Interaction effcet of percutaneous coronary intervention and frailty on poor prognosis among elderly patients with coronary heart disease
-
摘要:
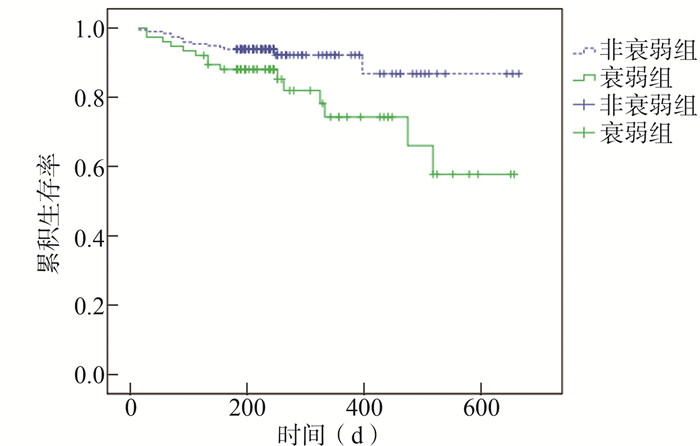
目的 探讨经皮冠状动脉介入治疗(percutaneous coronary intervention, PCI)和衰弱对老年冠心病患者近期死亡率以及心源性再住院率的交互作用。 方法 选取池州市人民医院2018年4月1日至2019年11月30日期间在心血管内科住院的老年冠心病患者作为研究对象,收集患者的临床资料,使用衰弱量表对每位患者进行衰弱评估。随访患者出院后的全因死亡情况和心源性再住院情况。采用Kaplan-Meier法生存分析、χ2检验、t检验进行数据分析。 结果 共计273例住院老年冠心病患者纳入研究,76例符合衰弱标准,占比27.84%,160例行PCI,占比58.61%。衰弱相对于非衰弱发生死亡的比例增大到2.77(95% CI:1.41~7.04)倍、发生全因死亡/心源性再住院增大到2.73(95% CI:1.90~3.93)倍。其中,在PCI患者中,衰弱相对于非衰弱组发生死亡和全因死亡/心源性再住院的RR值分别增加到3.02(95% CI:1.32~6.93)和2.96(95% CI:1.89~4.62)。Kaplan-Meier法生存分析的结果显示,衰弱组患者随访期间全因死亡率、全因死亡/心源性再住院率高于非衰弱组(均有P<0.05)。然而,在非PCI患者中,衰弱组患者随访期间全因死亡率与非衰弱组的差异无统计学意义(χ2=1.95, P=0.163)。 结论 PCI增加了衰弱对老年冠心病患者的近期不良预后的发生风险,PCI与衰弱对老年冠心病患者的不良预后可能存在交互作用。 Abstract:Objective To investigate the interaction effect of percutaneous coronary intervention (PCI) and frailty on the short-term mortality and cardiogenic readmission rates in elderly patients with coronary heart disease (CHD). Methods From April 1, 2018 to November 30, 2019, the elderly patients with CHD were selected as the research objects, who were hospitalized in the Department of Cardiology of Chizhou people's hospital. The clinical data of the patients were collected. The frailty of each patient was evaluated with the frail scale. All-cause death and cardiogenic readmission after discharge were followed up. Kaplan-Meier method, Chi-square test, and t-test were used to analyze the data. Results A total of 273 hospitalized elderly patients with CHD were included in the study. 76 (27.84%) of them met the fattening criteria. 160 (58.61%) of them received PCI. The incidence of death due to frailty among frailly patients increased to 2.77 (95% CI: 1.41-7.04) times higher than that among non-frailly patients. The incidence of all-cause death/cardiogenic readmission among frailly patients increased to 2.73 (95% CI: 1.90-3.93) times higher than that among non-frailly patients. Among patients treated with PCI, the RR for death and all-cause death / cardiogenic readmission in the frailty group increased to 3.02 (95% CI: 1.32-6.93) and 2.96 (95% CI: 1.89-4.62) times higher than those in the non-frailty group respectively. The results of Kaplan-Meier survival analysis showed that all-cause mortality and all-cause death / cardiogenic readmission rates were significantly higher in the frail group than that in the non-frail group (all P < 0.05). However, among patients without PCI, there was no significant difference in all-cause mortality between the frailty group and the non-Frailty group (χ2=1.95, P=0.163). Conclusion PCI increases the risk of poor short-term prognosis in frailly elderly patients with CHD, and there may be an interact effect of PCI and frailty on the poor prognosis in elderly patients with CHD. -
Key words:
- Coronary heart disease /
- Frailty /
- FRAIL Scale /
- Prognosis
-
表 1 2018年4月1日-2019年11月30日池州市人民医院纳入的冠心病患者基本资料[n(%)]
Table 1. Basic data of CHD patients enrolled in Chizhou People's Hospital from April 1, 2018 to November 30, 2019 [n(%)]
项目 非衰弱(n=197) 衰弱(n=76) t/χ2值 P值 年龄(x±s, 岁) 72.22±5.28 73.75±5.53 2.118 0.035 BMI(x±s, kg/m2) 24.22±3.38 23.86±4.08 -0.743 0.458 男性 120(60.91) 42(55.26) 0.726 0.394 吸烟 58(29.44) 25(32.89) 0.309 0.578 PCI 117(59.39) 43(56.58) 0.179 0.672 高血压 120(60.91) 41(53.95) 1.100 0.294 心力衰竭 50(25.38) 26(34.21) 2.129 0.145 心房颤动 65(32.99) 27(35.53) 0.157 0.692 糖尿病 52(26.40) 22(28.95) 0.181 0.671 高脂血症 58(29.44) 21(27.63) 0.087 0.768 慢性肾脏疾病 45(22.84) 18(23.68) 0.022 0.882 贫血 31(15.74) 28(36.84) 14.421 < 0.001 脑血管病 50(25.38) 21(27.63) 0.144 0.704 慢性阻塞性肺疾病 58(29.44) 28(36.84) 1.392 0.238 表 2 两组老年冠心病患者生化检查指标比较(x±s)
Table 2. Comparison of biochemical parameters in two groups of elderly patients with coronary heart disease (x±s)
项目 非衰弱(n=197) 衰弱组(n=76) t/χ2值 P值 氮末端脑钠肽前体(lg pg/ml) 3.18±0.48 3.26±0.53 1.198 0.232 白蛋白(g/L) 40.21±3.59 37.75±3.65 -5.051 < 0.001 前白蛋白(mg/L) 231.65±44.48 218.56±58.63 -1.986 0.048 谷丙转氨酶(U/L) 32.75±21.48 33.15±22.06 0.137 0.891 谷草转氨酶(U/L) 35.66±28.76 36.27±29.53 0.156 0.876 TC(mmol/L) 4.12±1.03 3.99±0.96 -0.952 0.342 TG(mmol/L) 1.43±0.57 1.37±0.62 -0.761 0.448 LDL-C(mmol/L) 1.08±0.28 1.06±0.30 -0.519 0.605 HDL-C(mmol/L) 2.35±0.68 2.31±0.57 -0.455 0.650 FPG(mmol/L) 6.21±3.75 6.26±3.68 0.099 0.921 血肌酐(μmol/L) 81.25±28.78 84.47±31.25 0.809 0.419 血尿酸(μmol/L) 358.25±125.56 346.37±127.39 -0.698 0.486 表 3 患者全因死亡及心源性再住院发生率比较[n(%)]
Table 3. Comparison of the incidence of all-cause death and cardiogenic readmission [n(%)]
分组 衰弱 非衰弱 RR(95% CI)值 χ2值 P值 死亡 总人群 15(19.74) 14(7.11) 2.77(1.41~7.04) 9.215 0.002 PCI组 10(23.30) 9(7.70) 3.02(1.32~6.93) 7.278 0.007 非PCI组 5(15.15) 5(6.25) 2.42(0.75~7.82) 2.295 0.130 全因死亡/心源性再住院 总人群 39(51.32) 37(18.78) 2.73(1.90~3.93) 28.896 < 0.001 PCI组 25(58.14) 23(19.66) 2.96(1.89~4.62) 22.173 < 0.001 非PCI组 14(42.42) 14(17.50) 2.42(1.41~8.54) 7.787 0.005 -
[1] 胡盛寿, 高润霖, 刘力生, 等. 《中国心血管病报告2018》概要[J]. 中国循环杂志, 2019, 34(3): 209-220. DOI:10. 3969/j.issn.1000-3614. 2019. 03. 001.Hu SS, Gao RL, Liu LS, et al. Summary of the 2018 Report on Cardiovascular Diseases in China[J]. Chinese Circulation Journal, 2019, 34(3): 209-220. DOI:10. 3969/j.issn.1000-3614.2019.03.001. [2] Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action[J]. J Am Med Dir Assoc, 2013, 14(6): 392-397. DOI: 10.1016/j.jamda.2013.03.022. [3] 康琳, 朱鸣雷, 刘晓红, 等. 老年稳定型冠心病患者的衰弱评估与预后分析[J]. 中华老年多器官疾病, 2016, 15(8): 583-586. DOI: 10.11915/j.issn.1671-5403.2016.08.138.Kang L, Zhu ML, Liu XH, et al. Frailty assessment and prognostic analysis of stable coronary artery disease in the elderly[J]. Chin J Muh Organ Dis Elderly, 2016, 15(8): 583-586. DOI: 10.11915/j.issn.1671-5403.2016.08.138. [4] Gharacholou SM, Roger VL, Lennon RJ, et al. Comparison of frail patients versus nonfrail patients ≥65 years of age undergoing percutaneous coronary intervention[J]. Am J Cardiol, 2012, 109(11): 1569-1575. DOI: 10.1016/j.amjcard.2012.01.384. [5] Murali-Krishnan R, Iqbal J, Rowe R, et al. Impact of frailty on outcomes after percutaneous coronary intervention: a prospective cohort study[J]. Open Heart, 2015, 2(1): e294. DOI: 10.1136/openhrt-2015-000294. [6] Lutski M, Tanne D, Goldbourt U. Tall stature in coronary heart disease patients is associated with decreased risk of frailty in late life[J]. Geriatr Gerontol Int, 2017, 17(9): 1270-1277. DOI: 10.1111/ggi.12855. [7] Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire(FRAIL)predicts outcomes in middle aged African Americans[J]. J Nutr Health Aging, 2012, 16(7): 601-608. DOI: 10.1007/s12603-012-0084-2. [8] 刘春艳, 姜春燕, 李虹伟. 衰弱合并老年心血管疾病发病机制的研究进展[J]. 临床和实验医学杂志, 2020, 19(3): 334-337. DOI:10. 3969/j. issn.1671-4695.2020.03.033.Liu CY, Jiang CY, Li HW. Research progress on pathogenesis of frailty complicated with senile cardiovascular diseases[J]. J Clin Exp Med, 2020, 19(3): 334-337. DOI: 10.3969/j.issn.1671-4695.2020.03.033. [9] Clegg A, Young J, Iliffe S, et al. Frailty in elderly people[J]. Lancet, 2013, 381(9868): 752-762. DOI: 10.1016/s0140-6736(12)62167-9. [10] 张宁, 朱文玲, 刘晓红, 等. 住院老年冠心病患者合并衰弱的患病率及影响因素研究[J]. 中国循环杂志, 2019, 34(7): 640-645. DOI: 10.3969/j.issn.1000-3614.2019.07.004.Zhang N, Zhu WL, Liu XH, et al. Cross-sectional study on the prevalence of frailty and associated risk factors in hospitalized elderly patients with coronary artery disease[J]. Chinese Circulation Journal, 2019, 34(7): 640-645. DOI: 10.3969/j.issn.1000-3614.2019.07.004. [11] Nguyen TV, Le D, Tran KD, et al. Frailty in older patients with acute coronary syndrome in Vietnam[J]. Clin Interv Aging, 2019, 14: 2213-2222. DOI: 10.2147/CIA.S234597. [12] Hou P, Xue HP, Mao XE, et al. Inflammation markers are associated with frailty in elderly patients with coronary heart disease[J]. Aging (Albany NY), 2018, 10(10): 2636-2645. DOI: 10.18632/aging.101575. [13] 张宁, 朱文玲, 刘晓红, 等. 住院老年冠心病患者衰弱与肌肉功能评价的横断面分析[J]. 中华内科杂志, 2019, 58(4): 265-269. DOI: 10.3760/cma.j.issn.0578-1426.2019.04.006.Zhang N, Zhu WL, Liu XH, et al. A cross-sectional study on the association between frailty and muscular performances in hospitalized elder patients with coronary artery disease[J]. Chin J Intern Med, 2019, 58(4): 265-269. DOI: 10.3760/cma.j.issn.0578-1426.2019.04.006. [14] Kang L, Zhang SY, Zhu WL, et al. Is frailty associated with short-term outcomes for elderly patients with acute coronary syndrome?[J]. J Geriatr Cardiol, 2015, 12(6): 662-667. DOI: 10.11909/j.issn.1671-5411.2015.06.010. [15] Man C, Xiang S, Fan Y. Frailty for predicting all-cause mortality in elderly acute coronary syndrome patients: a meta-analysis[J]. Ageing Res Rev, 2019, 52: 1-6. DOI: 10.1016/j.arr.2019.03.003. [16] Ekerstad N, Swahn E, Janzon M, et al. Frailty is independently associated with short-term outcomes for elderly patients with non-ST segment elevation myocardial infarction[J]. Circulation, 2011, 124(22): 2397-2404. DOI: 10.1161/CIRCULATIONAHA.111.025452. [17] 张绍敏, 郑融融, 刘洋, 等. 衰弱对老年急性冠脉综合征患者短期预后的影响[J]. 现代生物医学进展, 2016, 16(26): 5058-5061. DOI: 10.13241/j.cnki.pmb.2016.26.014.Zhang SM, Zheng RR, Liu Y, et al. Impact of weakness on short term prognosis of elderly patients with acute coronary syndrome[J]. Prog Mod Biomed, 2016, 16(26): 5058-5061. DOI: 10.13241/j.cnki.pmb.2016.26.014. [18] Vandermolen S, Abbott J, De Silva K. What's age got to do with it? A review of contemporary revascularization in the elderly[J]. Curr Cardiol Rev, 2015, 11(3): 199-208. DOI: 10.2174/1573403x10666141020110122. [19] Tse G, Gong M, Nunez J, et al. Frailty and mortality outcomes after percutaneous coronary intervention: a systematic review and meta-analysis[J]. J Am Med Dir Assoc, 2017, 18(12): 1097. e1-1097. e10. DOI: 10.1016/j.jamda.2017.09.002. -





 下载:
下载: