The effect of passive smoking during pregnancy on pregnancy complications and outcomes
-
摘要:
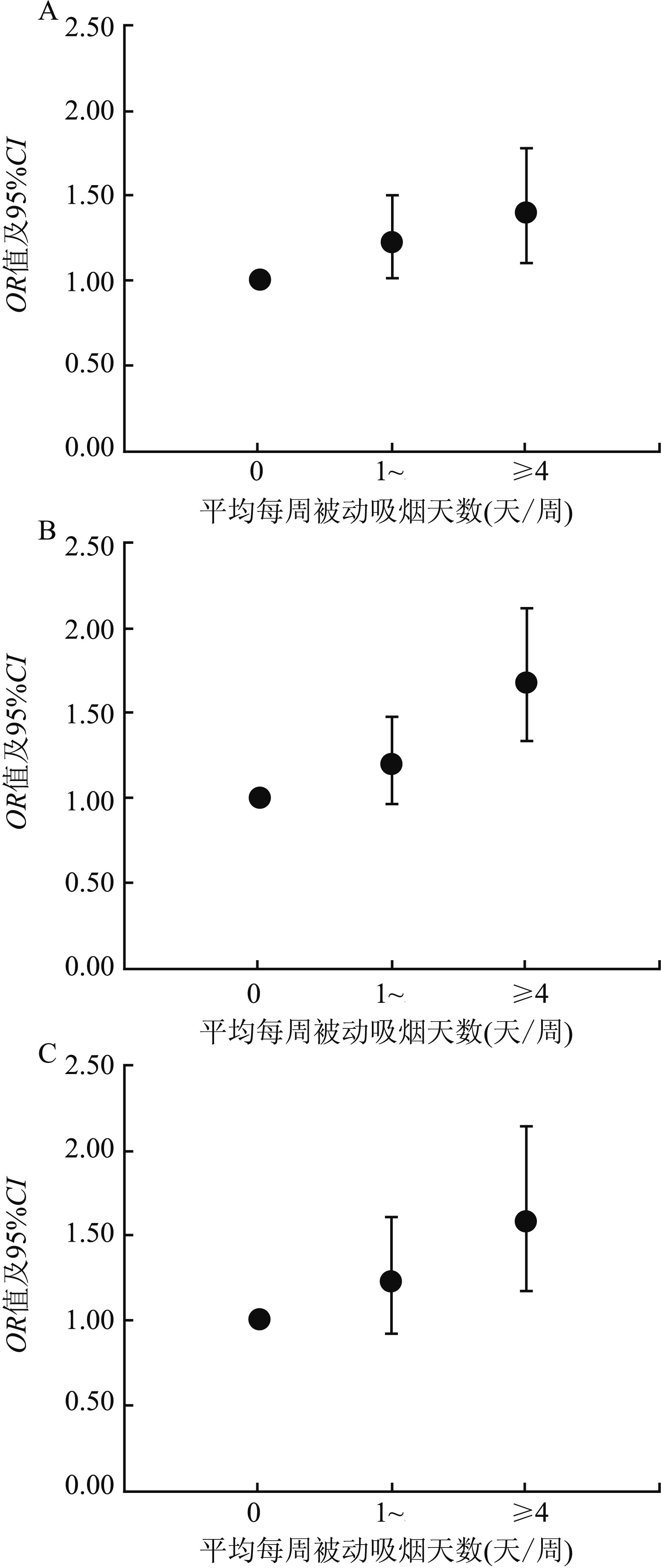
目的 了解孕期被动吸烟发生情况, 并探讨其对妊娠并发症及结局的影响。 方法 选取2012年4月-2013年3月在我国15家医疗保健机构分娩的8 926例单胎活产产妇作为研究对象, 使用自制调查问卷收集孕期被动吸烟发生情况、妊娠并发症和结局等信息, 采用单因素和多因素Logistic回归分析模型分析孕期被动吸烟对妊娠并发症及结局的影响。 结果 共1 801例产妇在孕期经历被动吸烟。控制混杂因素后, 孕期经历被动吸烟的产妇妊娠期糖尿病(gestational diabetes mellitus, GDM)的发生风险是非被动吸烟者的1.359倍(95%CI:1.146~1.612, P < 0.001), 胎膜早破的风险为1.290倍(95%CI:1.095~1.520, P=0.002), 早产的风险为1.367倍(95%CI:1.155~1.619, P < 0.001), 娩出低出生体重儿的风险为1.341倍(95%CI:1.079~1.668, P=0.008)。与非被动吸烟者相比, 平均每周被动吸烟天数≥4天者胎膜早破、早产和低出生体重儿的发生风险分别为非被动吸烟者的1.402倍(95%CI:1.104~1.780, P=0.006)、1.690倍(95%CI:1.339~2.132, P < 0.001)和1.584倍(95%CI:1.172~2.141, P=0.023)。 结论 被调查产妇孕期被动吸烟率较高, 孕期经历被动吸烟能够增加妊娠期糖尿病、胎膜早破、早产和低出生体重儿的发生风险。 Abstract:Objective To assess the prevalence of passive smoking during pregnancy, and toexplore the effect of passive smoking during pregnancy on pregnancy complications and outcomes. Methods A total of 8 926 postpartum women who delivered live singletons between April, 2012 to March, 2013 in 15 hospitals were enrolled. A self-made questionnaire was used to collect general information, occurrence of passive smoking during pregnancy, pregnancy complications and outcomes. Logistic regression models were used to analyze the effect of passive smoking during pregnancy on pregnancy complications and outcomes. Results A total of 1 801 women had experienced passive smoking during pregnancy. After adjusting for covariates, women who experienced passive smoking during pregnancy had an increased risk of gestational diabetes mellitus(OR=1.359, 95% CI:1.146-1.612, P < 0.001), premature rupture of membranes(OR=1.290, 95% CI:1.095-1.520, P=0.002), preterm birth(OR=1.367, 95% CI:1.155-1.619, P < 0.001), and delivering low birth weight infants(OR=1.341, 95% CI:1.079-1.668, P=0.008). Compared to those who did not experience passive smoking, women experienced passive smoking≥4 days/week had an increased risk of premature rupture of membranes(OR=1.402, 95% CI:1.104-1.780, P=0.006), preterm birth(OR=1.690, 95% CI:1.339-2.132, P < 0.001), and low birth weight(OR=1.584, 95% CI:1.172-2.141, P=0.023). Conclusions In this study, passive smoking during pregnancy is prevalent, and passive smoking during pregnancy may increase the risk of pregnancy outcomes like gestational diabetes mellitus, premature rupture of membranes, preterm birth and low birth weight. -
Key words:
- Passive smoking /
- Pregnancy /
- Pregnancy complications /
- Pregnancy outcomes
-
表 1 研究对象的一般人口学特征[n (%)]
Table 1. Characteristics of study participants[n (%)]
项目 被动吸烟组(n=1 801) 非被动吸烟组(n=7 125) χ2 /Z值 P值 分娩年龄(岁) 28(25, 30)a 28(26, 38) -3.412 < 0.001 分娩孕周 39(38, 40) 39(38, 40) -2.201 0.028 孕前体重指数(kg/m2) -3.062 0.002 < 24 408(22.7) 1 379(19.4) 24~ 1 182(65.6) 4 824(67.7) ≥28 211(11.7) 922(12.9) 文化程度 -4.639 < 0.001 大专及以下 1 270(70.5) 4 611(64.7) 本科及以上 531(29.5) 2 514(35.3) 职业 34.226 < 0.001 干部/职员/专业技术人员 890(49.4) 4 061(57.0) 工人/服务人员 252(14.0) 829(11.6) 无业 543(30.2) 1 870(26.3) 其他 116(6.4) 365(5.1) 家庭户平均月收入(元) -3.609 < 0.001 < 10 000 1 495(83.0) 5 643(79.2) ≥10 000 306(17.0) 1 482(20.8) 初产 7.856 0.005 否 371(20.6) 1 264(17.7) 是 1 430(79.4) 5 861(82.3) 孕期饮酒 127.528 < 0.001 否 1 684(93.5) 7 004(98.3) 是 117(6.5) 121(1.7) 注:a为M (P25, P75)。 表 2 孕期被动吸烟与妊娠并发症及结局关系的Logistic回归分析模型分析
Table 2. Logistic regression model analysis for passive smoking during pregnancy and pregnancy complications and outcomes
被动吸烟组[n (%)] 非被动吸烟组[n (%)] 调整前 调整后a OR(95%CI)值 P值 OR(95%CI)值 P值 妊娠期高血压疾病 94(5.2) 298(4.2) 1.262(0.995~1.600) 0.055 1.271(0.997~1.620) 0.053 子痫前期 44(2.4) 128(1.8) 1.370(0.969~1.937) 0.075 1.348(0.947~1.919) 0.097 妊娠期糖尿病 203(11.3) 651(9.1) 1.263(1.069~1.493) 0.006 1.359(1.146~1.612) < 0.001 前置胎盘 39(2.2) 146(2.1) 1.058(0.740~1.512) 0.757 1.013(0.705~1.455) 0.945 胎盘早剥 10(0.6) 25(0.4) 1.568(0.760~3.308) 0.219 1.493(0.703~3.170) 0.297 胎膜早破 217(12.1) 704(9.9) 1.250(1.063~1.469) 0.007 1.290(1.095~1.520) 0.002 羊水过多 54(3.0) 160(2.3) 1.346(0.984~1.840) 0.063 1.305(0.985~1.856) 0.062 羊水过少 74(4.1) 308(4.3) 0.948(0.732~1.229) 0.689 0.934(0.719~1.215) 0.613 早产 211(11.7) 602(8.5) 1.438(1.218~1.698) < 0.001 1.367(1.155~1.619) < 0.001 低出生体重儿b 120(6.7) 342(4.8) 1.416(1.142~1.755) 0.002 1.341(1.079~1.668) 0.008 巨大儿b 110(6.1) 472(6.6) 1.009(0.851~1.195) 0.919 0.966(0.776~1.203) 0.758 SGAb 130(7.2) 424(6.0) 1.230(1.003~1.507) 0.047 1.219(0.992~1.499) 0.060 LGAb 187(10.4) 734(10.3) 0.917(0.740~1.136) 0.428 1.035(0.871~1.230) 0.696 新生儿窒息b 33(1.8) 80(1.1) 1.644(1.092~2.474) 0.017 1.410(0.913~2.176) 0.121 注:a调整分娩年龄、孕前体质指数、文化程度、职业、家庭户平均月收入、初产、孕期饮酒; b进一步调整分娩孕周。 -
[1] Zhang L, Hsia J, Tu X, et al. Exposure to secondhand tobacco smoke and interventions among pregnant women in China: a systematic review[J]. Prev Chronic Dis, 2015, 12: E35. DOI: 10.5888/pcd12.140377. [2] 丁鹏, 陈维清.环境香烟烟雾对妊娠结局影响的研究现状[J].中山大学学报(医学科学版), 2009, 30(4S): 293-296. DOI: 10.3321/j.issn:1672-3554.2009.z2.083.Ding P, Chen WQ. Study on the effect of environmental tobacco smoke on pregnancy outcomes[J]. J Sun Yat-Sen Univ Med Sci, 2009, 30(4S): 293-296. DOI: 10.3321/j.issn:1672-3554.2009.z2.083. [3] Hoyt AT, Canfield MA, Romitti PA, et al. Does maternal exposure to secondhand tobacco smoke during pregnancy increase the risk for preterm or small-for-gestational age birth[J]. Matern Child Health J, 2018, 22(10): 1418-1429. DOI: 10.1007/s10995-018-2522-1. [4] Leng J, Wang P, Shao P, et al. Passive smoking increased risk of gestational diabetes mellitus independently and synergistically with prepregnancy obesity in Tianjin, China[J]. Diabetes Metab Res Rev, 2017, 33(3): e2861. DOI: 10.1002/dmrr.2861. [5] 郑保义.世界卫生组织关于吸烟行为调查的基本原则[J].中国健康教育, 1992, 8(5): 2-6. DOI: 10.16168/j.cnki.issn.1002-9982.1992.05.002.Zheng BY. Basic principles of the world health organization survey on smoking behavior[J]. Chin J Health Education, 1992, 8(5): 2-6. DOI: 10.16168/j.cnki.issn.1002-9982.1992.05.002. [6] Ishimitsu T. Starting the new review series: pregnancy-induced hypertension[J]. Hypertens Res, 2017, 40(1): 3-4. DOI: 10.1038/hr.2016.105. [7] 杨慧霞, 狄文.妇产科学[M].北京: 人民卫生出版社, 2016.Yang HX, Di W. Obstetrics and gynecology[M]. Beijing: People's Medical Publishing House, 2016. [8] 中华医学会妇产科学分会产科学组, 中华医学会围产医学分会妊娠合并糖尿病协作组.妊娠合并糖尿病诊治指南(2014)[J].中华妇产科杂志, 2014, 49(8): 561-569. DOI: 10.3760/cma.j.issn.0529-567x.2014.08.001.Obstetrics group of the Obstetrics branch of the Chinese Medical Association, Collaborative group of pregnancy and diabetes mellitus of the Perinatal Medicine branch of the Chinese Medical Association. Guidelines for diagnosis and treatment of gestational diabetes mellitus(2014)[J]. Chin J Obstetr Gynecol, 2014, 49(8): 561-569. DOI: 10.3760/cma.j.issn.0529-567x.2014.08.001. [9] 邵肖梅, 叶鸿瑁, 丘小汕.实用新生儿学[M].第四版.北京: 人民卫生出版社, 2011.Shao XM, Ye HM, Qiu XS. Practice of neonatology[M]. 4th ed. Beijing: People's Medical Publishing House, 2011. [10] Cupul-Uicab LA, Skjaerven R, Haug K, et al. In utero exposure to maternal tobacco smoke and subsequent obesity, hypertension, and gestational diabetes among women in the MoBa cohort[J]. Environ Health Perspect, 2012, 120(3): 355-360. DOI: 10.1289/ehp.1103789. [11] Terry PD, Weiderpass E, Ostenson CG, et al. Cigarette smoking and the risk of gestational and pregestational diabetes in two consecutive pregnancies[J]. Diabetes Care, 2003, 26(11): 2294-2298. DOI: 10.2337/diacare.26.11.2994. [12] 李朝平, 华红, 刘新, 等.被动吸烟对孕期生殖结局影响的研究[J].中国妇幼保健, 2004, (14): 30-32. DOI: 10.3969/j.issn.1001-4411.2004.20.015.Li CP, Wu QS, Hua H, et al. Study on the effect of passive smoking on pregnancy outcomes[J]. Maternal and Child Health Care of China, 2004, (14): 30-32. DOI: 10.3969/j.issn.1001-4411.2004.20.015. [13] 张爱英.孕妇被动吸烟对胎儿的影响研究[J].河南职工医学院学报, 2009, (4): 373-374. DOI: 10.3969/j.issn.1008-9276.2009.04.023.Zhang AY. Study on the effect of pregnancy passive smoking on fetuses[J]. Journal of Henan Medical College for Staff and Workers, 2009, (4): 373-374. DOI: 10.3969/j.issn.1008-9276.2009.04.023. [14] Qiu J, He X, Cui H, et al. Passive smoking and preterm birth in urban China[J]. Am J Epidemiol, 2014, 180(1): 94-102. DOI: 10.1093/aje/kwu092. [15] Cui H, Gong TT, Liu CX, et al. Associations between passive maternal smoking during pregnancy and preterm birth: evidence from a meta-analysis of observational studies[J]. PLoS One, 2016, 11(1): e0147848. DOI: 10.1371/journal.pone.0147848. [16] Andriani H, Kuo HW. Adverse effects of parental smoking during pregnancy in urban and rural areas[J]. BMC Pregnancy Childbirth, 2014, 14: 414. DOI: 10.1186/s12884-014-0414-y. [17] Huang SH, Weng KP, Huang SM, et al. The effects of maternal smoking exposure during pregnancy on postnatal outcomes: a cross sectional study[J]. J Chin Med Assoc, 2017, 80(12): 796-802. DOI: 10.1016/j.jcma.2017.01.007. [18] Owili PO, Muga MA, Kuo HW. Gender difference in the association between environmental tobacco smoke and birth weight in Africa[J]. Int J Environ Res Public Health, 2018, 15(7): 1409. DOI: 10.3390/ijerph15071409. [19] Lee J, Lee DR, Lee DH, et al. Influence of maternal environmental tobacco smoke exposure assessed by hair nicotine levels on birth weight[J]. Asian Pac J Cancer Prev, 2015, 16(7): 3029-3034. DOI: 10.7314/apjcp.2015.16.7.3029. [20] Ko TJ, Tsai LY, Chu LC, et al. Parental smoking during pregnancy and its association with low birth weight, small for gestational age, and preterm birth offspring: a birth cohort study[J]. Pediatr Neonatol, 2014, 55(1): 20-27. DOI: 10.1016/j.pedneo.2013.05.005. -





 下载:
下载: