Comparison of prevalence and correlates of smoking between males with and without HIV-infection in Taizhou City
-
摘要:
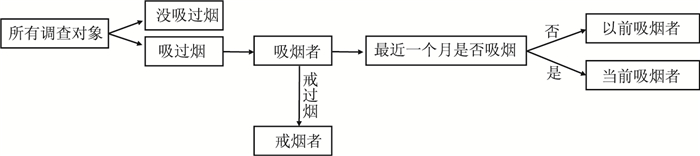
目的 比较台州市男性人类免疫缺陷病毒(human immunodeficiency virus,HIV)阳性者和HIV阴性者吸烟率并分析其影响因素,为台州市HIV阳性者有针对的制定和实施控烟措施提供依据。 方法 基于"HIV与衰老相关疾病前瞻性队列研究"的基线数据,收集人口学、吸烟相关特征等信息。最终纳入分析3 785名男性研究对象,应用SAS 9.4软件进行统计分析。 结果 男性HIV阳性者当前吸烟率为33.9%(95% CI:31.4%~36.5%),低于HIV阴性者(46.3%,95% CI:44.3%~48.3%);男性HIV阳性者以前吸烟率为14.1%(95% CI:12.3%~16.1%)略高于HIV阴性者(12.5%,95% CI:11.2%~13.9%),差异有统计学意义(χ2=56.81,P < 0.001)。男性HIV阳性者中,知晓感染后戒烟率为23.7%。使用多因素二分类Logistic回归模型分析显示,相较HIV阴性者,HIV阳性者当前吸烟的影响因素除职业、体重指数(body mass index,BMI)、日常锻炼以外,还包含年龄(40~岁,OR=1.87,95% CI:1.28~2.74,P=0.001;≥ 50岁,OR=2.30,95% CI:1.56~3.39,P < 0.001)、同性传播途径(OR=0.45,95% CI:0.35~0.59,P < 0.001)。 结论 台州市男性HIV阳性者目前吸烟状况仍然较普遍,且知晓HIV感染后曾尝试戒烟率较低。可通过加强男性HIV阳性者戒烟意识并结合影响当前吸烟的因素采取有针对性的措施控烟。 Abstract:Objective To analyze and compare the prevalence and correlates of smoking among HIV-infected and HIV-uninfected men in Taizhou City, and to provide this for the development and implementation of tobacco control measures for HIV-infected population. Methods We used baseline data from the ongoing prospective cohort study of Comparative HIV and Aging Research in Taizhou(CHART), China. 3 785 men were included in analysis. We collected basic characteristics, smoking behaviors, and so on. All analysis were performed using SAS 9.3. Results Compared to HIV-uninfected men, the prevalence of current smoking was lower(33.9%, 95% CI: 31.4%-36.5% versus 44.6%, 95%CI: 44.3%-48.3%) but prevalence of previous smoking was higher(14.1%, 95% CI: 12.3%-16.1% versus 12.5%, 95% CI: 11.2%-13.9%; χ2=56.81, P < 0.001). Among male HIV-positive people, the rate of smoking cessation after infection was 23.7%. Multivariate multinomial Logistic regression analysis showed that compared to HIV-uninfected men, in addition to occupation, body mass index and regular exercise that were associated with current smoking, older age(40-50years, OR=1.87, 95%CI: 1.28-2.74, P=0.001; ≥ 50 years, OR=2.30, 95% CI: 1.56-3.39, P < 0.001) and homosexual transmission(OR=0.45, 95% CI: 0.35-0.59, P < 0.001) were also associated with current smoking among HIV-infected men. Conclusions Cigarette smoking remains highly prevalent among HIV-infected men in Taizhou City, but with low self-reported smoking cessation rate even after knowing their HIV-positive status. Targeted measures can be taken to control tobacco by strengthening the awareness of HIV-positive persons to quit smoking and combining the factors affecting current smoking among HIV-infected population. -
Key words:
- Males /
- HIV-infected individuals /
- Smoking
-
表 1 不同特征的男性HIV阳性者和HIV阴性者的吸烟情况[例(比例)]
Table 1. Smoking status in different characteristics among HIV-infected and uninfected males [n(%)]
HIV阳性者 HIV阴性者 合计
(n=1 367)从不吸烟
(n=711)以前吸烟
(n=193)当前吸烟
(n=463)χ2/t值 P值 合计
(n=2 418)从不吸烟
(n=996)以前吸烟
(n=302)当前吸烟
(n=1 120)χ2/t值 P值 年龄(岁) 78.89 < 0.001 250.27 < 0.001 18~ 287 190(66.2) 20(7.0) 77(26.8) 543 312(57.5) 14(2.6) 217(39.9) 30~ 299 179(59.9) 27(9.0) 93(31.1) 582 250(42.9) 33(5.7) 299(51.4) 40~ 360 180(50.0) 48(13.3) 132(36.7) 542 198(36.5) 58(10.7) 286(52.8) ≥50 421 162(38.5) 98(23.3) 161(38.2) 751 236(31.4) 197(26.2) 318(42.4) 职业 24.17 < 0.001 49.02 < 0.001 农民/工人 850 430(50.6) 140(16.5) 280(32.9) 1314 486(37) 186(14.2) 642(48.9) 公务员/老师/职
员等45 36(80.0) 1(2.2) 8(17.8) 151 82(54.3) 12(8) 57(37.8) 未就业(家务/学
生/退休等)177 90(50.9) 23(13.0) 64(36.2) 369 182(49.3) 56(15.2) 131(35.5) 其他 295 155(52.5) 29(9.8) 111(37.6) 584 246(42.1) 48(8.2) 290(49.7) 文化程度 31.17 < 0.001 122.03 < 0.001 初中及以下 905 425(47.0) 152(16.8) 328(36.2) 1 478 487(32.9) 240(16.2) 751(50.9) 高中及以上 462 286(61.9) 41(8.9) 135(29.2) 940 509(54.2) 62(6.6) 369(39.3) 婚姻状况 37.72 < 0.001 85.29 < 0.001 单身 425 269(63.3) 34(8.0) 122(28.7) 599 653(38.1) 247(14.4) 814(47.5) 已婚 708 329(46.5) 125(17.7) 254(35.9) 1 714 323(53.9) 32(5.3) 244(40.7) 再婚/离异/丧偶 234 113(48.3) 34(14.5) 87(37.2) 105 20(19.1) 23(21.9) 62(59.1) BMI(kg/m2) 5.42 0.067 6.94 0.031 < 24 1040 531(51.1) 140(13.5) 369(35.5) 1 538 507(40.8) 136(11.0) 599(48.2) ≥24 327 180(55.1) 53(16.2) 94(28.8) 1 176 489(41.6) 166(14.1) 521(44.3) 腰围 0.41 0.813 13.16 0.001 正常 856 449(52.5) 117(13.7) 290(33.9) 1 378 578(41.9) 143(10.4) 657(47.7) 偏高(中心性肥胖) 511 262(51.3) 76(14.9) 173(33.9) 1 040 418(40.2) 159(15.3) 463(44.5) 日常锻炼 5.17 0.076 27.92 < 0.001 否 882 439(49.8) 128(14.5) 315(35.7) 1 660 638(38.4) 193(11.6) 829(49.9) 是 485 272(56.1) 65(13.4) 148(30.5) 758 358(47.2) 109(14.4) 291(38.4) 抑郁a(x±s) 13.8±4.4 13.8±4.5 13.7±4.3 13.9±4.4 0.24 0.887 11.4±3.1 11.1±3.0 11.7±3.0 11.6±3.2 30.90 < 0.001 HIV相关变量 - - HIV感染途径 92.15 < 0.001 异性传播及其他 808 336(41.6) 153(19.0) 319(39.4) - - - - 同性传播 559 375(67.1) 40(7.2) 144(25.8) - - - - 确诊HIV感染时间(年) 10.68 0.005 - - < 1 437 211(48.3) 81(18.5) 145(33.2) - - - - ≥1 930 500(53.8) 112(12.0) 318(34.2) - - - - cART时间(年) 1.97 0.113 - - 未知治疗 99 41(41.4) 16(16.2) 42(42.4) - - - - < 3 796 425(53.4) 118(14.8) 253(31.8) - - - - ≥3 472 245(51.9) 59(12.5) 168(35.6) - - - - 最近CD4细胞计数
(个/μl)b12.64 0.002 - - < 350 508 251(49.4) 94(18.5) 163(32.1) - - - - ≥350 856 460(53.7) 99(11.6) 297(34.7) - - - - 注:a缺失5人;b缺失3人。cART: combination antiretroviral therapy, 联合抗逆转录病毒治疗。 表 2 男性HIV阳性者以前和当前吸烟的单因素和多因素二分类Logistic回归分析
Table 2. Multinomial Logistic regression analysis of factors related to previous or current HIV-infected smokers
单因素 多因素a 以前吸烟 当前吸烟 以前吸烟 当前吸烟 cOR(95% CI)值 P值 cOR(95% CI)值 P值 cOR(95% CI)值 P值 cOR(95% CI)值 P值 年龄(岁) 18~ 1.00 1.00 1.00 1.00 30~ 1.43(0.78~2.65) 0.250 1.28(0.89~1.85) 0.182 1.45(0.77~2.74) 0.255 1.37(0.93~2.01) 0.115 40~ 2.53(1.45~4.44) 0.001 1.81(1.28~2.56) 0.001 2.14(1.18~3.89) 0.012 1.87(1.28~2.74) 0.001 ≥50 5.75(3.40~9.71) < 0.001 2.45(1.74~3.46) < 0.001 3.98(2.25~7.05) < 0.001 2.30(1.56~3.39) < 0.001 职业 农民/工人 1.00 1.00 1.00 1.00 公务员/老师/职员等 0.58(0.37~0.89) 0.014 1.10(0.83~1.47) 0.515 0.14(0.02~1.07) 0.058 0.47(0.21~1.05) 0.067 未就业(家务/学生/
退休等)0.79(0.48~1.29) 0.339 1.09(0.77~1.56) 0.626 1.25(0.74~2.14) 0.405 1.48(1.01~2.17) 0.042 其他 0.09(0.01~0.63) 0.016 0.34(0.16~0.75) 0.007 0.93(0.58~1.49) 0.765 1.41(1.04~1.92) 0.027 文化程度 初中及以下 1.00 1.00 - - 高中及以上 0.40(0.28~0.58) < 0.001 0.61(0.48~0.79) < 0.001 - - - - 婚姻状况 单身 0.33(0.22~0.50) < 0.001 0.59(0.45~0.77) < 0.001 - - - - 已婚 1.00 1.00 - - - - 再婚/离异/丧偶 0.79(0.51~1.22) 0.293 1.00(0.72~1.38) 0.987 - - - - BMI(kg/m2) < 24 1.00 1.00 1.00 1.00 ≥24 1.12(0.78~1.60) 0.546 0.75(0.57~1.00) 0.048 1.03(0.70~1.51) 0.882 0.64(0.48~0.86) 0.004 腰围 正常 1.00 1.00 偏高(中心性肥胖) 1.11(0.80~1.54) 0.520 1.02(0.80~1.30) 0.858 - - - - 日常锻炼 否 1.00 1.00 1.00 1.00 是 0.82(0.59~1.15) 0.244 0.76(0.59~0.97) 0.028 0.86(0.60~1.22) 0.392 0.75(0.58~0.97) 0.031 抑郁得分 0.99(0.96~1.03) 0.715 1.01(0.98~1.03) 0.720 - - - - HIV感染途径 异性传播及其他 1.00 1.00 1.00 1.00 同性传播 0.23(0.16~0.34) < 0.001 0.40(0.32~0.52) < 0.001 0.34(0.22~0.50) < .001 0.45(0.35~0.59) < 0.001 确诊HIV感染时间(年) < 1 1.00 1.00 1.00 1.00 ≥1 0.58(0.42~0.81) 0.001 0.93(0.72~1.19) 0.550 0.55(0.39~0.79) 0.001 0.84(0.64~1.10) 0.212 cART时间(年) <3 1.00 1.00 - - - - ≥3 0.84(0.59~1.18) 0.311 1.08(0.85~1.38) 0.522 - - - - 最近CD4细胞计数
(个/μl)< 350 1.00 1.00 1.00 1.00 ≥350 0.58(0.42~0.79) 0.001 0.99(0.78~1.27) 0.963 0.84(0.60~1.19) 0.337 1.22(0.94~1.59) 0.135 表 3 男性HIV阴性者以前和当前吸烟的单因素和多因素二分类Logistic回归分析
Table 3. Multinomial Logistic regression analysis of factors related to previous or current HIV-uninfected smokers
单因素 多因素a 以前吸烟 当前吸烟 以前吸烟 当前吸烟 cOR(95% CI)值 P值 cOR(95% CI)值 P值 cOR(95% CI)值 P值 cOR(95% CI)值 P值 年龄(岁) 18~ 1.00 1.00 1.00 1.00 30~ 2.94(1.54~5.62) 0.001 1.72(1.35~2.19) < 0.001 2.25(1.09~4.67) 0.029 1.15(0.84~1.56) 0.385 40~ 6.53(3.55~12.02) < 0.001 2.08(1.62~2.67) < 0.001 4.30(2.08~8.91) < .001 1.16(0.82~1.63) 0.396 ≥50 18.60(10.54~32.82) < 0.001 1.94(1.52~2.47) < 0.001 11.56(5.71~23.39) < .001 1.06(0.75~1.50) 0.729 职业 农民/工人 1.00 1.00 1.00 1.00 公务员/老师/职员等 0.51(0.36~0.73) < 0.001 0.89(0.73~1.10) 0.281 0.96(0.48~1.92) 0.904 0.82(0.56~1.19) 0.295 未就业(家务/学生/
退休等)0.80(0.57~1.13) 0.214 0.55(0.42~0.70) < 0.001 0.85(0.58~1.25) 0.403 0.68(0.52~0.89) 0.005 其他 0.38(0.20~0.72) 0.003 0.53(0.37~0.75) < 0.001 0.82(0.56~1.19) 0.289 1.06(0.85~1.32) 0.589 文化程度 初中及以下 1.00 1.00 1.00 1.00 高中及以上 0.25(0.18~0.34) < 0.001 0.47(0.39~0.56) < 0.001 0.69(0.47~1.01) 0.053 0.56(0.45~0.70) < 0.001 婚姻状况 单身 0.26(0.18~0.39) < 0.001 0.61(0.50~0.74) < 0.001 0.87(0.54~1.41) 0.570 0.89(0.68~1.16) 0.380 已婚 1.00 1.00 1.00 1.00 再婚/离异/丧偶 3.04(1.64~5.63) < 0.001 2.49(1.49~4.16) 0.001 2.54(1.34~4.81) 0.004 2.35(1.39~3.96) 0.001 BMI(kg/m2) < 24 1.00 1.00 1.00 1.00 ≥24 1.27(0.98~1.64) 0.074 0.90(0.76~1.07) 0.236 1.10(0.83~1.45) 0.509 0.82(0.69~0.99) 0.034 腰围 正常 1.00 1.00 - - 偏高(中心性肥胖) 1.54(1.19~1.99) 0.001 0.97(0.82~1.16) 0.770 - - 日常锻炼 否 1.00 1.00 1.00 1.00 是 1.01(0.77~1.32) 0.962 0.63(0.52~0.75) < 0.001 1.10(0.82~1.47) 0.541 0.74(0.61~0.90) 0.003 抑郁得分 1.07(1.02~1.11) 0.002 1.06(1.03~1.09) < 0.001 1.02(0.98~1.07) 0.350 1.04(1.01~1.07) 0.007 注:a单因素分析中P < 0.15的变量纳入多因素分析,采用倒退选择法以P < 0.10纳入多因素分析。cOR: Crude odds ratios, 粗比值比; aOR: adjusted odds ratio, 调整比值比; 95%CI: 95%confidence interval, 95%置信区间。 -
[1] Pacek LR, Crum RM. A review of the literature concerning HIV and cigarette smoking: morbidity and mortality, associations with individual-and social-level characteristics, and smoking cessation efforts[J]. Addict Res Theory, 2015, 23(1): 10-23. DOI: 10.3109/16066359.2014.920013. [2] Liang H, Chang L, Chen R, et al. Independent and combined effects of chronic HIV-infection and tobacco smoking on brain microstructure[J]. J Neuroimmune Pharmacol, 2018, 13(4): 509-522. DOI: 10.1007/s11481-018-9810-9. [3] Lifson AR, Neuhaus J, Arribas JR, et al. Smoking-related health risks among persons with HIV in the strategies for management of antiretroviral therapy clinical trial[J]. Am J Public Health, 2010, 100(10): 1896-1903. DOI: 10.2105/AJPH.2009.188664. [4] Petoumenos K, Worm S, Reiss P, et al. Rates of cardiovascular disease following smoking cessation in patients with HIV infection: Results from the D: A: D study(*)[J]. HIV Med, 2011, 12(7): 412-421. DOI: 10.1111/j.1468-1293.2010.00901.x. [5] Lewden C, Salmon D, Morlat P, et al. Causes of death among human immunodeficiency virus(HIV)-infected adults in the era of potent antiretroviral therapy: emerging role of hepatitis and cancers, persistent role of AIDS[J]. Int J Epidemiol, 2005, 34(1): 121-130. DOI: 10.1093/ije/dyh307. [6] Reddy KP, Kong CY, Hyle EP, et al. Lung cancer mortality associated with smoking and smoking cessation among people living with HIV in the United States[J]. JAMA Intern Med, 2017, 177(11): 1613-1621. DOI: 10.1001/jamainternmed.2017.4349. [7] 杨练, 黄云霞, 孙群, 等. 归因于吸烟的疾病间接经济负担测算研究: 基于全收入法[J]. 中国卫生经济, 2015, 34(12): 79-81. DOI: 10.7664/CHE20151224.Yang L, Huang YX, Sun Q, et al. Study on Estimating the indirect economic burden of tobacco-attribution: based on full income approach[J]. Chinese Health Economics, 2015, 34(12): 79-81. DOI: 10.7664/CHE20151224. [8] Altekruse SF, Shiels MS, Modur SP, et al. Cancer burden attributable to cigarette smoking among HIV-infected people in North America[J]. AIDS, 2018, 32(4): 513-521. DOI: 10.1097/QAD.0000000000001721. [9] Luo X, Duan S, Duan Q, et al. Tobacco use among HIV-infected individuals in a rural community in Yunnan Province, China[J]. Drug Alcohol Depend, 2014, 134: 144-150. DOI: 10.1016/j.drugalcdep.2013.09.023. [10] Qiao XT, Chen XX, Lin H J, et al. Sex differences in neurocognitive screening among adults living with HIV in China[J]. J Neurovirol, 2019. DOI:10.1007/s13365-019-00727-0. (inpress) [11] 乔晓彤, 陈潇潇, 林海江, 等. 男性HIV阳性者与HIV阴性对照者饮酒现状及其影响因素[J]. 中华流行病学杂志, 2019, 40(5): 493-498. DOI: 10.3760/cma.j.issn.0254-6450.2019.05.001.Qiao XT, Chen XX, Lin HJ, et al. Prevalence of alcohol use and related factors in HIV positive and HIV negative males[J]. Chin J Epidemiol, 2019, 40(5): 493-498. DOI: 10.3760/cma.j.issn.0254-6450.2019.05.001. [12] 肖瑛琦, 刘娅, 郑思琳, 等. 体质指数、腰围、腰臀比与社区中老年居民高血压关系研究[J]. 中华流行病学杂志, 2016, 37(9): 1223-1227. DOI: 10.3760/cma.j.issn.0254-6450.2016.09.008.Xiao YQ, Liu Y, Zheng SL, et al. Relationship between hypertension and body mass index, waist circumference and waist-hip ratio in middle-aged and elderly residents[J]. Chin J Epidemiol, 2016, 37(9): 1223-1227. DOI: 10.3760/cma.j.issn.0254-6450.2016.09.008. [13] 杨功焕, 马杰民, 刘娜, 等. 中国人群2002年吸烟和被动吸烟的现状调查[J]. 中华流行病学杂志, 2005, 26(2): 77-83. DOI: 10.3760/j.issn:0254-6450.2005.02.001.Yang GH, Ma JM, Liu N, et al. Smoking and passive smoking in Chinese[J]. Chin J Epidemiol, 2005, 26(2): 77-83. DOI: 10.3760/j.issn:0254-6450.2005.02.001. [14] Mdodo R, Frazier EL, Dube SR, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys[J]. Ann Intern Med, 2015, 162(5): 335-344. DOI: 10.7326/M14-0954. [15] Elf JL, Variava E, Chon S, et al. Prevalence and correlates of smoking among people living with HIV in south Africa[J]. Nicotine Tob Res, 2018, 20(9): 1124-1131. DOI: 10.1093/ntr/ntx145. [16] Yang T, Barnett R, Jiang S, et al. Gender balance and its impact on male and female smoking rates in Chinese cities[J]. Soc Sci Med, 2016, 154: 9-17. DOI: 10.1016/j.socscimed.2016.02.035. [17] Tesoriero JM, Gieryic SM, Carrascal A, et al. Smoking among HIV positive New Yorkers: prevalence, frequency, and opportunities for cessation[J]. AIDS Behav, 2010, 14(4): 824-835. DOI: 10.1007/s10461-008-9449-2. [18] Regan S, Meigs JB, Grinspoon SK, et al. Determinants of smoking and quitting in HIV-infected individuals[J]. PLoS One, 2016, 11(4): e153103. DOI: 10.1371/journal.pone.0153103. [19] Nguyen NP, Tran BX, Hwang LY, et al. Prevalence of cigarette smoking and associated factors in a large sample of HIV-positive patients receiving antiretroviral therapy in Vietnam[J]. PLoS One, 2015, 10(2): e118185. DOI: 10.1371/journal.pone.0118185. [20] Shirley DK, Kesari RK, Glesby MJ. Factors associated with smoking in HIV-infected patients and potential barriers to cessation[J]. AIDS Patient Care STDS, 2013, 27(11): 604-612. DOI: 10.1089/apc.2013.0128. -





 下载:
下载: