Study on association between lipid levels and HCV infection in remunerated blood donation
-
摘要:
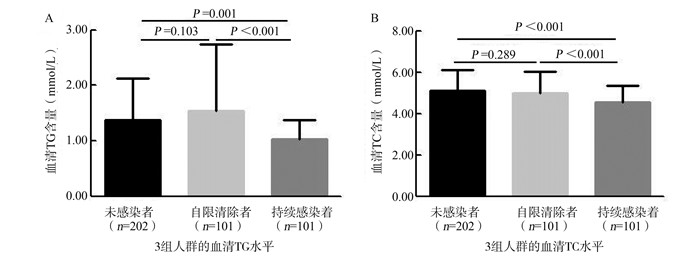
目的 探讨既往有偿献血地区丙型肝炎病毒(hepatitis C virus,HCV)感染与血脂的相关性及血脂异常的影响因素。 方法 2015年3月至5月对江苏省某地区>50周岁人群进行横断面调查,通过问卷调查获取一般人口学资料及既往献血史等信息,并采集5 ml空腹静脉血进行相关指标的检测;分析比较不同HCV感染状况血脂水平,并进行单因素、多因素逐步Logistic回归分析模型探索血脂异常的影响因素。 结果 共纳入1 537例研究对象,其中未感染者1 234例(80.3%),自限清除者117例(7.6%),持续感染者186例(12.1%)。倾向得分匹配后3组血清甘油三酯(triglyceride,TG)、总胆固醇(total cholesterol,TC)水平均存在统计学差异(均有P<0.05),且持续感染组血清TG和TC水平均低于其余两组。该地区血脂异常率为18.6%(286/1 537),多因素Logistic回归分析模型结果显示性别(OR=1.41,95% CI:1.06~1.87,P=0.018)、较高的空腹血糖(OR=2.54,95% CI:1.75~3.68,P<0.001)以及HCV持续感染者(OR=0.22,95% CI:0.12~0.41,P<0.001)是血脂异常发生的独立影响因素。 结论 江苏省既往有偿献血地区,持续感染者血清TG和TC水平均低于未感染者或自限清除者;HCV感染、性别及空腹血糖水平是该地区血脂异常的独立影响因素。 Abstract:Objective To explore the correlation between hepatitis C virus (HCV) infection and lipid, and determine the influencing factors of dyslipidemia in remunerated blood donation. Methods From March to May 2015, a cross-sectional study was conducted among people over 50 years old in Jiangsu Province. We obtained demographic data and related measurements through questionnaire surveys and blood test. We compared the lipid levels of different HCV infection groups. The influencing factors of dyslipidemia were explored by univariate and multivariate Logistic regression analysis. Results Of a total of 1 537 participants were included, of which 1 234 (80.3%) were uninfected HCV, 117 (7.6%) were HCV spontaneous clearance, and 186 (12.1%) were HCV persistent infection clients. Differences in serum TG and TC levels among the three groups after PSM were statistically significan (all P < 0.05), and those were lower in the participants with persistent infection than the other groups. Dyslipidemia occurred in 286 participants and the prevalence was 18.6%. Multivariate Logistic regression analysis showed that sex (OR=1.41, 95%CI: 1.06-1.87, P=0.018), higher fasting plasma glucose (OR=2.54, 95% CI: 1.75-3.68, P < 0.001) and HCV persistent infection (OR=0.22, 95% CI: 0.12-0.41, P < 0.001) were independent influencing factors for dyslipidemia. Conclusions The serum levels of TG and TC are lower in patients with persistent infection than those uninfected or with spontaneous clearance in remunerated blood donation. HCV infection, sex and fasting plasma glucose are related with dyslipidemia. -
Key words:
- Hepatitis C virus /
- Total cholesterol /
- Triglyceride /
- Influencing factors /
- Remunerated blood donation
-
表 1 研究对象一般人口学特征及部分血液检测结果[n(%)]
Table 1. General demographic characteristics and blood test results [n(%)]
变量 全人群 PSM后人群 未感染组 自限清除组 持续感染组 χ2值 P值 未感染组 自限清除组 持续感染组 χ2值 P值 性别 81.186 <0.001 3.037 0.219 男 516 (41.8) 10 (8.5) 34 (18.3) 18 (8.9) 7 (6.9) 14 (13.9) 女 718 (58.2) 107 (91.5) 152 (81.7) 184 (91.1) 94 (93.1) 87 (86.1) 年龄(岁) 16.452 <0.001 2.953 0.228 <60 434 (35.4) 63 (53.8) 75 (40.5) 115 (56.9) 53 (52.5) 47 (46.5) ≥60 793 (64.6) 54 (46.2) 110 (59.5) 87 (43.1) 48 (47.5) 54 (53.5) 文化程度 24.974 <0.001 0.057 0.972 小学及以下 734 (62.0) 86 (76.8) 134 (78.4) 156 (77.2) 79 (78.2) 79 (78.2) 小学以上 450 (38.0) 26 (23.2) 37 (21.6) 46 (22.8) 22 (21.8) 22 (21.8) 献全血史 397.562 <0.001 25.495 <0.001 无 1 129 (92.5) 44 (38.3) 86 (48.0) 139 (68.8) 41 (40.6) 49 (48.5) 有 92 (7.5) 71 (61.7) 93 (52.0) 63 (31.2) 60 (59.4) 52 (51.5) 献全血次数 5.173 0.075 0.573 0.751 <3 37 (43.5) 21 (32.8) 24 (27.3) 20 (31.7) 18 (30.0) 19 (36.5) ≥3 48 (56.5) 43 (67.2) 64 (72.7) 43 (68.3) 42 (70.0) 33 (63.5) 单采血浆史 617.873 <0.001 49.837 <0.001 无 1 053 (86.3) 15 (12.9) 27 (15.0) 97 (48.0) 15 (14.9) 16 (15.8) 有 167 (13.7) 101 (87.1) 153 (85.0) 105 (52.0) 86 (85.1) 85 (84.2) 单采血浆次数 12.094 0.002 11.670 0.003 <10 54 (32.5) 18 (18.6) 26 (17.2) 6 (5.7) 16 (18.6) 19 (22.4) ≥10 112 (67.5) 79 (81.4) 125 (82.8) 99 (94.3) 70 (81.4) 66 (77.6) ALT(IU/L) 454.230 <0.001 30.866 <0.001 ≤40 1 189 (96.4) 111 (94.9) 87 (46.8) 187 (92.6) 95 (94.1) 73 (72.3) >40 45 (3.6) 6 (5.1) 99 (53.2) 15 (7.4) 6 (5.9) 28 (27.7) AST(IU/L) 473.988 <0.001 19.601 <0.001 ≤40 1 206 (97.7) 113 (96.6) 96 (51.6) 193 (95.5) 97 (96.0) 83 (82.2) >40 28 (2.3) 4 (3.4) 90 (48.4) 9 (4.5) 4 (4.0) 18 (17.8) FPG(mmol/L) 6.543 0.038 0.663 0.718 <7.0 1 117 (90.5) 105 (89.7) 157 (84.4) 174 (86.1) 89 (88.1) 85 (84.2) ≥7.0 117 (9.5) 12 (10.3) 29 (15.6) 28 (13.9) 12 (11.9) 16 (15.8) 注:所有研究对象中,8人无年龄信息,70人无文化程度信息,22人无献全血史信息,41人无献全血次数信息,57人无单采血浆史信息,28人无单采血浆史次数信息。 表 2 既往有偿献血地区血脂异常影响因素分析
Table 2. Analysis of influencing factors of dyslipidemiain remunerated blood donation
变量 血脂异常
/正常β值 多因素分析 OR (95% CI)值 P值 性别 男 91/469 1.00 女 195/782 0.344 1.41 (1.06~1.87) 0.018 FPG(mmol/L) <7.0 235/1 144 1.00 ≥7.0 51/107 0.932 2.54 (1.75~3.68) <0.001 HCV感染状况 未感染组 249/985 1.00 自限清除组 26/91 0.020 1.02 (0.64~1.63) 0.937 持续感染组 11/175 -1.514 0.22 (0.12~0.41) <0.001 -
[1] Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study[J]. Lancet Gastroenterol Hepatol, 2017, 2(3):161-176. DOI: 10.1016/s2468-1253(16)30181-9. [2] Spearman CW, Dusheiko GM, Hellard M, et al. Hepatitis C[J]. Lancet, 2019, 394(10207):1451-1466. DOI: 10.1016/s0140-6736(19)32320-7. [3] 张标, 霍文哲.丙型肝炎病毒和肝细胞抗病毒机制相互作用的研究进展[J].中华疾病控制杂志, 2018, 22(3):302-307. DOI: 10.16462/j.cnki.zhjbkz.2018.03.020.Zhang B, Huo WZ. Advance in of research on interactions between hepatitis C virus and host cell-mediated antiviral mechanism[J]. Chin J Dis Control Prev, 2018, 22(3):302-307. DOI: 10.16462/j.cnki.zhjbkz.2018.03.020. [4] Meng Z, Liu Q, Sun F, et al. Hepatitis C virus nonstructural protein 5A perturbs lipid metabolism by modulating AMPK/SREBP-1c signaling[J]. Lipids Health Dis, 2019, 18(1):191. DOI: 10.1186/s12944-019-1136-y. [5] Negro F. Facts and fictions of HCV and comorbidities: steatosis, diabetes mellitus, and cardiovascular diseases[J]. J Hepatol, 2014, 61(Suppl 1):S69-78. DOI: 10.1016/j.jhep.2014.08.003. [6] Syed GH, Siddiqui A. Effects of hypolipidemic agent nordihydroguaiaretic acid on lipid droplets and hepatitis C virus[J]. Hepatology, 2011, 54(6):1936-1946. DOI: 10.1002/hep.24619. [7] 中国成人血脂异常防治指南修订联合委员会.中国成人血脂异常防治指南(2016年修订版)[J].中华健康管理学杂志, 2017, 11(1):7-28. DOI: 10.3760/cma.j.issn.1674-0815.2017.01.003.Joint Committee on the Revision of Guidelines for the Prevention and Treatment of Dyslipidemia in China. Guidelines for the prevention and control of dyslipidemia in China (2016 Revision)[J]. Chinese Journal of Health Management, 2017, 11(1):7-28. DOI: 10.3760/cma.j.issn.1674-0815.2017.01.003. [8] 程杨杨, 曹志, 侯洁, 等.中国中老年人群慢性病现状调查与共病关联分析[J].中华疾病控制杂志, 2019, 23(6):625-629. DOI: 10.16462/j.cnki.zhjbkz.2019.06.002.Cheng YY, Cao Z, Hou J, et al. Investigation and association analysis of multimorbidity in middle-aged and elderly population in China[J]. Chin J Dis Control Prev, 2019, 23(6): 625-629. DOI: 10.16462/j.cnki.zhjbkz.2019.06.002. [9] 顾景范. 《中国居民营养与慢性病状况报告(2015)》解读[J].营养学报, 2016, 38(6):525-529. DOI: 10.13325/j.cnki.acta.nutr.sin.2016.06.004.Gu JF. Interpretation of "Report on the Status of Nutrition and Chronic Diseases of Chinese Residents (2015)"[J]. Acta Nutrimenta Sinica, 2016, 38(6):525-529. DOI: 10.13325/j.cnki.acta.nutr.sin.2016.06.004. [10] 徐楚, 张平安.脂质代谢在HCV感染及生命周期中的作用[J].临床肝胆病杂志, 2019, 35(2):395-398. DOI: 10.3969/j.issn.1001-5256.2019.02.035.Xu C, Zhang PA. Research advances in the role of lipid metabolism in hepatitis C virus infection and life cycle[J]. J Clin Hepatol, 2019, 35(2):395-398. DOI: 10.3969/j.issn.1001-5256.2019.02.035. [11] Gao XF, Cui Q, Shi X, et al. Prevalence and trend of hepatitis C virus infection among blood donors in Chinese mainland: a systematic review and meta-analysis[J]. BMC Infect Dis, 2011, l1(1):88. DOI: 10.1186/1471-2334-11-88. [12] 陈明珠, 黄鹏, 陈红波, 等.江苏某地区既往有偿献血人群HCV感染状况及相关因素研究[J].中华流行病学杂志, 2016, 37(5):653-657. DOI: 10.3760/cma.j.issn.0254-6450.2016.05.013.Chen MZ, Huang P, Chen HB, et al. HCV infection status and risk factors in remunerated blood donors in Jiangsu province[J]. Chin J Epidemiol, 2016, 37(5):653-657. DOI: 10.3760/cma.j.issn.0254-6450.2016.05.013. [13] 中华医学会肝病学分会; 中华医学会感染病学分会.丙型肝炎防治指南(2019年版)[J].临床肝胆病杂志, 2019, 35(12):2670-2686. DOI: 10.3760/cma.j.issn.1000-6680.2020.01.004.Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for the prevention and treatment of hepatitis C(2019 version)[J]. J Clin Hepatol, 2019, 35(12):2670-2686. DOI: 10.3760/cma.j.issn.1000-6680.2020.01.004. [14] Narindrarangkura P, Bosl W, Rangsin R, et al. Prevalence of dyslipidemia associated with complications in diabetic patients: a nationwide study in Thailand[J]. Lipids Health Dis, 2019, 18(1):90. DOI: 10.1186/s12944-019-1034-3. [15] Rubin DB, Thomas N. Matching using estimated propensity scores: relating theory to practice[J]. Biometrics, 1996, 52(1):249-264. DOI: 10.2307/2533160. [16] Benedetto U, Head SJ, Angelini GD, et al. Statistical primer: propensity score matching and its alternatives[J]. Eur J Cardiothorac Surg, 2018, 53(6):1112-1117. DOI: 10.1093/ejcts/ezy167. [17] Arain SQ, Talpur FN, Channa NA. A comparative study of serum lipid contents in pre and post IFN-alpha treated acute hepatitis C patients[J]. Lipids Health Dis, 2015, 14:117. DOI: 10.1186/s12944-015-0119-x. [18] 徐楚, 张平安. HCV对脂代谢相关指标表达的影响[J].临床肝胆病杂志, 2019, 35(5):987-991. DOI: 10.3969/j.issn.1001-5256.2019.05.011.Xu C, Zhang PA. Influence of hepatitis C virus on the expression of lipid metabolism indices[J]. J Clin Hepatol, 2019, 35(5):987-991. DOI: 10.3969/j.issn.1001-5256.2019.05.011. [19] Sun HY, Cheng PN, Tseng CY, et al. Favouring modulation of circulating lipoproteins and lipid loading capacity by direct antiviral agents grazoprevir/elbasvir or ledipasvir/sofosbuvir treatment against chronic HCV infection[J]. Gut, 2018, 67(7):1342-1350. DOI: 10.1136/gutjnl-2017-313832. [20] Wang CC, Cheng PN, Kao JH. Systematic review: chronic viral hepatitis and metabolic derangement[J]. Aliment Pharmacol Ther, 2020, 51(2):216-230. DOI: 10.1111/apt.15575. [21] 宋培新, 李雷, 陶月, 等.丙型肝炎病毒感染者病毒载量与血脂代谢指标的相关性分析[J].实用临床医药杂志, 2015, 19(11):32-35. DOI: 10.7619/jcmp.201511010.Song PX, Li L, Tao Y, et al. Analysis in correlation between serum hepatitis C virus load and lipid metabolic components in chronic hepatitis C patients[J]. Journal of Clinical Medicine in Practice, 2015, 19(11):32-35. DOI: 10.7619/jcmp.201511010. [22] 刘梅林, 胡大一, 韩雅玲, 等.绝经后女性血脂异常管理的中国专家共识[J].中华心血管病杂志, 2014, 42(4):279-283. DOI: 10.3969/j.issn.1000-3614.2014.z2.027.Liu ML, Hu DY, Han YL, et al. Consensus of Chinese experts on management of dyslipidemia in postmenopausal women[J]. Chin J Cardiol, 2014, 42(4):279-283. DOI: 10.3969/j.issn.1000-3614.2014.z2.027. [23] Qi L, Ding X, Tang W, et al. Prevalence and risk factors associated with dyslipidemia in Chongqing, China[J]. Int J Environ Res Public Health, 2015, 12(10):13455-13465. DOI: 10.3390/ijerph121013455. -





 下载:
下载: