The risk factors for death in chronic obstructive pulmonary disease patients: a systematic review and Meta-analysis of cohort studies
-
摘要:
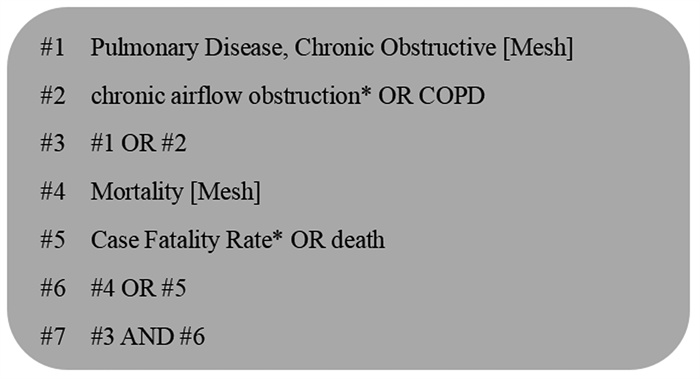
目的 系统评价慢性阻塞性肺疾病(chronic obstructive pulmonary disease, COPD)患者死亡危险因素。 方法 检索PubMed、Cochrane Library、Web of Science、Embase、中国知网、维普网、万方数据知识服务平台和中国生物医学文献数据库有关COPD患者死亡危险因素的研究,再筛选文献、提取数据和质量评价,并进行荟萃分析。 结果 纳入15篇队列研究,纽卡斯尔-渥太华(Newcastle-Ottawa Scale, NOS)量表评分7~9分。荟萃分析结果显示:高龄(HR=1.074, 95% CI: 1.048~1.101, P<0.001)、吸烟(HR=1.390, 95% CI: 1.298~1.490, P<0.001)、低BMI(HR=1.434, 95% CI: 1.190~1.727, P<0.001)、高改良英国医学研究学会呼吸困难指数(modified British medical research council, mMRC)(HR=1.597, 95% CI: 1.550~1.646, P<0.001)、高Charlson共病指数(Charlson comorbidity index, CCI)(HR=1.191, 95% CI: 1.096~1.294, P<0.001)、Ⅳ级COPD(HR=2.114, 95% CI: 1.681~2.658, P<0.001)与COPD患者死亡关联有统计学意义。女性(HR=1.091, 95% CI: 0.781~1.522, P=0.610)、低去脂体重指数(fat free mass index, FFMI)(HR=3.025, 95% CI: 0.268~34.203, P=0.371)与COPD患者死亡关联无统计学意义。描述性分析结果显示高N端脑钠肽前体(N-terminal pro-brain nitric peptide, NT-proBNP)、铜绿假单孢菌(pseudomonas aeruginosa, PA)阳性可能是COPD患者死亡的危险因素。 结论 高龄、吸烟、低BMI、高mMRC、高CCI、Ⅳ级COPD是COPD患者死亡的独立危险因素,女性和低FFMI不是COPD患者死亡的危险因素,高NT-proBNP、PA感染与COPD患者的死亡关系还需进一步研究证明。 Abstract:Objective To systematically review the risk factors for death in chronic obstructive pulmonary disease (COPD) patients. Methods PubMed, Cochrane Library, Web of Science, Embase, CNKI, CBM, VIP and WanFang databases were searched to query the original studies. Then two researchers further screened the studies simultaneously, extracted the data and assessed study quality, and performed Meta-analysis. Results A total of 15 studies were included with Newcastle-Ottawa Scale (NOS) score were among 7 to 9. Meta-analysis showed that elderly people (HR=1.074, 95% CI: 1.048-1.101, P < 0.001), had a high Charlson comorbidity index (CCI) score (HR=1.191, 95% CI: 1.096-1.294, P < 0.001), low BMI (HR=1.434, 95% CI: 1.190-1.727, P < 0.001), smoking (HR=1.390, 95% CI: 1.298-1.490, P < 0.001), had a high modified British medical research council (mMRC) score (HR=1.597, 95% CI: 1.550-1.646, P < 0.001), had Ⅳ COPD (HR=2.114, 95% CI: 1.681-2.658, P < 0.001) were related to the mortality in COPD patients. There was no statistically significant difference between women (HR=1.091, 95% CI: 0.781-1.522, P=0.610), low fat free mass index (FFMI) (HR=3.025, 95% CI: 0.268-34.203, P=0.371) and COPD mortality. Descriptive analysis results showed that high N-terminal pro-brain nitric peptide (NT-proBNP), positive pseudomonas aeruginosa (PA) might be involved in the deaths of COPD patients. Conclusions Among COPD patients, those with advanced age, low BMI, had high CCI and mMRC index score, smoking and those with ⅣCOPO were more likly to have mortality outcomes. And the relationship between high NT-proBNP, PA infection and the mortality in COPD patients still needed further research. -
Key words:
- Chronic obstructive pulmonary disease /
- Death /
- Risk factors /
- Cohort studies /
- Systematic review
-
表 1 纳入研究基本特征
Table 1. Basic characteristics about the literatures
纳入研究及发表年份(年) 国家 数据来源 样本量(n) 男/女(n) 年龄(岁) 随访时间(年) 暴露因素 校正因素 Marco等[10],2019 西班牙 单中心 118 95/23 66.6±9.0 2.00 D、H 年龄、梗阻严重程度 de Blasio等[11],2019 意大利 单中心 210 143/67 — 2.00 H 年龄、性别、6 min步行距离 Ho等[12],2016 中国 单中心 104 98/6 74.2±6.9 3.00 A、D、E 年龄、性别、BMI Martínez-García等[13],2013 西班牙 多中心 201 182/19 70.3±8.9 0.50 A、C、F、H BMI、加重次数 吕志强等[14],2011 中国 单中心 352 287/65 75.0 1.00 C 年龄、性别 Eklöf等[15],2020 丹麦 多中心 22 053 9 868/12 185 69.0 3.00 A、D、E、F 年龄、性别、吸烟 Holmgaard等[16],2013 丹麦 单中心 462 230/232 — 3.00 A、C、D、F、G 年龄、性别、第1 s用力呼气容积 Brekke等[17],2008 挪威 单中心 897 441/456 70.9 2.00 A、B、D 年龄、性别 Morasert等[18],2020 泰国 单中心 358 309/49 — 住院期间 A COPD急性加重期、体温、平均动脉压 Oh等[19],2018 韩国 多中心 629 615/14 — 2.00 A、B、D、F 年龄、性别、BMI Zhang等[20],2020 中国 单中心 829 588/241 — 5.00 A、C 年龄、Charlson综合症 Høiseth等[21],2012 挪威 单中心 99 52/47 71.5±9.0 2.00 A、B BMI、糖尿病、C反应蛋白 Holmgaard等[22],2013 丹麦 单中心 460 — — 5.00 A、B、C、G 年龄、性别、COPD分期 Prudente等[23],2018 巴西 单中心 133 92/41 — 3.00 A、C 年龄、性别、血氧饱和度 Mao等[24],2020 中国 单中心 488 340/148 77.0 0.25 A C反应蛋白、呼吸衰竭 注:暴露因素:A:高龄;B:女性;C:高Charlson合并症指数(Charlson comorbidity index, CCI);D:BMI;E:吸烟;F:高改良英国医学研究学会呼吸困难指数(modified British medical research council, mMRC);G:Ⅳ级COPD;H:低去脂体重指数(fat free mass index, FFMI)。 表 2 纳入研究质量评价
Table 2. Quality evaluation about the literatures
纳入研究 人群选择(分) 组间可比性(分) 结果测量(分) 总分(分) (1) (2) (3) (4) (5) (6) (7) (8) Marco等[10] 1 1 1 1 2 1 1 1 9 de Blasio等[11] 1 0 1 1 2 1 1 1 8 Ho等[12] 1 1 1 1 2 1 1 1 9 Martínez-García等[13] 1 1 1 1 2 1 1 0 8 吕志强等[14] 1 1 1 1 2 1 1 1 9 Eklöf等[15] 1 1 1 1 2 1 1 1 9 Holmgaard等[16] 1 1 1 1 2 1 0 0 7 Brekke等[17] 1 1 1 1 2 1 1 0 8 Morasert等[18] 1 1 1 1 2 1 1 1 9 Oh等[19] 1 1 1 1 2 1 1 0 8 Zhang等[20] 1 1 1 1 2 1 1 1 9 Høiseth等[21] 1 1 1 1 2 1 1 0 8 Holmgaard等[22] 1 1 1 1 2 1 1 1 9 Prudente等[23] 1 1 1 1 2 1 1 1 9 Mao等[24] 1 1 1 1 2 1 1 1 9 注:(1)病例定义与诊断是否准确;(2)病例代表性;(3)对照的选择;(4)对照定义;(5)病例和对照组可比性;(6)暴露的调查和评估;(7)病例和对照的调查;(8)应答率。 表 3 COPD患者死亡危险因素荟萃分析结果
Table 3. The result of Meta-analysis of the risk factors for mortality in the COPD patients
危险因素 纳入研究数(n) 异质检验结果 效应模型 荟萃分析结果 I2值 P值 HR(95%CI)值 P值 高龄 12[13-14, 16-25] 86.9% <0.001 随机效应模型 1.074(1.048~1.101) <0.001 女性 4[17, 20, 22-23] 63.5% 0.041 随机效应模型 1.091(0.781~1.522) 0.610 吸烟 3[13, 16-17] 0.0% 0.752 固定效应模型 1.390(1.298~1.490) <0.001 低BMI 4[11, 13, 17-18] 0.0% 0.448 固定效应模型 1.434(1.190~1.727) <0.001 高mMRC 3[14, 16, 20] 0.0% 0.702 固定效应模型 1.597(1.550~1.646) <0.001 高CCI 5[14, 17, 21, 23-24] 0.0% 0.602 固定效应模型 1.191(1.096~1.294) <0.001 Ⅳ级COPD 2[17, 23] 0.0% 0.762 固定效应模型 2.114(1.681~2.658) <0.001 低FFMI 2[11-12] 81.5% 0.020 随机效应模型 3.025(0.268~34.203) 0.371 表 4 转换效应模型分析与发表偏倚结果
Table 4. Transformation effect model analysis and publication bias results
危险因素 效应模型HR(95%CI)值 Egger’s检验结果 固定效应模型 随机效应模型 t值 P值 高龄 1.058(1.054~1.063) 1.074(1.048~1.101) 1.45 0.177 女性 0.992(0.847~1.163) 1.091(0.781~1.522) 0.74 0.536 吸烟 1.390(1.298~1.490) 1.390(1.298~1.490) -0.33 0.796 低BMI 1.434(1.190~1.727) 1.434(1.190~1.727) 1.73 0.226 高mMRC 1.597(1.550~1.646) 1.597(1.550~1.646) -6.43 0.098 高CCI 1.191(1.096~1.294) 1.191(1.096~1.294) 2.32 0.103 Ⅳ级COPD 2.040(1.681~2.658) 2.040(1.681~2.658) — — 低FFMI 1.222(0.749~1.991) 3.025(0.268~34.203) — — -
[1] WHO. Global health estimates: life expectancy and leading causes of death and disability[EB/OL]. (2020-12-09)[2021-03-25]. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates. [2] 张艳, 刘庆敏, 付文, 等. 2006—2018年浙江省杭州市居民慢性阻塞性肺疾病死亡率变化趋势分析[J]. 疾病监测, 2020, 35(5): 446-450. DOI: 10.3784/j.issn.1003-9961.2020.05.017.Zhang Y, Liu QM, Fu W, et al. Analysis of mortality trend of chronic obstructive pulmonary disease among residents in Hangzhou, Zhejiang Province, 2006-2018[J]. Dis Surveillance, 2020, 35(5): 446-450. DOI: 10.3784/j.issn.1003-9961.2020.05.017. [3] 李正欢, 张晓云, 陈杨, 等. 2020年慢性阻塞性肺疾病全球倡议《COPD诊断、治疗与预防全球策略》指南解读(一)——稳定期药物管理[J]. 中国全科医学, 2021, 24(8): 923-929. DOI: 10.12114/j.issn.1007-9572.2021.00.155.Li ZH, Zhang XY, Chen Y, et al. The global strategy for the diagnosis, treatment andprevention of COPD, the global initiative for chronic obstructive pulmonary disease 2020 south interpretation (1)——stable drug management[J]. Chin Gen Pract, 2021, 24(8): 923-929. DOI: 10.12114/j.issn.1007-9572.2021.00.155. [4] 王弟海, 崔小勇, 龚六堂. 健康在经济增长和经济发展中的作用——基于文献研究的视角[J]. 经济学动态, 2015, (8): 107-127. https://www.cnki.com.cn/Article/CJFDTOTAL-JJXD201508012.htmWang DH, Cui XY, Gong LT. The role of health in economic growth and development——based on the perspective of literature research[J]. Economic Perspectives, 2015, (8): 107-127. https://www.cnki.com.cn/Article/CJFDTOTAL-JJXD201508012.htm [5] Zhi JH, Shan Q, Liang LY, et al. Low skeletal muscle area as a prognostic marker for chronic obstructive pulmonary disease in elderly patients admitted to ICU[J]. Sci Rep, 2019, 9(1): 19117. DOI: 10.1038/s41598-019-55737-z. [6] Maters GA, Voogd JN, Sanderman R, et al. Predictors of all-cause mortality in patients with stable COPD: medical co-morbid conditions or high depressive symptoms[J]. COPD, 2014, 11(4): 468-474. DOI: 10.3109/15412555.2014.898026. [7] Lei S, Li M, Duan W, et al. The long-term outcomes of tobacco control strategies based on thecognitive intervention for smoking cessation in COPD patients[J]. Respir Med, 2020, 172: 106155. DOI: 10.1016/j.rmed.2020.106155. [8] Gan WQ, FitzGerald JM, Carlsten C, et al. Associations of ambient air pollution with chronic obstructive pulmonary disease hospitalization and mortality[J]. Am J Respir Crit Care Med, 2013, 187(7): 721-727. DOI: 10.1164/rccm.201211-2004OC. [9] 朱洁云, 罗毅沣, 王霄玲, 等. BMI与慢性阻塞性肺病患者死亡率相关性的Meta分析[J]. 中国循证医学杂志, 2019, 19(7): 811-817. DOI: 10.7507/1672-2531.201903069.Zhu JY, Luo YP, Wang XL, et al. Meta-analysis of association between BMI and mortality in patients with chronic obstructive pulmonary disease[J]. Chin J Evidence-Based Med, 2019, 19(7): 811-817. DOI: 10.7507/1672-2531.201903069. [10] Marco E, Sánchez-Rodríguez D, Dávalos-Yerovi VN, et al. Malnutrition according to ESPEN consensus predicts hospitalizations and long-term mortality in rehabilitation patients with stable chronic obstructive pulmonary disease[J]. Clin Nutr, 2019, 38(5): 2180-2186. DOI: 10.1016/j.clnu.2018.09.014. [11] de Blasio F, Scalfi L, Di Gregorio A, et al. Raw bioelectrical impedance analysis variables are independent predictors of early all-cause mortality in patients with COPD[J]. Chest, 2019, 155(6): 1148-1157. DOI: 10.1016/j.chest.2019.01.001. [12] Ho SC, Wang JY, Kuo HP, et al. Mid-arm and calf circumferences are stronger mortality predictors than body mass index for patients with chronic obstructive pulmonary disease[J]. Int J Chron Obstruct Pulmon Dis, 2016, 11: 2075-2080. DOI: 10.2147/COPD.S107326. [13] Martínez-García MA, de la Rosa Carrillo D, Soler-Cataluña JJ, et al. Prognostic value of bronchiectasis in patients with moderate-to-severe chronic obstructive pulmonary disease[J]. Am J Respir Crit Care Med, 2013, 187(8): 823-831. DOI: 10.1164/rccm.201208-1518OC. [14] 吕志强, 陈芸, 张蔚. 慢性阻塞性肺疾病急性加重患者的预后影响因素[J]. 中国医师杂志, 2011, 13(12): 1611-1614, 1620. DOI: 10.3760/cma.j.issn.1008-1372.2011.12.008.Lyu ZQ, Chen Y, Zhang W. Prognostic factors in patients with acute exacerbation of chronic obstructive pulmonary disease[J]. J Chin Physician, 2011, 13(12): 1611-1614, 1620. DOI: 10.3760/cma.j.issn.1008-1372.2011.12.008. [15] Eklöf J, Sørensen R, Ingebrigtsen TS, et al. Pseudomonas aeruginosa and risk of death and exacerbations in patients with chronic obstructive pulmonary disease: an observational cohort study of 22053 patients[J]. Clin Microbiol Infect, 2020, 26(2): 227-234. DOI: 10.1016/j.cmi.2019.06.011. [16] Holmgaard DB, Mygind LH, Titlestad IL, et al. Serum vitamin D in patients with chronic obstructive lung disease does not correlate with mortality-results from a 10-year prospective cohort study[J]. PLoS One, 2013, 8(1): e53670. DOI: 10.1371/journal.pone.0053670. [17] Brekke PH, Omland T, Holmedal SH, et al. Troponin T elevation and long-term mortality after chronic obstructive pulmonary disease exacerbation[J]. Eur Respir J, 2008, 31(3): 563-570. DOI: 10.1183/09031936.00015807. [18] Morasert T, Jantarapootirat M, Phinyo P, et al. Prognostic indicators for in-hospital mortality in COPD with acute exacerbation in Thailand: a retrospective cohort study[J]. BMJ Open Respir Res, 2020, 7(1): e000488. DOI: 10.1136/bmjresp-2019-000488. [19] Oh YM, Lee KS, Hong Y, et al. Blood eosinophil count as a prognostic biomarker in COPD[J]. Int J Chron Obstruct Pulmon Dis, 2018, 13: 3589-3596. DOI: 10.2147/COPD.S179734. [20] Zhang Y, Liang LR, Zhang S, et al. Blood eosinophilia and its stability in hospitalized COPD exacerbations are associated with lower risk of all-cause mortality[J]. Int J Chron Obstruct Pulmon Dis, 2020, 15: 1123-1134. DOI: 10.2147/COPD.S245056. [21] Høiseth AD, Omland T, Hagve TA, et al. NT-proBNP independently predicts long term mortality after acute exacerbation of COPD-a prospective cohort study[J]. Respir Res, 2012, 13(1): 97. DOI: 10.1186/1465-9921-13-97. [22] Holmgaard DB, Mygind LH, Titlestad I, et al. Calprotectin-a marker of mortality in COPD? Results from a prospective cohort study[J]. COPD, 2013, 10(5): 581-587. DOI: 10.3109/15412555.2013.781580. [23] Prudente R, Franco EAT, Mesquita CB, et al. Predictors of mortality in patients with COPD after 9 years[J]. Int J Chron Obstruct Pulmon Dis, 2018, 13: 3389-3398. DOI: 10.2147/COPD.S174665. [24] Mao WP, Wang J, Zhang LM, et al. Serum β2-microglobulin is associated with mortalityin hospitalized patients with exacerbated chronic obstructive pulmonary disease[J]. Int J Chron Obstruct Pulmon Dis, 2020, 15: 723-732. DOI: 10.2147/COPD.S243905. [25] 罗文婷, 林艺兰. 厦门市慢性阻塞性肺疾病死亡率的影响因素[J]. 职业与健康, 2016, 32(10): 1376-1378. DOI: 10.13329/j.cnki.zyyjk.2016.0388.Luo WT, Lin YL. Factors influencing mortality of chronic obstructive pulmonary disease in Xiamen City[J]. Occupation Health, 2016, 32(10): 1376-1378. DOI: 10.13329/j.cnki.zyyjk.2016.0388. [26] 徐刚, 鄢艳兰, 黄久玲, 等. 吸烟对中老年人癌症和慢性阻塞性肺疾病的归因分析[J]. 中国老年学杂志, 2016, 36(20): 5148-5150. DOI: 10.3969/j.issn.1005-9202.2016.20.100.Xu G, Yan YL, Huang JL, et al. Attributive analysis of smoking on cancer and chronic obstructive pulmonary disease in middle-aged and elderly people[J]. Chin J Gerontol, 2016, 36(20): 5148-5150. DOI: 10.3969/j.issn.1005-9202.2016.20.100. [27] 谢梅, 刘春红, 刘艳琴. 老年慢性阻塞性肺疾病住院病人的营养水平及肺功能分析[J]. 实用老年医学, 2019, 33(10): 1012-1015. doi: 10.3969/j.issn.1003-9198.2019.10.021Xie M, Liu CH, Liu YQ. Analysis of nutritional level and pulmonary function in elderly inpatients with chronic obstructive pulmonary disease[J]. Pract Geriatr, 2019, 33(10): 1012-1015. doi: 10.3969/j.issn.1003-9198.2019.10.021 [28] 陈淑娟, 闻立新, 金兵, 等. 不同体质量指数慢性阻塞性肺疾病急性加重期老年患者肺功能及血清细胞因子水平的差异[J]. 实用医学杂志, 2020, 36(24): 3349-3352. DOI: 10.3969/j.issn.1006-5725.2020.24.009.Chen SJ, Wen LX, Jin B, et al. Differences of lung function and serum cytokine levels in elderly patients with acute exacerbation of chronic obstructive pulmonary disease with different body mass indexes[J]. The J Pract Med, 2020, 36(24): 3349-3352. DOI: 10.3969/j.issn.1006-5725.2020.24.009. [29] 陈茂辉. 慢性阻塞性肺疾病患者呼吸困难与肺功能的相关性研究[J]. 临床和实验医学杂志, 2008, 7(6): 107-108. DOI: 10.3969/j.issn.1671-4695.2008.06.066.Chen MH. Correlation between dyspnea and lung function in patients with chronic obstructive pulmonary disease[J]. J Clin and Exper Med, 2008, 7(6): 107-108. DOI: 10.3969/j.issn.1671-4695.2008.06.066. [30] 漆波, 张鹤, 李国智, 等. 慢性阻塞性肺疾病急性加重患者住院死亡影响因素研究[J]. 中国呼吸与危重监护杂志, 2013, 12(1): 24-28. DOI: 10.7507/1671-6205.20130006.Qi B, Zhang H, Li GZ, et al. Study on influencing factors of death in patients with acute exacerbation of chronic obstructive pulmonary disease[J]. Chin J Respiratory and Critical Care, 2013, 12(1): 24-28. DOI: 10.7507/1671-6205.20130006. [31] 雷亚军, 李军, 张利娟, 等. 慢性阻塞性肺疾病稳定期患者5年预后的队列研究[J]. 中国临床研究, 2014, 27(9): 1046-1048, 1052. DOI: 10.13429/j.cnki.cjcr.2014.09.004.Lei YJ, Li J, Zhang LJ, et al. A cohort study of 5-year outcomes in patients with stablechronic obstructive pulmonary disease[J]. Chin J Clin Res, 2014, 27(9): 1046-1048, 1052. DOI: 10.13429/j.cnki.cjcr.2014.09.004. [32] 留永健, 田欣伦, 郭兮恒, 等. 慢性阻塞性肺疾病合并焦虑抑郁患病调查[J]. 中国呼吸与危重监护杂志, 2020, 19(5): 425-429. DOI: 10.7507/1671-6205.202001049.Liu YJ, Tian XL, Guo XH, et al. Chronic obstructive pulmonary disease with anxiety and depression[J]. Chin J Respiratory and Critical Care, 2020, 19(5): 425-429. DOI: 10.7507/1671-6205.202001049. -





 下载:
下载: