-
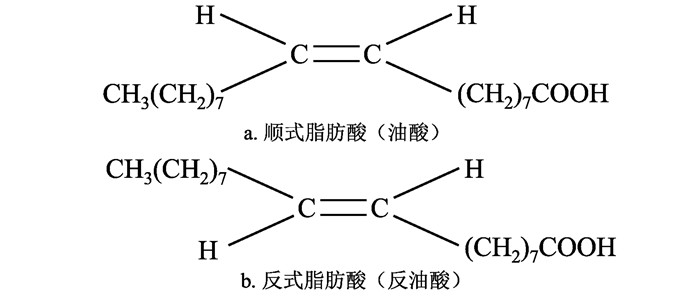
摘要: 随着膳食模式的改变,主要存在于加工食品中的膳食反式脂肪酸(trans fatty acid,TFA)通过饮食摄入在身体中慢慢累积。在国外很早就有学者研究TFA的种类、来源、结构以及对疾病的影响,但是在国内TFA对疾病的危害还没有引起足够的重视。本文就近几年TFA对肥胖、心血管疾病、糖尿病、非酒精性脂肪肝、癌症等慢性非传染性疾病(简称慢性病)的危害及作用机制做讨论,为疾病预防和治疗、营养膳食指导、工业生产优化等方面提供参考依据。Abstract: With the change of dietary patterns, dietary trans fatty acids (TFA), which mainly presents in processed foods, accumulates slowly in the body through dietary intake. Scholars have studied the types, sources, structures, and effects of TFA on diseases very early in foreign countries, but the harm of TFA to diseases in China has not attracted enough attention. This article discusses the harm and mechanism of TFA in recent years on obesity, cardiovascular disease, diabetes, non-alcoholic fatty liver, cancer and other chronic diseases, and provides reference for disease prevention and treatment, nutrition and diet guidance, as well as industrial production optimization.
-
Key words:
- Trans fatty acids /
- Obesity /
- Cardiovascular disease /
- Diabetes /
- Non-alcoholic liver disease /
- Cancer
-
表 1 日常膳食中常见的反式脂肪酸种类
Table 1. Classification of common trans fatty acids in diets
中文名 英文名 分子简式 反棕榈酸 Trans palmitoleic acid C16:1 9t 反油酸 Elaidic acid(EA) C18:1 9t 反-10-十八碳烯酸 Trans-10-octadecenoic acid C18:1 10t 反异油酸 Trans vaccenic acid (TVA) C18:1 11t 瘤胃酸 Rumenic acid C18:2 9c, 11t 反亚油酸 Trans, trans-9, 12-octadecadienoic acid C18:2 9t, 12t -
[1] 张嘉峻, 单淑晴, 许莎莎, 等.反式脂肪酸(TFA)与慢性代谢性疾病关系的研究进展[J].卫生软科学, 2017, 31(2):31-34. DOI: 10.3969/j.issn.1003-2800.2017.02.008.Zhang JJ, Shan SQ, Xu SS, et al. Study on the progress of the relationship between trans-fatty acids and chronic metabolic disease[J]. Soft Science of Health, 2017, 31(2):31-34. DOI: 10.3969/j.issn.1003-2800.2017.02.008. [2] González-Becerra K, Ramos-Lopez O, Barrón-Cabrera E, et al. Fatty acids, epigenetic mechanisms and chronic diseases: a systematic review[J]. Lipids Health Dis, 2019, 18(1):178. DOI: 10.1186/s12944-019-1120-6. [3] Blüher M. Obesity: global epidemiology and pathogenesis[J]. Nat Rev Endocrinol, 2019, 15(5):288-298. DOI: 10.1038/s41574-019-0176-8. [4] Chajès V, Biessy C, Ferrari P, et al. Plasma elaidic acid level as biomarker of industrial trans fatty acids and risk of weight change: report from the EPIC study[J]. PLoS One, 2015, 10(2):e0118206. DOI: 10.1371/journal.pone.0118206. [5] Rashidi AA, Heidari Bakavoli AR, Avan A, et al. Dietary intake and its relationship to different body mass index categories: a population-based study[J]. J Res Health Sci, 2018, 18(4):e00426. [6] Koochakpour G, Esfandiar Z, Hosseini-Esfahani F, et al. Evaluating the interaction of common FTO genetic variants, added sugar, and trans-fatty acid intakes in altering obesity phenotypes[J]. Nutr Metab Cardiovasc Dis, 2019, 29(5):474-480. DOI: 10.1016/j.numecd.2019.01.005. [7] Hansen CP, Berentzen TL, Østergaard JN, et al. Adipose tissue trans-fatty acids and changes in body weight and waist circumference[J]. Br J Nutr, 2014, 111(7):1283-1291. DOI: 10.1017/S0007114513003747. [8] Zhao X, Shen C, Zhu H, et al. Trans-fatty acids aggravate obesity, insulin resistance and hepatic steatosis in C57BL/6 mice, possibly by suppressing the IRS1 dependent pathway[J]. Molecules, 2016, 21(6):705. DOI: 10.3390/molecules21060705. [9] Qiu B, Wang Q, Du FL, et al. Comparative proteomics analysis reveals trans fatty acid isomers activates different pathways in human umbilical vein endothelial cell[J]. Lipids, 2018, 53(2):189-203. DOI: 10.1002/lipd.12015. [10] Zhu W, Niu X, Wang M, et al. Endoplasmic reticulum stress may be involved in insulin resistance and lipid metabolism disorders of the white adipose tissues induced by high-fat diet containing industrial trans-fatty acids[J]. Diabetes Metab Syndr Obes, 2019, 12:1625-1638. DOI: 10.2147/DMSO.S218336. [11] Zhuang P, Zhang Y, He W, et al. Dietary fats in relation to total and cause-specific mortality in a prospective cohort of 521120 individuals with 16 years of follow-up[J]. Circ Res, 2019, 124(5):757-768. DOI: 10.1161/CIRCRESAHA.118.314038. [12] De Souza RJ, Mente A, Maroleanu A, et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies[J]. BMJ, 2015, 351:h3978. DOI: 10.1136/bmj.h3978. [13] Shah B, Thadani U. Trans fatty acids linked to myocardial infarction and stroke: what is the evidence?[J]. Trends Cardiovasc Med, 2019, 29(5):306-310. DOI: 10.1016/j.tcm.2018.09.011. [14] Herreras Z, Cofán M, Catalan M, et al. The proportion of total C18:1 trans-fatty acids in red blood cell membranes relates to carotid plaque prevalence[J]. J Nutr Biochem, 2016, 38:81-85. DOI: 10.1016/j.jnutbio.2016.08.004. [15] Takeuchi H, Futatsuya C, Miki A, et al. Supplementation with trans fatty acid at 1% energy did not increase serum cholesterol irrespective of the obesity-related genotypes in healthy adult Japanese[J]. Asia Pac J Clin Nutr, 2018, 27(4):797-803. DOI: 10.6133/apjcn.112017.04. [16] Restrepo BJ, Rieger M. Trans fat and cardiovascular disease mortality: evidence from bans in restaurants in New York[J]. J Health Econ, 2016, 45:176-196. DOI: 10.1016/j.jhealeco.2015.09.005. [17] Hirata Y, Takahashi M, Kudoh Y, et al. Trans-fatty acids promote proinflammatory signaling and cell death by stimulating the apoptosis signal-regulating kinase 1 (ASK1)-p38 pathway[J]. J Biol Chem, 2017, 292(20):8174-8185. DOI: 10.1074/jbc.M116.771519. [18] 刘展. PPARα/PGC1-α/AKT信号通路在低剂量TFA对大鼠心肌组织损伤中的作用[D].石家庄: 河北医科大学, 2017.Liu Z. Effect of low-dose TFA on PPARα/PGC1-α/AKT signaling pathway in rat heart[D]. Shijiazhuang: Hebei Medical University, 2017. [19] 谢上才, 江力勤.反式脂肪酸对心血管的危害及机制的研究进展[J].心脑血管病防治, 2016, 16(2):134-135, 139. DOI: 10.3969/j.issn.1009-816x.2016.02.19.Xie SC, Jiang LQ. Advances in the study of the harm and mechanism of trans fatty acids to cardiovascular disease[J]. Prevention and Treatment of Cardio-Cerebral-Vascular Disease, 2016, 16(2):134-135, 139. DOI: 10.3969/j.issn.1009-816x.2016.02.19. [20] 黄忱, 谢佳格, 季敏燕, 等.番茄红素对反式脂肪酸致小鼠心血管毒作用的影响[J].食品安全导刊, 2017(6):140-142. DOI: 10.16043/j.cnki.cfs.2017.06.096.Huang S, Xie JG, Ji MY, et al. Effect of lycopene on cardiovascular toxicity in mice with trans fatty acids[J]. China Food Safety, 2017(6):140-142. DOI: 10.16043/j.cnki.cfs.2017.06.096. [21] 王友良, 甘功友, 张冬初, 等.原花青素对反式脂肪酸致小鼠心血管损害的修复作用[J].食品安全导刊, 2019(18):168-170. DOI: 10.16043/j.cnki.cfs.2019.18.119.Wang YL, Gan GY, Zhang DC, et al. Effects of proanthocyanins on the repair of cardiovascular damage induced by trans fatty acids in mice[J]. China Food Safety, 2019(18):168-170. DOI: 10.16043/j.cnki.cfs.2019.18.119. [22] Mazidi M, Katsiki N, Mikhailidis DP, et al. Link between plasma trans-fatty acid and fatty liver is moderated by adiposity[J]. Int J Cardiol, 2018, 272:316-322. DOI: 10.1016/j.ijcard.2018.07.061. [23] Oteng AB, Loregger A, van Weeghel M, et al. Industrial trans fatty acids stimulate SREBP2-mediated cholesterogenesis and promote non-alcoholic fatty liver disease[J]. Mol Nutr Food Res, 2019, 63(19):e1900385. DOI: 10.1002/mnfr.201900385. [24] Jeyapal S, Putcha UK, Mullapudi VS, et al. Chronic consumption of fructose in combination with trans fatty acids but not with saturated fatty acids induces nonalcoholic steatohepatitis with fibrosis in rats[J]. Eur J Nutr, 2018, 57(6):2171-2187. DOI: 10.1007/s00394-017-1492-1. [25] Mazidi M, Katsiki N, Mikhailidis DP, et al. Link between plasma trans-fatty acid and fatty liver is moderated by adiposity[J]. Int J Cardiol, 2018, 272:316-322. DOI: 10.1016/j.ijcard.2018.07.061. [26] Ma RCW. Epidemiology of diabetes and diabetic complications in China[J]. Diabetologia, 2018, 61(6):1249-1260. DOI: 10.1007/s00125-018-4557-7. [27] Thompson AK, Minihane AM, Williams CM. Trans fatty acids, insulin resistance and diabetes[J]. Eur J Clin Nutr, 2011, 65(5):553-564. DOI: 10.1038/ejcn.2010.240. [28] 王淑娥, 孔正桥, 姜迎, 等.糖尿病与反式脂肪酸研究进展[J].中国公共卫生, 2019, 35(7):926-928. DOI: 10.11847/zgggws1120199.Wang SE, Kong ZQ, Jiang Y, et al. Relationship between trans-fatty acids and diabetes: a review[J]. Chin Publ Heal, 2019, 35(7):926-928. DOI: 10.11847/zgggws1120199. [29] Liu B, Sun Y, Snetselaar LG, et al. Association between plasma trans-fatty acid concentrations and diabetes in a nationally representative sample of US adults[J]. J Diabetes, 2018, 10(8):653-664. DOI: 10.1111/1753-0407.12652. [30] Wang Q, Imamura F, Ma W, et al. Circulating and dietary trans fatty acids and incident type 2 diabetes in older adults: the Cardiovascular Health Study[J]. Diabetes Care, 2015, 38(6):1099-1107. DOI: 10.2337/dc14-2101. [31] Tremblay BL, Rudkowska I. Nutrigenomic point of view on effects and mechanisms of action of ruminant trans fatty acids on insulin resistance and type 2 diabetes[J]. Nutr Rev, 2017, 75(3):214-223. DOI: 10.1093/nutrit/nuw066. [32] Imamura F, Fretts A, Marklund M, et al. Fatty acid biomarkers of dairy fat consumption and incidence of type 2 diabetes: a pooled analysis of prospective cohort studies[J]. PLoS Med, 2018, 15(10):e1002670. DOI: 10.1371/journal.pmed.1002670. [33] Wang X, Gupta J, Kerslake M, et al. Trans-11 vaccenic acid improves insulin secretion in models of type 2 diabetes in vivo and in vitro[J]. Mol Nutr Food Res, 2016, 60(4):846-857. DOI: 10.1002/mnfr.201500783. [34] Liss MA, Al-Bayati O, Gelfond J, et al. Higher baseline dietary fat and fatty acid intake is associated with increased risk of incident prostate cancer in the SABOR study[J]. Prostate Cancer Prostatic Dis, 2019, 22(2):244-251. DOI: 10.1038/s41391-018-0105-2. [35] Anjom-Shoae J, Sadeghi O, Larijani B, et al. Dietary intake and serum levels of trans fatty acids and risk of breast cancer: a systematic review and dose-response meta-analysis of prospective studies[J]. Clin Nutr, 2020, 39(3):755-764. DOI: 10.1016/j.clnu.2019.03.024. [36] Chajès V, Assi N, Biessy C, et al. A prospective evaluation of plasma phospholipid fatty acids and breast cancer risk in the EPIC study[J]. Ann Oncol, 2017, 28(11):2836-2842. DOI: 10.1093/annonc/mdx482. [37] Bertrand KA, Giovannucci E, Rosner BA, et al. Dietary fat intake and risk of non-Hodgkin lymphoma in 2 large prospective cohorts[J]. Am J Clin Nutr, 2017, 106(2):650-656. DOI: 10.3945/ajcn.117.155010. [38] Barcelos RC, Vey LT, Segat HJ, et al. Cross-generational trans fat intake exacerbates UV radiation-induced damage in rat skin[J]. Food Chem Toxicol, 2014, 69:38-45. DOI: 10.1016/j.fct.2014.03.031. [39] Ohmori H, Fujii K, Kadochi Y, et al. Elaidic acid, a trans-fatty acid, enhances the metastasis of colorectal cancer cells[J]. Pathobiology, 2017, 84(3):144-151. DOI: 10.1159/000449205. [40] Hu X, Wang X, Jia F, et al. A trans-fatty acid-rich diet promotes liver tumorigenesis in HCV core gene transgenic mice[J]. Carcinogenesis, 2020, 41(2):159-170. DOI: 10.1093/carcin/bgz132. [41] Ginter E, Simko V. New data on harmful effects of trans-fatty acids[J]. Bratisl Lek Listy, 2016, 117(5):251-253. DOI: 10.4149/bll_2016_048. [42] 秦书琪, 麻微微.反式脂肪酸与老年痴呆症发病相关性的研究进展[J].卫生研究, 2015, 44(1):143-146. DOI: 10.19813/j.cnki.weishengyanjiu.2015.01.038.Qin SQ, Ma WW. The research progress of the association between trans fatty acids and alzheimer's disease[J]. J Hygiene Res, 2015, 44(1):143-146. DOI: 10.19813/j.cnki.weishengyanjiu.2015.01.038. [43] Çekici H, Akdevelio lu Y. The association between trans fatty acids, infertility and fetal life: a review[J]. Hum Fertil (Camb), 2019, 22(3):154-163. DOI: 10.1080/14647273.2018.1432078. [44] 齐磊, 李刚, 李洪龙, 等.孕哺期至成年反式脂肪酸摄入对小鼠学习记忆能力的影响[J].环境与健康杂志, 2019, 36(3):210-213. DOI: 10.16241/j.cnki.1001-5914.2019.03.006.Qi L, Li G, Li HL, et al. Effects of intake of trans fatty acids on memory and learning among offspring mice during gestation, lactation and adulthood[J]. J Environment Health, 2019, 36(3):210-213. DOI: 10.16241/j.cnki.1001-5914.2019.03.006. [45] 杨月欣.中国食物成分表[M].第2版.北京:北京大学医学出版社, 2009.Yang YX. China Food Composition[M]. 2nd ed. Beijing: Peking University Medical Press, 2009. [46] 韩文静, 从仁怀, 陈鹏, 等.膳食脂肪酸与心血管疾病关系的研究进展[J].中国食物与营养, 2017, 23(5):63-68. DOI: 10.3969/j.issn.1006-9577.2017.05.015.Han WJ, Cong RH, Chen P, et al. Effects of dietary fatty acid on cardiovascular disease[J]. Food and Nutrition in China, 2017, 23(5):63-68. DOI: 10.3969/j.issn.1006-9577.2017.05.015. -





 下载:
下载: