg/m2)a -11.279c < 0.001 < 18.5 337(53.92) 4 142(67.95) 18.5~ 52(8.32) 878(14.40) 24~ 161(25.76) 860(14.11) ≥28 75(12.00) 216(3.54) 居住地 319.904 < 0.001 农村 327(52.24) 1 250(20.45) 城市 299(47.76) 4 861(79.55) 人均月收入(元) 8.853c < 0.001 < 2 000 181(28.91) 937(15.33) 2 000~ 402(64.22) 4 357(71.30) ≥5 000 43(6.87) 817(13.37) 文化程度 12.705c < 0.001 小学及以下 41(6.55) 158(2.59) 中学 441(70.45) 2 992(48.96) 大专及以上 144(23.00) 2 961(48.45) 孕前健康教育a 62.832 < 0.001 无 482(77.74) 3 737(61.62) 有 138(22.26) 2 328(38.38) 孕前一年,月经是否规律a 16.179 < 0.001 否 574(92.73) 5 812(96.13) 是 45(7.27) 234(3.87) 阴道出血a 0.915c 0.180 无 563(89.94) 5 405(88.74) 轻微 59(9.42) 639(10.49) 严重 4(0.64) 47(0.77) 孕早期呕吐情况a 1.243c 0.107 无 474(75.72) 4 447(72.90) 轻微 124(19.81) 1 376(22.56) 严重 28(4.47) 277(4.54) 激素治疗a 0.996 0.318 无 594(98.34) 5 774(97.72) 有 10(1.66) 135(2.28) 自然妊娠a 0.000 0.997 否 22(4.08) 213(4.09) 是 517(95.92) 5 001(95.91) 是否为初产 4.256 0.039 否 334(53.35) 2 996(49.03) 是 292(46.65) 3 115(50.97) 产次 6.123 0.013 ≤3 593(94.73) 5 906(96.65) >3 33(5.27) 205(3.35) 孕期前三月发热a 2.101 0.147 无 616(98.88) 5 932(98.05) 有 7(1.12) 118(1.95) 先天性心脏病a 0.377b 无 596(99.67) 5 812(99.45) 有 2(0.33) 32(0.55) 其他心脑血管疾病a 0.639b 无 596(99.67) 5 824(99.64) 有 2(0.33) 21(0.36) 糖尿病a 0.534b 无 602(99.67) 5 862(99.58) 有 2(0.33) 25(0.42) 甲状腺功能亢进a 0.235b 无 597(99.83) 5 815(99.52) 有 1(0.17) 28(0.48) 甲状腺功能减低a 0.640 0.424 无 592(99.00) 5 768(98.60) 有 6(1.00) 82(1.40) 其他内分泌系统疾病a 0.290b 无 597(99.83) 5 818(99.57) 有 1(0.17) 25(0.43) 缺铁性贫血a 0.434b 无 597(99.83) 5 826(99.67) 有 1(0.17) 19(0.33) 病毒性乙型肝炎a 0.356b 无 597(99.83) 5 820(99.62) 有 1(0.17) 22(0.38) 主动吸烟 0.743b 无 624(99.68) 6 094(99.72) 有 2(0.32) 17(0.28) 被动吸烟 18.454 < 0.001 无 507(80.99) 5 325(87.14) 有 119(19.01) 786(12.86) 孕前经常饮酒 0.255b 无 626(100.00) 6 097(99.77) 有 0(0.00) 14(0.23) 孕前经常喝茶 0.000 0.985 无 616(98.40) 6 014(98.41) 有 10(1.60) 97(1.59) 孕前补充过维生素B2 2.950 0.086 无 623(99.52) 6 034(98.74) 有 3(0.48) 77(1.26) 孕前补充过维生素B12 4.580 0.032 无 625(99.84) 6 048(98.97) 有 1(0.16) 63(1.03) 孕前补充过维生素B6 5.706 0.017 无 624(99.68) 6 020(98.51) 有 2(0.32) 91(1.49) 孕前补充过叶酸 39.602 < 0.001 无 493(78.75) 4 057(66.39) 有 133(21.25) 2 054(33.61) 孕早期补充过维生素B6 7.830 0.005 无 606(96.81) 5 750(94.09) 有 20(3.19) 361(5.91) 孕早期补充过叶酸 31.171 < 0.001 无 176(28.12) 1 149(18.80) 有 450(71.88) 4 962(81.20) 经常体育活动 6.105 0.014 无 62(9.90) 439(7.18) 有 564(90.10) 5 672(92.82) 孕期增重(Kg) 1.825 0.177 ≤10 616(98.40) 6 049(98.99) >10 10(1.60) 62(1.01) 本次怀孕胎数 95.840 < 0.001 单胎 561(89.62) 5 939(97.19) 双胎及以上 65(10.38) 172(2.81) 每日吃盐量(g) 3.780 0.052 ≤6 541(86.42) 5 097(83.41) >6 85(13.58) 1 014(16.59) 母亲(或姐妹)患有妊娠期高血压疾病a 0.134 0.714 无 614(99.03) 5 997(99.17) 有 6(0.97) 50(0.83) 妊娠期高血压疾病患病史 112.931 < 0.001 无 593(94.73) 6 071(99.35) 有 33(5.27) 40(0.65) 家族高血压、糖尿病或心血管疾病等慢性病史 11.937 0.001 无 462(73.80) 4 870(79.69) 有 164(26.20) 1 241(20.31) 注:a存在缺失值;bFisher确切概率法;c趋势χ2检验。 表 2 子痫前期影响因素的多因素logistic回归分析
Table 2. Multivariate logistic regression analysis of influencing factors of preeclampsia
参数 β值 Sx Wald χ2值 P值 OR值(95%CI) 常数 -2.517 0.191 173.919 < 0.001 孕前BMI(kg/m2) 18.5~ 1.00 < 18.5 -0.696 0.119 34.504 < 0.001 0.78(0.57~1.06) < 24~ 0.200 0.087 5.298 0.021 1.91(1.54~2.36) < ≥28 0.944 0.116 65.684 < 0.001 4.02(2.97~5.44) 居住地 < 农村1.00 < 城市 -1.295 0.090 208.306 < 0.001 0.27(0.23~0.33) 孕前补充过叶酸 < 否 1.00 < 是 -0.409 0.106 14.782 < 0.001 0.66(0.54~0.82) 本次怀孕胎数 < 单胎1.00 < 双胎及以上 1.323 0.162 67.081 < 0.001 3.75(2.74~5.15) 妊娠期高血压疾病患病史 < 无 1.00 < 有 1.708 0.260 43.041 < 0.001 5.52(3.31~9.19) 表 3 子痫前期风险评估模型评价
Table 3. Evaluation of preeclampsia risk assessment model
预测模型 院内诊断 合计 患者(%) 非患者(%) 高风险 223(81.68) 652(24.95) 875 低风险 50(18.32) 1 961(75.05) 2 011 合计 273 2 613 2 886 -
[1] Bokslag A, Van Weissenbruch M, Mol BW, et al. Preeclampsia; short and long-term consequences for mother and neonate[J]. Early Human Development, 2016, 102: S0378378216304030. DOI: 10.1016/j.earlhumdev.2016.09.007. [2] Steegers EA, Von DP, Duvekot JJ, et al. Pre-eclampsia[J]. Lancet, 2010, 376(9741): 631-644. DOI: 10.1016/S0140-6736(10)60279-6. [3] Bwj M, Roberts CT, Thangaratinam S, et al. Pre-eclampsia[J]. Lancet, 2016, 387(10022): 999-1011. DOI: 10.1016/S0140-6736(15)00070-7. [4] Correa PJ, Palmeiro Y, Soto MJ, et al. Etiopathogenesis, prediction, and prevention of preeclampsia[J]. Hypertension in Pregnancy, 2016, 35(3): 280-294. DOI: 10.1080/10641955.2016.1181180. [5] Mccarthy FP, Ryan RM, Chappell LC. Prospective biomarkers in preterm preeclampsia: a review[J]. Pregnancy Hypertension, 2018, 14: 72-78. DOI: 10.1016/j.preghy.2018.03.010. [6] Agius A, Sultana R, Camenzuli C, et al. An update on the genetics of pre-eclampsia[J]. Minerva Ginecol, 2018, 70(4): 465-479. DOI: 10.23736/S0026-4784.17.04150-8. [7] Yang X, Chen H, Du Y, et al. Periconceptional folic acid fortification for the risk of gestational hypertension and pre-eclampsia: a meta-analysis of prospective studies[J]. Matern Child Nutr, 2016, 12(4): 669-679. DOI: 10.1111/mcn.12209. [8] Azami M, Azadi T, Farhang S, et al. The effects of multi mineral-vitamin D and vitamins (C+E) supplementation in the prevention of preeclampsia: An RCT[J]. Int J Reprod Biomed (Yazd), 2017, 15(5): 273-278. DOI: 10.29252/ijrm.15.5.273. [9] Mujawar SA, Patil VW, Daver RG. Study of Serum Homocysteine, Folic Acid and Vitamin B12 in Patients with Preeclampsia[J]. Indian J Clin Biochem, 2011, 26(3): 257-260. DOI: 10.1007/s12291-011-0109-3. [10] 杨孜, 张为远. 妊娠期高血压疾病诊治指南(2015)[J]. 中华产科急救电子杂志, 2015, 4(4): 206-213. DOI: 10.3760/cma.j.issn.0529-567x.2015.10.001Yang Z, Zhang WY. Guidelines for diagnosis and treatment of hypertensive disorders in pregnancy (2015)[J]. Chin J Obstet Emerg(Electronic Edition), 2015, 4(4): 206-213. DOI:10.3760/cma.j.issn.0529-567x. 2015.10.001. [11] 何雪仪, 王晨虹. 子痫前期预测和预防的研究进展[J]. 国际妇产科学杂志, 2014, 41(2): 171-174. https://www.cnki.com.cn/Article/CJFDTOTAL-GWVC201402023.htmHe XY, Wang CH. Progress in the prediction and prevention of preeclampsia[J]. J Int Obstet Gynecol, 2014, 41(2): 171-174. https://www.cnki.com.cn/Article/CJFDTOTAL-GWVC201402023.htm [12] Talasaz ZH, Sadeghi R, Askari F, et al. First trimesters pregnancy-associated plasma protein-A levels value to predict gestational diabetes mellitus: a systematic review and meta-analysis of the literature[J]. Taiwan J Obstet Gynecol, 2018, 57(2): 181-189. DOI: 10.1016/j.tjog.2018.02.003. [13] Goetzinger KR, Tuuli MG, Cahill AG, et al. Development and validation of a risk factor scoring system for first-trimester prediction of preeclampsia[J]. Am J Perinatol, 2014, 31(12): 1049-1056. DOI: 10.1055/s-0034-1371705. [14] Bujold E, Roberge S, Lacasse Y, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis[J]. Obstet Gynecol, 2010, 116(2 Pt 1): 402-414. DOI: 10.1097/AOG.0b013e3181e9322a. -





 下载:
下载: