-
摘要:
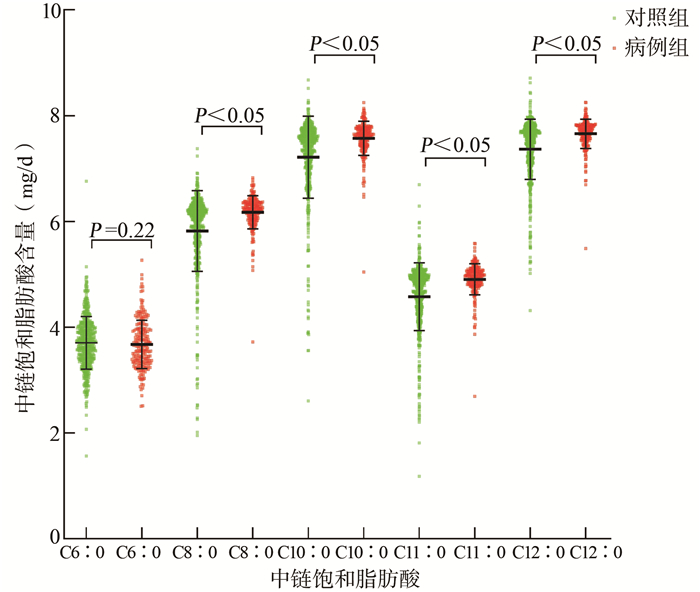
目的 探讨膳食中链饱和脂肪酸与口腔癌发病的关联。 方法 本病例对照研究以面访式问卷的形式调查2013年11月14日至2019年3月21日在福建医科大学附属第一医院口腔颌面外科确诊的225例新发口腔癌患者及527例健康对照。以对照组中能量校正后的各类脂肪酸每日摄入量的中位数进行分组,进行非条件Logistic回归分析模型分析、分层分析及相乘交互作用分析。 结果 高水平组的总中链饱和脂肪酸、辛酸、癸酸、十一烷酸及月桂酸等与口腔癌的发病风险呈正相关,其调整后的OR值及其95% CI值分别为3.19(95% CI: 2.17~4.69)、2.54(95% CI: 1.75~3.69)、2.56(95% CI: 1.76~3.71)、5.00(95% CI: 3.27~7.64)和3.09(95% CI: 2.10~4.54)。在不吸烟者中,辛酸和癸酸与口腔癌发生风险呈正相关,且无论是否饮酒,其均能增加口腔癌的发病风险;各亚组均发现高总中链饱和脂肪酸、十一烷酸及月桂酸摄入量与口腔癌发生风险呈正相关。此外,中链饱和脂肪酸与吸烟、饮酒存在相乘交互作用。 结论 较高水平的膳食中链饱和脂肪酸可能会增加口腔癌的发病风险。 Abstract:Objective To investigate the association between dietary medium-chain saturated fatty acids and the risk of oral cancer. Methods A case-control study was conducted in 225 patients with diagnosed oral cancer and 527 controls. All participants were recruited from the First Affiliated Hospital of Fujian Medical University from November 14, 2013 to March 21, 2019. The median daily intake of all kinds of fatty acids after energy correction in the control group was divided into groups. Unconditional Logistic regression analysis stratified analysis and multiplicative interaction analysis were performed, stratified analysis and multiplicative interaction analysis were performed to investigate the relationship between medium chain saturated fatty acids and the risk of oral cancer. Results Compared with the low-level group, the total medium-chain saturated fatty acids, octanoic acid, decanoic acid, undecanoic acid and lauric acid in the high-level group may increase the risk of oral cancer. The adjusted OR and 95% CI were 3.19 (95% CI: 2.17-4.69), 2.54 (95% CI: 1.75-3.69)、2.56 (95% CI: 1.76-3.71)、5.00 (95% CI: 3.27-7.64) and 3.09 (95% CI: 2.10-4.54), respectively. Stratified analysis showed that octanoic acid and decanoic acid were risk factors of oral cancer among non-smokers, and they may also increased the risk of oral cancer regardless of drinking status. There was a positive correlation between the daily intake of total medium-chain saturated fatty acids, undecanoic acid and lauric acid and the risk for oral cancer regardless of smoking and drinking status. In addition, there were multiplicative interactions between medium-chain saturated fatty acids and smoking or drinking status. Conclusion A higher level of dietary medium-chain saturated fatty acids may increase the risk of oral cancer. -
Key words:
- Oral cancer /
- Dietary medium chain saturated fatty acid /
- Risk factor /
- Smoking /
- Drinking
-
表 1 病例组与对照组的一般人口学特征比较[n(%)]
Table 1. Comparison of general characteristics between the case group and the control group [n(%)]
特征 病例组 对照组 χ2值 P值 年龄(岁) 72.494 < 0.001 < 60 108(48.00) 417(79.13) ≥60 117(52.00) 110(20.87) 性别 2.690 0.101 男 121(53.78) 249(47.25) 女 104(46.22) 278(52.75) 文化程度 17.217 < 0.001 文盲 16(7.11) 41(7.78) 小学及初中 153(68.00) 275(52.18) 高中及以上 56(24.89) 211(40.04) 婚姻状况 5.697 0.017 已婚 205(91.11) 446(84.63) 未婚及其他 20(8.89) 81(15.37) 职业 7.178 < 0.001 农民 84(37.33) 145(27.51) 其他 141(62.67) 382(72.49) 居住地 3.522 0.061 农村 135(60.00) 277(52.56) 城市 90(40.00) 250(47.44) BMI(kg/m2) 7.974 0.019 < 18.5 20(8.89) 40(7.59) 18.5~ < 24.0 150(66.67) 303(57.50) ≥24.0 55(24.44) 184(34.91) 吸烟 4.979 0.026 无 137(60.89) 365(69.26) 有 88(39.11) 162(30.74) 饮酒 17.572 < 0.001 无 148(65.78) 422(80.08) 有 77(34.22) 105(19.92) 肿瘤家族史 1.064 0.302 无 191(84.89) 462(87.67) 有 34(15.11) 65(12.33) 注:表中数据收集于福建省2013年11月14日至2019年3月21日。 表 2 中链饱和脂肪酸与口腔癌关联的非条件Logistic回归分析模型分析
Table 2. The unconditional Logistic regression analysis of medium-chain saturated fatty acids on oral cancer
变量(mg/d) OR(95% CI)值 P值 OR(95% CI)值a P值 总中链饱和脂肪酸 ≤29.40 1.00 1.00 >29.40 3.34(2.34~4.76) < 0.001 3.19(2.17~4.69) < 0.001 C6∶0 ≤3.71 1.00 1.00 >3.71 0.80(0.58~1.09) 0.156 0.79(0.56~1.11) 0.170 C8∶0 ≤6.06 1.00 1.00 >6.06 2.80(1.99~3.95) < 0.001 2.54(1.75~3.69) < 0.001 C10∶0 ≤7.46 1.00 1.00 >7.46 2.68(1.91~3.76) < 0.001 2.56(1.76~3.71) < 0.001 C11∶0 ≤4.75 1.00 1.00 >4.75 5.10(3.45~7.55) < 0.001 5.00(3.27~7.64) < 0.001 C12∶0 ≤7.54 1.00 1.00 >7.54 3.23(2.27~4.60) < 0.001 3.09(2.10~4.54) < 0.001 注:a调整年龄、性别、文化程度、婚姻状况、职业、居住地、BMI、肿瘤家族史、饮酒。 表 3 中链饱和脂肪酸与口腔癌的分层分析
Table 3. Stratified analysis on the association between medium-chain saturated fatty acids and the risk of oral cancer
变量(mg/d) 调整OR(95% CI)值a 调整OR(95% CI)值b 吸烟 不吸烟 饮酒 不饮酒 总中链饱和脂肪酸 ≤29.40 1.00 1.00 1.00 1.00 >29.40 1.90(1.03~3.53) 4.72(2.76~8.07) 3.23(1.58~6.59) 3.28(2.04~5.28) C6∶0 ≤3.71 1.00 1.00 1.00 1.00 >3.71 0.89(0.49~1.64) 0.73(0.48~1.12) 0.89(0.44~1.77) 0.74(0.50~1.11) C8∶0 ≤6.06 1.00 1.00 1.00 1.00 >6.06 1.63(0.88~3.02) 3.53(2.14~5.84) 2.06(1.04~4.10) 2.79(1.76~4.43) C10∶0 ≤7.46 1.00 1.00 1.00 1.00 >7.46 1.56(0.84~2.89) 3.75(2.27~6.22) 2.29(1.15~4.56) 2.73(1.73~4.32) C11∶0 ≤4.75 1.00 1.00 1.00 1.00 >4.75 3.47(1.79~6.72) 7.50(4.06~13.85) 4.02(1.93~8.36) 6.11(3.50~10.68) C12∶0 ≤7.54 1.00 1.00 1.00 1.00 >7.54 2.15(1.15~4.04) 4.03(2.41~6.75) 2.53(1.26~5.08) 3.41(2.11~5.51) 注:a调整年龄、性别、文化程度、婚姻状况、职业、居住地、BMI、肿瘤家族史、饮酒;b调整年龄、性别、文化程度、婚姻状况、职业、居住地、BMI、肿瘤家族史、吸烟。 表 4 中链饱和脂肪酸与吸烟、饮酒的交互作用[n(%)]
Table 4. Analysis of the interaction between medium-chain saturated fatty acids and smoking and drinking [n(%)]
变量(mg/d) 病例组 对照组 OR(95% CI)值 总中链饱和脂肪酸 吸烟a ≤29.40 无 21(9.33) 176(33.40) 1.00 ≤29.40 有 31(13.78) 88(16.70) 1.62(0.78~3.35) >29.40 无 116(51.56) 189(35.86) 4.83(2.81~8.28) >29.40 有 57(25.33) 74(14.04) 3.01(1.51~6.01) 总中链饱和脂肪酸×吸烟 1.48(0.91~2.40) 总中链饱和脂肪酸 饮酒b ≤29.40 无 28(12.44) 202(38.33) 1.00 ≤29.40 有 24(10.67) 62(11.76) 2.57(1.30~5.10) >29.40 无 120(53.33) 220(41.75) 3.27(2.03~5.26) >29.40 有 53(23.56) 43(8.16) 7.81(4.14~14.72) 总中链饱和脂肪酸×饮酒 3.50(2.11~5.83) C6∶0 吸烟a ≤3.71 无 78(34.67) 184(34.91) 1.00 ≤3.71 有 47(20.89) 79(14.99) 0.81(0.44~1.50) >3.71 无 59(26.22) 181(34.35) 0.73(0.48~1.12) >3.71 有 41(18.22) 83(15.75) 0.73(0.38~1.37) C6∶0×吸烟 0.88(0.53~1.45) C6∶0 饮酒b ≤3.71 无 85(37.78) 214(40.60) 1.00 ≤3.71 有 40(17.78) 49(9.30) 2.04(1.14~3.63) >3.71 无 63(28.00) 208(39.47) 0.74(0.49~1.11) >3.71 有 37(16.44) 56(10.63) 1.88(1.06~3.35) C6∶0×饮酒 1.67(0.99~2.81) C8∶0 吸烟a ≤6.06 无 26(11.56) 174(33.02) 1.00 ≤6.06 有 33(14.67) 89(16.89) 1.45(0.72~2.90) >6.06 无 111(49.33) 191(36.24) 3.55(2.14~5.88) >6.06 有 55(24.44) 73(13.85) 2.29(1.17~4.49) C8∶0×吸烟 1.32(0.80~2.15) C8∶0 饮酒b ≤6.06 无 32(14.22) 203(38.51) 1.00 ≤6.06 有 27(12.00) 60(11.39) 2.90(1.50~5.59) C8∶0 饮酒b >6.06 无 116(51.56) 219(41.56) 2.83(1.79~4.49) >6.06 有 50(22.22) 45(8.54) 5.88(3.16~10.97) C8∶0×饮酒 2.74(1.65~4.55) C10∶0 吸烟a ≤7.46 无 26(11.55) 176(33.40) 1.00 ≤7.46 有 35(15.56) 87(16.51) 1.54(0.77~3.07) >7.46 无 111(49.33) 189(35.86) 3.81(2.29~6.32) >7.46 有 53(23.56) 75(14.23) 2.26(1.15~4.41) C10∶0×吸烟 1.25(0.76~2.04) C10∶0 饮酒b ≤7.46 无 33(14.67) 203(38.51) 1.00 ≤7.46 有 28(12.44) 60(11.39) 2.80(1.46~5.37) >7.46 无 115(51.11) 219(41.56) 2.79(1.76~4.41) >7.46 有 49(21.78) 45(8.54) 6.01(3.22~11.20) C10∶0×饮酒 2.85(1.71~4.73) C11∶0 吸烟a ≤4.75 无 14(6.22) 174(33.02) 1.00 ≤4.75 有 23(10.22) 90(17.08) 1.75(0.77~3.98) >4.75 无 123(54.67) 191(36.24) 7.72(4.16~14.36) >4.75 有 65(28.89) 72(13.66) 5.32(2.51~11.29) C11∶0×吸烟 2.00(1.23~3.25) C11∶0 饮酒b ≤4.75 无 17(7.56) 203(38.52) 1.00 ≤4.75 有 20(8.89) 61(11.57) 3.87(1.79~8.39) >4.75 无 131(58.22) 219(41.56) 6.26(3.58~10.96) >4.75 有 57(25.33) 44(8.35) 13.50(6.71~27.15) C11∶0×饮酒 3.61(2.19~5.94) C12∶0 吸烟a ≤7.54 无 24(10.67) 176(33.40) 1.00 ≤7.54 有 29(12.89) 87(16.51) 1.35(0.66~2.79) >7.54 无 113(50.22) 189(35.86) 4.14(2.47~6.95) >7.54 有 59(26.22) 75(14.23) 2.78(1.42~5.45) C12∶0×吸烟 1.55(0.95~2.52) C12∶0 饮酒b ≤7.54 无 28(12.44) 204(38.70) 1.00 ≤7.54 有 25(11.11) 59(11.20) 2.98(1.51~5.90) >7.54 无 120(53.33) 218(41.37) 3.45(2.14~5.57) >7.54 有 52(23.12) 46(8.73) 7.45(3.95~14.06) C12∶0×饮酒 3.09(1.87~5.11) 注:a调整年龄、性别、文化程度、婚姻状况、职业、居住地、BMI、肿瘤家族史、饮酒;b调整年龄、性别、文化程度、婚姻状况、职业、居住地、BMI、肿瘤家族史、吸烟。 -
[1] 李江, 张春叶. 口腔癌及口咽癌病理诊断规范[J]. 中国口腔颌面外科杂志, 2020, 18(4): 289-296. DOI: 10.3760/cma.j.issn.1002-0098.2020.03.001.Li J, Zhang CY. Guideline on pathological diagnosis of oral and oropharyngeal squamous cell carcinoma[J]. China J of Oral Maxillofac Surg, 2020, 18(4): 289-296. DOI: 10.3760/cma.j.issn.1002-0098.2020.03.001. [2] 郑雄伟. 2017福建省肿瘤登记年报[M]. 福州: 福建科学技术出版社, 2018.Zheng XW. 2017 Fujian cancer registry annual report[M]. Fuzhou: Fujian Science and Technology Press, 2018. [3] Petrick JL, Castro-Webb N, Gerlovin H, et al. A prospective analysis of intake of red and processed meat in relation to pancreatic cancer among African American women[J]. Cancer Epidem Biomar, 2020, 29(9): 1775-1783. DOI: 10.1158/1055-9965.EPI-20-0048. [4] Zhu YH, Jeong S, Wu M, et al. Dietary intake of fatty acids, total cholesterol, and stomach cancer in a Chinese population[J]. Nutrients, 2019, 11(8)1730. DOI: 10.3390/nu11081730. [5] Duarte-Salles T, Fedirko V, Stepien M, et al. Dietary fat, fat subtypes and hepatocellular carcinoma in a large European cohort[J]. Int J Cancer, 2015, 137(11): 2715-2728. DOI: 10.1002/ijc.29643. [6] Cao Y, Hou L, Wang W. Dietary total fat and fatty acids intake, serum fatty acids and risk of breast cancer: a Meta-analysis of prospective cohort studies[J]. Int J Cancer, 2016, 138(8): 1894-1904. DOI: 10.1002/ijc.29938. [7] Ruan L, Cheng SP, Zhu QX. Dietary fat intake and the risk of skin cancer: a systematic review and Meta-analysis of observational studies[J]. Nutr Cancer, 2020, 72(3): 398-408. DOI: 10.1080/01635581.2019.1637910. [8] 苏宜香, 郭艳. 膳食脂肪酸构成及适宜推荐比值的研究概况[J]. 中国油脂, 2003, 28(1): 31-34. DOI: 10.3321/j.issn:1003-7969.2003.01.011.Su YX, Guo Y. A review of dietary fatty acid composition and recommended optimal ratio[J]. China Oils Fats, 2003, 28(1): 31-34. DOI: 10.3321/j.issn:1003-7969.2003.01.011. [9] RadoiL, Paget-Bailly S, Menvielle G, et al. Tea and coffee consumption and risk of oral cavity cancer: results of a large population-based case-control study, the ICARE study[J]. Cancer Epidemiol, 2013, 37(3): 284-289. DOI: org/ 10.1016/j.canep.2013.02.001. [10] Chen F, He BC, Hu Z, et al. Passive smoking and Cooking Oil Fumes (COF) may modify the association between tea consumption and oral cancer in Chinese women[J]. J Cancer Res Clin Oncol, 2016, 142(5): 995-1001. DOI: 10.1007/s00432-016-2123-6. [11] 魏跃红, 吕桦, 倪进发, 等. 吸烟、饮酒与胃癌关系的条件logistic回归分析[J]. 中华疾病控制杂志, 2006, 10(2): 116-119. DOI: 10.3969/j.issn.1674-3679.2006.02.004.Wei YH, Lv H, Ni JF, et al. Conditional logistic analysis of smoking, alcohol consumption and gastric cancer[J]. Chin J Dis Control Prev, 2006, 10(2): 116-119. DOI: 10.3969/j.issn.1674-3679.2006.02.004. [12] Yan LJ, Chen F, He BC, et al. A novel environmental exposure index and its interaction with familial susceptibility on oral cancer in non-smokers and non-drinkers: a case-control study[J]. Eur Arch Otorhinolaryngol, 2017, 274(4): 1945-1950. DOI: 10.1007/s00405-016-4427-1. [13] 杨月欣, 中国疾病预防控制中心营养与健康所. 中国食物成分表标准版[M]. 北京: 北京大学医学出版社, 2018.Yang YX, Nutrition and Health Institute, Chinese Center for Disease Control and Prevention. China food composition tables standard edition[M]. Beijing: Peking University Medical Press, 2018. [14] Chaturvedi P, Singh A, Chien CY, et al. Tobacco related oral cancer[J]. BMJ. 2019, 365: l2142. DOI: 10.1136/bmj.l2142. [15] Di CG, Polesel J, Dal ML, et al. Alcohol drinking and head and neck cancer risk: the joint effect of intensity and duration[J]. Br J Cancer, 2020, 123: 1456-1463. DOI: 10.1038/s41416-020-01031-z. [16] Auguste A, Deloumeaux J, Joachim C, et al. Joint effect of tobacco, alcohol, and oral HPV infection on head and neck cancer risk in the French West Indies[J]. Cancer Med, 2020, 9(18): 1-10. DOI: 10.1002/cam4.3327. [17] Su SY, Chen WT, Chiang CJ, et al. Oral cancer incidence rates from 1997 to 2016 among men in Taiwan: association between birth cohort trends and betel nut consumption[J]. Oral Oncol, 2020, 107: 104798. DOI: 10.1016/j.oraloncology.2020.104798. [18] Xu J, Yang XX, Wu YG, et al. Meat consumption and risk of oral cavity and oropharynx cancer: a Meta-analysis of observational studies[J]. PLoS ONE, 2014, 9(4): e95048. DOI: 10.1371/journal.pone.0095048. [19] Kim Y, Je Y, Giovannucci EL. Association between dietary fat intake and mortality from all-causes, cardiovascular disease, and cancer: a systematic review and Meta-analysis of prospective cohort studies[J]. Clin Nutr, 2020. DOI: 10.1016/j.clnu.2020.07.007. [20] Jansen RJ, Robinson DP, Frank RD, et al. Fatty acids found in dairy, protein and unsaturated fatty acids are associated with risk of pancreatic cancer in a case-control study[J]. Int J Cancer, 2014, 134(8): 1935-1946. DOI: 10.1002/ijc.28525. [21] Nkondjock A, Shatenstein B, Maisonneuve P, et al. Specific fatty acids and human colorectal cancer: an overview[J]. Cancer Detect and Prev, 2003, 27(1): 55-66. DOI: 10.1016/s0361-090x(02)00179-4. [22] 宋传宇, 戴辛鹏, 关键. COX-2及NF-κB在口腔鳞癌组织中的表达及相关性研究[J]. 医学理论与实践, 2018, 31(11): 1565-1567, 1570. DOI: 10.19381/j.issn.1001-7585.2018.11.002.Song CY, Dai XP, Guan J. COX-2 and NF-κB Expression and Correlation in OSCC[J]. J Med Theor Prac, 2018, 31(11): 1565-1567, 1570. DOI: 10.19381/j.issn.1001-7585.2018.11.002. [23] Rodríguez RM, López P, Rodríguez-Santiago RE, et al. Cigarette smoking modulation of saliva microbial composition and cytokine levels[J]. Int J Environ Res Public Health, 2018, 15(11): 2479. DOI: 10.3390/ijerph15112479. [24] 时小婷, 潘亚萍. 烟酒致癌物致口腔细胞恶性转化的研究进展[J]. 中国医科大学学报, 2020, 49(3): 264-268. DOI: 10.12007/j.issn.0258-4646.2020.03.015.Shi XT, Pan YP. Advances in research on the malignant transformation of oral cells caused by tobacco and alcohol carcinogens[J]. J China Med Univ, 2020, 49(3): 264-268. DOI: 10.12007/j.issn.0258-4646.2020.03.015. -





 下载:
下载: