Association between combined trajectories of cardiac structure and function indicators and prognosis of chronic heart failure
-
摘要:
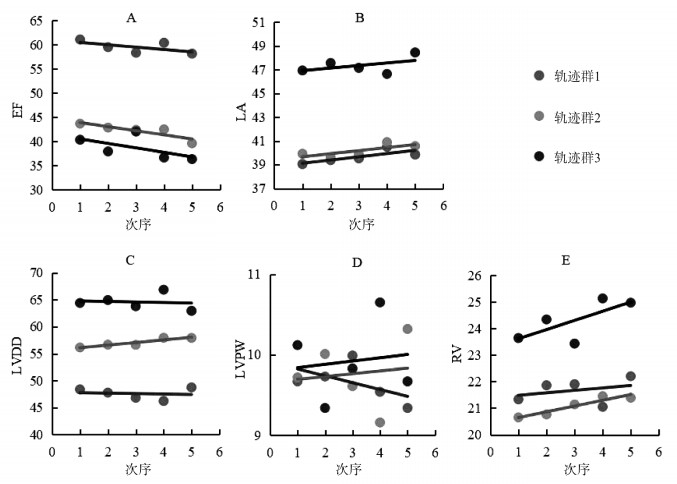
目的 探讨心脏结构及功能指标纵向变化轨迹群对慢性心力衰竭(chronic heart failure, CHF)预后存在的潜在价值。 方法 纳入2012年1月-2019年1月在山西省两所三级甲等医院住院并符合标准的277例患者,利用多次住院的心脏结构及功能指标,建立基于群组的多轨迹模型,识别具有相似轨迹变化的患者群体。使用Cox比例风险回归模型分析轨迹群对患者死亡风险的影响。 结果 共识别轨迹指标变化各异、基线特征分布存在差异的3组轨迹群组。其中轨迹群1中患者男女均衡,纽约心脏病协会(New York Heart Association, NYHA)心功能分级集中于Ⅱ~Ⅲ级,射血分数(ejection fraction, EF)整体较稳定并高于另外两组,不稳定型心绞痛的患者较多;轨迹群2中男性、陈旧性心肌梗死患者占比高,EF稳定下降;轨迹群3中男性、NYHA心功能分级为Ⅳ级的患者比例高,EF呈现波动下降状态,患缺血性心肌病、瓣膜性心脏病和房颤的患者多。Cox比例风险回归模型结果表明轨迹群组在单独纳入、校正基线特征和校正共病影响三种情况下均为CHF患者发生死亡的影响因素。 结论 基于心脏结构及功能指标纵向变化识别的轨迹群能够对CHF患者的死亡风险进行分层,有助于帮助识别高危患者。 Abstract:Objective To explore the potential value of the longitudinal trajectory groups of cardiac structure and function indicators for the prognosis of patients with chronic heart failure. Methods A total of 277 patients who were hospitalized in two tertiary hospitals in Shanxi Province from January 2012 to January 2019 and met the criteria were included. The cardiac structure and function indicators of multiple hospitalizations were used to establish the group-based multi-trajectory model to identify patient groups with similar trajectory changes. The Cox proportional hazards regression model was used to analyze the influence of trajectory group on the risk of death of patients. Results Three trajectory groups with different changes in trajectory indicators and baseline feature distributions were identified. Among them, patients in trajectory group 1 were balanced between men and women, New York Heart Association (NYHA) functional class was concentrated in grades Ⅱ-Ⅲ, the overall ejection fraction (EF) was relatively stable, which was higher than the other two groups, and more patients had unstable angina. The proportion of men and patients with old myocardial infarction in trajectory group 2 were high, and the EF was steadily decreasing. Trajectory group 3 had a high proportion of males and NYHA grade IV patients, EF presented a fluctuated decline state, ischemic cardiomyopathy, valvular heart disease and atrial fibrillation were more common. The results of the Cox proportional hazards regression model showed that the trajectory group were an influencing factor for the death of patients with chronic heart failure under the three conditions of individual inclusion, adjustment of baseline characteristics, and adjustment of comorbidity. Conclusion The trajectory groups identified based on the longitudinal changes of cardiac structure and function indicators can stratify the death risk of patients with chronic heart failure and help identify high-risk patients. -
Key words:
- Chronic heart failure /
- Group-based trajectory model /
- Risk of death
-
表 1 患者基本特征描述及轨迹组间比较结果[n(%)]
Table 1. Description of basic characteristics of patients and comparison results between trajectories groups [n(%)]
指标 例数(N=277) 轨迹群1(n=133) 轨迹群2(n=99) 轨迹群3(n=45) F/χ2/H值 P值 人口学特征 年龄(x±s, 岁) 70.51±10.63 71.92±9.54 69.52±11.38 68.53±11.61 2.403 0.092 BMI(x±s, kg/m2) 25.14±3.53 25.65±3.70 24.37±3.27 25.35±3.33 3.850 0.022 a 性别 16.305 < 0.001 a 男性 175(63.18) 68(51.13) 72(72.73) 35(77.78) 女性 102(36.82) 65(48.87) 27(27.27) 10(22.22) NYHA心功能分级 14.441 0.001 a Ⅱ级 122(44.04) 66(49.62) 43(43.43) 13(28.89) Ⅲ级 102(36.82) 54(40.60) 35(35.35) 13(28.89) Ⅳ级 53(19.14) 13(9.78) 21(21.22) 19(42.22) 影像学检查(x±s, mm) EF 51.50±12.74 61.10±8.46 43.69±8.24 40.35±10.45 156.586 < 0.001 a LA 40.64±5.33 39.05±4.95 39.92±3.84 46.93±4.76 52.258 < 0.001 a LVDD 53.76±9.81 48.38±7.97 56.15±8.22 64.40±6.83 76.368 < 0.001 a LVPW 9.76±2.05 9.67±1.42 9.72±2.09 10.12±3.25 0.827 0.438 RV 21.46±3.04 21.33±2.88 20.65±2.31 23.64±3.82 17.048 < 0.001 a 共病情况 高血压 202(72.92) 103(77.44) 65(65.66) 34(75.56) 4.182 0.124 糖尿病 96(34.66) 50(37.59) 30(30.30) 16(35.56) 1.351 0.523 冠心病 259(93.50) 121(90.98) 95(95.96) 43(95.56) 2.692 0.258 不稳定型心绞痛 168(60.65) 92(69.17) 53(53.54) 23(51.11) 7.864 0.020 a 陈旧性心肌梗死 153(55.23) 39(29.32) 85(85.86) 29(64.44) 75.207 < 0.001 a 缺血性心肌病 16(5.78) 3(2.26) 8(8.08) 5(11.11) 6.348 0.039 a 瓣膜性心脏病 24(8.66) 11(8.27) 5(5.05) 8(17.78) 6.383 0.036 a 房颤 57(20.58) 31(23.31) 12(12.12) 14(31.11) 7.994 0.018 a 陈旧性脑梗死 26(9.39) 14(10.53) 9(9.09) 3(6.67) 0.605 0.730 慢性阻塞性肺疾病 6(2.17) 3(2.26) 2(2.02) 1(2.22) 0.016 1.000 肺部感染 73(26.35) 28(21.05) 31(31.31) 14(31.11) 3.705 0.157 血脂异常 48(17.33) 30(22.56) 12(12.12) 6(13.33) 4.913 0.090 肾功能不全 18(6.50) 7(5.26) 6(6.06) 5(11.11) 1.941 0.393 结局 3.545 0.169 好转 249(89.89) 124(93.23) 87(87.88) 38(84.44) 死亡 28(10.11) 9(6.77) 12(12.12) 7(15.56) 注:a P < 0.05。 表 2 基于群组的多轨迹模型代表性拟合结果
Table 2. Representative fitting results of group-based multi-trajectory model
指标 群组数 亚组阶数 |BIC| |AIC| 群组最少样本占比 群组最小平均后验概率 熵值 仅轨迹指标 1 (1)/(1)/(1)/(1)/(1) 14 554.19 14 527.01 - - 仅轨迹指标 2 (1, 1)/(1, 1)/(1, 1)/(1, 1)/(1, 1) 14 196.77 14 149.66 45.50 0.96 0.89 3 (1, 1, 1)/(1, 1, 1)/(1, 1, 1)/(1, 1, 1)/(1, 1, 1) 14 114.34 14 047.30 16.50 0.92 0.89 3 (1, 1, 1)/(1, 1, 1)/(2, 1, 1)/(1, 1, 1)/(1, 1, 1) 14 115.41 14 046.56 16.50 0.92 0.89 3 (1, 1, 1)/(1, 1, 2)/(2, 1, 1)/(1, 1, 1)/(1, 1, 1) 14 118.20 14 047.54 16.50 0.92 0.89 3 (1, 1, 1)/(1, 1, 1)/(2, 1, 2)/(1, 1, 1)/(1, 1, 1) 14 120.74 14 048.26 16.70 0.92 0.89 3 (1, 1, 1)/(1, 1, 3)/(3, 1, 1)/(1, 1, 1)/(1, 3, 1) 14 127.62 14 049.70 16.40 0.92 0.89 4 (1, 1, 1, 1)/(1, 1, 1, 1)/(1, 1, 1, 1)/(1, 1, 1, 1)/(1, 1, 1, 1) 13 961.66 13 874.68 1.40 0.97 0.95 轨迹指标+时依协变量 3 (1, 1, 1)/(1, 1, 1)/(1, 1, 1)/(1, 1, 1)/(1, 1, 1) 14 098.17 14 014.81 17.10 0.96 0.90 轨迹指标+稳定协变量+时依协变量 3 (1, 1, 1)/(1, 1, 1)/(1, 1, 1)/(1, 1, 1)/(1, 1, 1) 14 095.59 14 008.62 17.20 0.94 0.90 表 3 轨迹群组与CHF预后关联的Cox回归分析
Table 3. Cox regression analysis of the correlation between trajectory groups and CHF prognosis
指标 HR(95% CI)值 P值 单因素分析 高血压 1.114(0.473~2.622) 0.804 糖尿病 1.883(0.898~3.952) 0.094 冠心病 2.316(0.314~17.060) 0.410 不稳定型心绞痛 1.204(0.555~2.611) 0.638 陈旧性心肌梗死 1.365(0.639~2.916) 0.421 缺血性心肌病 1.575(0.374~6.637) 0.536 瓣膜性心脏病 1.758(0.610~5.067) 0.296 房颤 1.089(0.441~2.686) 0.853 陈旧性脑梗死 1.683(0.584~4.851) 0.335 慢性阻塞性肺疾病 4.113(0.975~17.348) 0.054 肺部感染 1.915(0.897~4.090) 0.093 血脂异常 2.051(0.903~4.659) 0.086 肾功能不全 1.841(0.555~6.107) 0.318 多因素分析 模型1 轨迹群1 1.000 轨迹群2 1.913(0.806~4.540) 0.141 轨迹群3 2.901(1.079~7.800) 0.035 模型2 轨迹群1 1.000 轨迹群2 2.290(0.950~5.523) 0.065 轨迹群3 3.847(1.330~11.130) 0.013 年龄 1.090(1.036~1.147) 0.001 NYHA心功能分级Ⅱ级 1.000 NYHA心功能分级Ⅲ级 2.656(1.080~6.531) 0.033 NYHA心功能分级Ⅳ级 1.402(0.452~4.352) 0.558 模型3 轨迹群1 1.000 轨迹群2 2.514(1.032~6.123) 0.042 轨迹群3 4.487(1.624~12.398) 0.004 年龄 1.092(1.039~1.148) < 0.001 糖尿病 2.344(1.087~5.058) 0.030 慢性阻塞性肺疾病 5.309(1.125~25.058) 0.035 血脂异常 3.631(1.536~8.584) 0.003 注:模型1纳入指标:轨迹群;模型2纳入指标:轨迹群、年龄、性别、NYHA心功能分级和BMI;模型3纳入指标:轨迹群、年龄、性别、NYHA心功能分级、BMI、糖尿病、慢性阻塞性肺疾病、肺部感染和血脂异常。 -
[1] Udelson JE, Konstam MA. Ventricular remodeling: fundamental to the progression (and regression) of heart failure[J]. J Am Coll Cardiol, 2011, 57(13): 1477-1479. DOI: 10.1016/j.jacc.2011.01.009. [2] Adamson PD, Verryt T, Frampton CM, et al. Age-related differences in ventricular remodeling and long-term heart failure outcomes following acute coronary syndrome[J]. Eur Heart J, 2020, 41. DOI: 10.1093/ehjci/ehaa946.0914. [3] Tadic M, Cuspidi C, Celic V, et al. The prognostic importance of right ventricular remodeling and the circadian blood pressure pattern on the long-term cardiovascular outcome[J]. J Hypertension, 2020, 38(8): 1525-1530. DOI: 10.1097/HJH.0000000000002432. [4] Lu C, Chen J, Suksaranjit P, et al. Regional myocardial remodeling characteristics correlates with cardiac events in sarcoidosis[J]. J Magn Reson Imaging, 2020, 52(2): 499-509. DOI: 10.1002/jmri.27057. [5] Borlaug BA. Evaluation and management of heart failure with preserved ejection fraction[J]. Nat Rev Cardiol, 2020, 17(9): 559-573. DOI: 10.1038/s41569-020-0363-2. [6] Shah JS, Kitzman WD, Borlaug AB, et al. Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap[J]. Circulation, 2016, 134(1): 73-90. DOI: 10.1161/CIRCULATIONAHA.116.021884. [7] Jensen PB, Jensen LJ, Brunak S. Mining electronic health records: towards better research applications and clinical care[J]. Nat Rev Genet, 2012, 13(6): 395-405. DOI: 10.1038/nrg3208. [8] 中华医学会心血管病学分会心力衰竭学组, 中国医师协会心力衰竭专业委员会, 中华心血管病杂志编辑委员会. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. DOI: 10.3760/cma.j.issn.0253-3758.2018.10.004.Heart Failure Group of Chinese Society of Cardiology of Chinese Medical Association, Chinese Heart Failure Association of Chinese Medical Doctor Association, Editorial Board of Chinese Journal of Cardiology. Chinese guidelines for the diagnosis and treatment of heart failure 2018[J]. Chin J Cardiol, 2018, 46(10): 760-789. DOI: 10.3760/cma.j.issn.0253-3758.2018.10.004. [9] Angraal S, Mortazavi BJ, Gupta A, et al. Machine learning prediction of mortality and hospitalization in heart failure with preserved ejection fraction[J]. JACC-Heart Fail, 2020, 8(1): 12-21. DOI: 10.1016/j.jchf.2019.06.013. [10] Fei T, Ishwaran H. Random forest missing data algorithms[J]. Stat Anal Data Min, 2017, 10(6): 363-377. DOI: 10.1002/sam.11348. [11] Wells BJ, Nowacki AS, Chagin K, et al. Strategies for handling missing data in electronic health record derived data[J]. Egems, 2013, 1(3): 1035. DOI: 10.13063/2327-9214.1035. [12] Stekhoven JD, Bühlmann P. MissForest-non-parametric missing value imputation for mixed-type data[J]. Bioinformatics, 2012, 28(1): 112-118. DOI: 10.1093/bioinformatics/btr597. [13] Franklin JM, Shrank WH, Pakes J, et al. Group-based trajectory models[J]. Med Care, 2013, 51(9): 789-796. DOI: 10.1097/mlr.0b013e3182984c1f. [14] Nagin DS, Jones BL, Passos VL, et al. Group-based multi-trajectory modeling[J]. Stat Method Med Res, 2018, 27(7): 2015-2023. DOI: 10.1177/0962280216673085. [15] 张晨旭, 谢峰, 林振, 等. 基于组轨迹模型及其研究进展[J]. 中国卫生统计, 2020, 37(6): 946-949. DOI: 10.3969/j.issn.1002-3674.2020.06.039.Zhang CX, Xie F, Lin Z, et al. Group-based trajectory model and its research progress[J]. Chinese Journal of Health Statistics, 2020, 37(6): 946-949. DOI: 10.3969/j.issn.1002-3674.2020.06.039. [16] Francis GS, Cogswell R, Thenappan T. The heterogeneity of heart failure: will enhanced phenotyping be necessary for future clinical trial success?[J]. Jam Coll Cradiol, 2014, 64(17): 1775-1776. DOI: 10.1016/j.jacc.2014.07.978. [17] Louridas GE, Lourida KG. Systems biology and clinical phenotypes of heart failure syndrome[J]. Jam Coll Cradiol, 2015, 65(12): 1269-1270. DOI: 10.1016/j.jacc.2014.12.051. [18] Liza C, Rrffaele M, Franceso B, et al. Echocardiographic phenotype and prognosis in transthyretin cardiac amyloidosis[J]. Eur Heart J, 2020, 41(14): 1439-1447. DOI: 10.1093/eurheartj/ehz905. [19] Lam CSP, Reger VL, Rodeheffer RJ, et al. Cardiac structure and ventricular-vascular function in persons with heart failure and preserved ejection fraction from olmsted county, minnesota[J]. Circulation, 2007, 115(15): 1982-1990. DOI: 10.1161/CIRCULATIONAHA.106.659763. [20] Cohn JN, Ferrari R, Sharpe N, et al. Cardiac remodeling—concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling[J]. Jam Coll Cradiol, 2000, 35(3): 569-582. DOI: 10.1016/s0735-1097(99)00630-0. [21] Goldfinger JZ, Nair AP. Myocardial recovery and the failing heart: medical, device and mechanical methods[J]. Ann Glob Health, 2014, 80(1): 55-60. DOI: 10.1016/j.aogh.2013.12.006. [22] Zhu N, Chen H, Zhao XY, et al. Left atrial diameter in heart failure with left ventricular preserved, mid-range, and reduced ejection fraction[J]. Medicine, 2019, 98(48): e18146. DOI: 10.1097/MD.0000000000018146. [23] Rossi A, Cicoira M, Florea VG, et al. Chronic heart failure with preserved left ventricular ejection fraction: Diagnostic and prognostic value of left atrial size[J]. Int J Cardiol, 2006, 110(3): 386-392. DOI: 10.1016/j.ijcard.2005.08.049. [24] Sardana M, Hashmath Z, Oldland G, et al. Left atrial longitudinal strain, left atrial size and left ventricular remodeling: implications for heart failure and preserved ejection fraction[J]. Eur Heart J, 2018, 39(Suppl 1): 2747. DOI: 10.1093/eurheartj/ehy565.P2747. [25] Manuel MS, Robert ND, Katrina P, et al. Gender and survival in patients with heart failure: interactions with diabetes and aetiology. Results from the MAGGIC individual patient meta-analysis[J]. Eur J Heart Fall, 2014, 14(5): 473-479. DOI: 10.1093/eurjhf/hfs026. [26] Olivetti G, Capasso JM, Meggs LG, et al. Cellular basis of ventricular remodeling after myocardial infarction[J]. Am J Cardiol, 1991, 68(14): 7-16. DOI: 10.1016/0002-9149(91)90256-K. [27] Ahmed MI, Lainscak M, Mujib M, et al. Gender-related dissociation in outcomes in chronic heart failure: reduced mortality but similar hospitalization in women[J]. Int J Cardiol, 2011, 148(1): 36-42. DOI: 10.1016/j.ijcard.2009.10.019. [28] Shotan A, Garty M, Blondhein DS, et al. Atrial fibrillation and long-term prognosis in patients hospitalized for heart failure: results from heart failure survey in Israel (HFSIS)[J]. Eur J Heart Fall, 2010, 31(3): 309-317. DOI: 10.1093/eurheartj/ehp422. [29] Khatibzadeh S, Farzar F, Oliver J, et al. Worldwide risk factors for heart failure: a systematic review and pooled analysis[J]. Int J Cardiol, 2013, 168(2): 1186-1194. DOI: 10.1016/j.ijcard.2012.11.065. [30] 刘颖娴, 方理刚, 陈未, 等. 心房颤动患者右心结构及压力变化研究[J]. 中国心血管杂志, 2015, 20(1): 34-38. DOI: 10.3969/j.issn.1007-5410.2015.01.008.Liu YX, Fang LG, Chen W, et al. Structure and pressure modifications of right heart in patients with atrial fibrillation[J]. Chin J Cardiovasc Med, 2015, 20(1): 34-38. DOI: 10.3969/j.issn.1007-5410.2015.01.008. [31] Ky B, French B, Khan AM, et al. Ventricular-arterial coupling, remodeling, and prognosis in chronic heart failure[J]. Jam Coll Cradiol, 2013, 62(13): 1165-1172. DOI: 10.1016/j.jacc.2013.03.085. [32] Wong M, Staszewsky L, Latini R, et al. Severity of left ventricular remodeling defines outcomes and response to therapy in heart failure: valsartan heart failure trial (Val-HeFT) echocardiographic data[J]. Jam Coll Cradiol, 2004, 43(11): 2022-2027. DOI: 10.1016/j.jacc.2003.12.053. [33] Bax JJ, Schinkel AF, Boersma E, et al. Extensive left ventricular remodeling does not allow viable myocardium to improve in left ventricular ejection fraction after revascularization and is associated with worse long-term prognosis[J]. Circulation, 2004, 110(11 Suppl 1): Ⅱ18-Ⅱ22. DOI: 10.1161/01.CIR.0000138195.33452.b0. -





 下载:
下载: