Mediating effect of body mass index and waist circumference on the relationship between obstructive sleep apnea and type 2 diabetes
-
摘要:
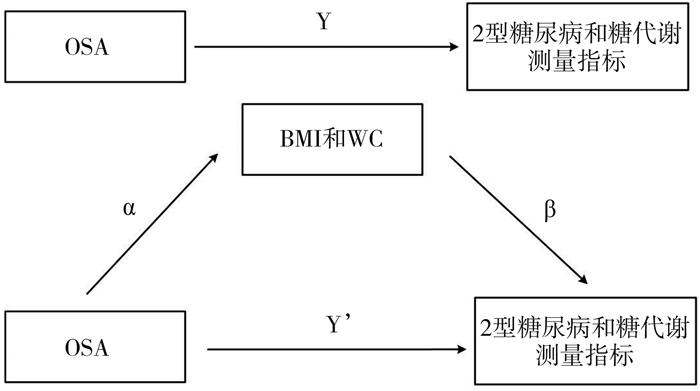
目的 探究BMI和腰围(waist circumference, WC)对阻塞性睡眠呼吸暂停(obstructive sleep apnea, OSA)与2型糖尿病、糖代谢连续测量指标之间的中介效应。 方法 纳入分析的1 615名研究对象来自动脉粥样硬化多民族研究(Multi-Ethnic Study of Atherosclerosis, MESA)。OSA评价指标为呼吸暂停低通气指数(apnea-hypopnea index,AHI),由多导睡眠图测定。糖代谢连续测量指标包括FPG和糖化血红蛋白(glycated hemoglobin,HbA1c)。肥胖指标包括全身肥胖指标BMI和腹型肥胖指标WC。 结果 OSA与2型糖尿病显著相关,后者的患病风险随OSA严重程度增加而升高(P < 0.001)。BMI和WC均介导重度OSA与2型糖尿病之间的关联,其中腹型肥胖指标WC的中介效应为1.296(95% CI: 1.182~1.466),中介效应比例为56.397%;BMI的中介效应为1.291(95% CI: 1.173~1.479),中介效应比例为55.400%。BMI和WC同样介导重度OSA与FPG、HbA1c之间的关联。 结论 OSA与2型糖尿病、FPG和HbA1c的关系,与肥胖程度增加有关。提示OSA患者通过早期的体重干预,特别是控制腹型肥胖对降低糖尿病和心血管并发症的患病率具有重要意义。 -
关键词:
- 阻塞性睡眠呼吸暂停综合征 /
- 2型糖尿病 /
- 中介效应 /
- 肥胖
Abstract:Objective To evaluate the mediating effect of BMI and waist circumference (WC)on the relationships between obstructive sleep apnea (OSA) and type 2 diabetes and continuous measures of glucose metabolism. Methods A total of 1 615 participants from the Multi-Ethnic Study of Atherosclerosis (MESA) were included in this cross-sectional study. OSA severity was assessed by apnea-hypopnea index (AHI), which was measured by polysomnography. Continuous measures of glucose metabolism were FPG and glycated hemoglobin (HbA1c). And obesity indexes used in this study included general obesity (BMI) and abdominal obesity (WC). Results OSA was significantly associated with type 2 diabetes. With increasing the severity of OSA, there was a significant increase in the risk of type 2 diabetes (P < 0.001). Mediation analysis showed that BMI and WC mediated the association between severe OSA and type 2 diabetes, respectively. The indirect effect mediated by WC and BMI were 1.296 (95% CI: 1.182-1.466) and 1.291 (95% CI: 1.173-1.479), and the proportion of mediation were 56.397% and 55.400%, respectively. Similarly, BMI and WC mediated the associations between OSA and FPG and HbA1c. Conclusions These findings show that the associations between OSA and type 2 diabetes, FPG and HbA1c are mediated by obesity indexes to a large proportion. It is suggested that weight control, especially reducing abdominal obesity, may have an important role for OSA patients in decreasing the risk of type 2 diabetes and related cardiovascular complications. -
Key words:
- Obstructive sleep apnea syndrome /
- Type 2 diabetes /
- Mediation analysis /
- Obesity
-
表 1 研究对象的一般特征
Table 1. General characteristics of participants
变量 全部样本
(N=1 615)2型糖尿病 χ2/Z b P值a 否(n=1 301) 是(n=314) 年龄[M(P25, P75), 岁] 67(61, 75) 67(60, 75) 68(62, 76) 1.763 0.078 性别[n(%)] 1.399 0.237 男 790(48.92) 627(48.19) 163(51.91) 女 825(51.08) 674(51.81) 151(48.09) 种族/民族[n(%)] 48.586 < 0.001 白人 591(36.59) 523(40.20) 68(21.66) 美国华裔 203(12.57) 171(13.14) 32(10.19) 黑人或美国非裔 447(27.68) 329(25.29) 118(37.58) 西班牙人 374(41.56) 278(21.37) 96(30.57) 饮酒[n(%)] 725(44.89) 615(47.27) 110(35.03) 15.317 < 0.001 吸烟情况[n(%)] 6.967 0.031 从未吸烟 750(46.44) 610(46.89) 140(44.59) 曾经吸烟 759(47.00) 616(47.35) 143(45.54) 现在吸烟 106(6.56) 75(5.76) 31(9.87) 身体活动水平
[M(P25, P75), MET-min/周]3 660(1 740, 7 200) 3 780(1 830, 7 360) 3 105(1 350, 6 570) -2.814 0.005 eGFR
[M(P25, P75), ml·min-1·1.73m-2]82.93(69.16, 93.40) 82.93(70.27, 93.08) 82.95(63.77, 94.51) -0.648 0.517 TG[M(P25, P75), mg/dl] 95(70, 129) 93(68, 124) 105(78, 143) 4.383 < 0.001 TC[M(P25, P75), mg/dl] 182(157, 206) 186(163, 208) 158(135, 188) -10.733 < 0.001 HDL-C[M(P25, P75), mg/dl] 53(44, 64) 54(45, 66) 49(41, 57) -6.572 < 0.001 LDL-C[M(P25, P75), mg/dl] 103(82, 127) 108(88, 129) 83(66, 111) -10.322 < 0.001 高血压[n(%)] 908(56.22) 668(51.35) 240(76.43) 64.685 < 0.001 充血性心力衰竭[n(%)] 44(2.72) 24(1.84) 20(6.37) 19.540 < 0.001 心肌梗死[n(%)] 54(3.34) 38(2.92) 16(5.10) 3.702 0.054 中风[n(%)] 42(2.60) 31(2.38) 11(3.50) 1.254 0.263 注:连续变量表示为中位数和四分位间距,分类变量为频数和构成比;a表示是否患2型糖尿病两组比较的P值。b Z值为连续变量组间比较采用Wilcoxon秩和检验的统计量,χ2为分类变量组间比较采用Pearson χ2检验的统计量。 表 2 研究对象的OSA、肥胖指标和糖代谢测量指标差异
Table 2. Characteristics of participants with OSA, obesity indexes and measures of glucose metabolism
变量 全部样本
(N=1 615)2型糖尿病 χ2/Z b值 P值a 否(n=1 301) 是(n=314) OSA[n(%)] 1 135(70.28) 887(68.18) 248(78.98) 14.132 < 0.001 AHI < 5 480(29.72) 414(31.82) 66(21.02) 28.854 < 0.001 5≤AHI < 15 542(33.56) 448(34.44) 94(29.94) 15≤AHI < 30 325(20.12) 246(18.91) 79(25.16) AHI≥30 268(16.59) 193(14.83) 75(23.89) 肥胖指标[M(P25, P75)] BMI(kg/m2) 27.83(24.73, 31.61) 27.41(24.38, 30.82) 30.50(26.91, 34.45) 8.562 < 0.001 WC(cm) 98.00(89.50, 107.20) 96.80(88.50, 105.10) 104.15(96.00, 114.50) 8.970 < 0.001 糖代谢测量指标[M(P25, P75)] FPG(mg/dl) 95.00(88.00, 105.00) 93.00(87.00, 100.00) 122.00(103.00, 143.00) 19.329 < 0.001 HbA1c c(%) 5.80(5.50, 6.20) 5.70(5.40, 5.90) 6.70(6.20, 7.50) 22.497 < 0.001 注:aP值表示是否患2型糖尿病两组间比较的结果;bZ值为连续变量组间比较采用Wilcoxon秩和检验的统计量,χ2为分类变量组间比较采用Pearson χ2检验的统计量;cHbA1c:全部样本(N=1 611),非2型糖尿病(n=1 299),2型糖尿病(n=312)。 表 3 不同AHI水平与2型糖尿病的关系
Table 3. Association between different levels of AHI and type 2 diabetes
2型糖尿病 AHI[OR (95% CI)值] P趋势值 AHI < 5 5≤AHI < 15 15≤AHI < 30 AHI≥30 模型1 1.000 1.316(0.935~1.853) 2.014(1.401~2.896) 2.438(1.680~3.537) < 0.001 模型2 1.000 1.263(0.891~1.791) 1.872(1.289~2.719) 2.226(1.511~3.280) < 0.001 模型3 1.000 1.281(0.886~1.851) 1.851(1.245~2.753) 2.188(1.446~3.312) < 0.001 注:模型1单变量模型;模型2校正年龄,性别和种族/民族;模型3在模型2的基础上校正饮酒、吸烟、身体活动水平、eGFR、TC、LDL-C、高血压、充血性心力衰竭、心肌梗死和中风。 表 4 重度OSA(AHI≥30)与2型糖尿病、糖代谢测量指标之间的关系
Table 4. Association between severe OSA (AHI≥30) and type 2 diabetes and measures of glucose metabolism
AHI≥30 2型糖尿病 FPG HbA1c OR(95% CI)值 P值 β(95% CI)值 P值 β(95% CI)值 P值 模型1 1.802(1.328~2.427) < 0.001 0.072(0.045~0.098) < 0.001 0.041(0.025~0.058) < 0.001 模型2 1.676(1.223~2.281) 0.001 0.061(0.035~0.087) < 0.001 0.040(0.024~0.056) < 0.001 模型3 1.645(1.173~2.296) 0.004 0.053(0.027~0.079) 0.001 0.037(0.021~0.053) < 0.001 注:模型1单变量模型;模型2校正年龄,性别和种族/民族;模型3在模型2的基础上校正饮酒、吸烟、身体活动水平、eGFR、TC、LDL-C、高血压、充血性心力衰竭、心肌梗死和中风。 表 5 重度OSA(AHI≥30)与肥胖指标的关系
Table 5. Association between severe OSA (AHI≥30) and obesity indexes
AHI≥30 a β(95% CI)值 P值 BMI(kg/m2) 0.114(0.093~0.136) < 0.001 WC(cm) 0.073(0.055~0.090) < 0.001 注:a模型中校正年龄、性别、种族/民族、饮酒、吸烟、身体活动水平、eGFR、TC、LDL-C、高血压、充血性心力衰竭、心肌梗死和中风。 表 6 肥胖对重度OSA(AHI≥30)与2型糖尿病和糖代谢测量指标之间的中介效应
Table 6. The mediating effect of obesity indexes on the relationship between severe obstructive sleep apnea (AHI≥30) with type 2 diabetes and measures of glucose metabolism
肥胖与糖尿病 直接效应
OR(95% CI)值/
β(95% CI)值间接效应
OR(95% CI)值/
β(95% CI)值中介效应
比例(%)BMI(kg/m2) 2型糖尿病 1.306(0.919~1.844) 1.291(1.173~1.479) a 55.400 FPG 0.037(0.009~0.070) a 0.016(0.008~0.020) a 29.614 HbA1c 0.028(0.011~0.046) a 0.009(0.005~0.013) a 23.539 WC(cm) 2型糖尿病 1.297(0.897~1.801) 1.296(1.182~1.466) a 56.397 FPG 0.035(0.008~0.066) a 0.018(0.011~0.027) a 33.843 HbA1c 0.027(0.011~0.045) a 0.010(0.006~0.014) a 26.455 注:2型糖尿病的直接效应和间接效应结果表示为OR (95% CI)值;FPG和HbA1c的直接效应和间接效应结果表示为β (95% CI)值;a OR (95% CI)值不包括1或者β (95% CI)值不包括0,表示P < 0.05。 -
[1] Liu Y, Han J, Ning L, et al. Cognitive function and life quality of patients with moderate-to-severe obstructive sleep apnea-hypopnea syndrome in China [J]. Expert Rev Respir Med, 2021, 15(3): 435-440. DOI: 10.1080/17476348.2021.1852081. [2] Morsy NE, Farrag NS, Zaki NFW, et al. Obstructive sleep apnea: personal, societal, public health, and legal implications [J]. Rev Environ Health, 2019, 34(2): 153-169. DOI: 10.1515/reveh-2018-0068. [3] Morgenstern M, Wang J, Beatty N, et al. Obstructive sleep apnea: an unexpected cause of insulin resistance and diabetes [J]. Endocrinol Metab Clin North Am, 2014, 43(1): 187-204. DOI: 10.1016/j.ecl.2013.09.002. [4] Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition [J]. Diabetes Res Clin Pract, 2019, 157: 107843. DOI: 10.1016/j.diabres.2019.107843. [5] 王志富, 朱苗霞, 王治平. 2型糖尿病患者血糖波动与血管并发症关系的研究进展[J]. 心血管病学进展, 2018, 39(6): 1064-1068. DOI: 10.16806/j.cnki.issn.1004-3934.2018.06.049.Wang ZF, Zhu MX, Wang ZP. Research progress on the relationship between blood glucose fluctuation and vascular complications in patients with type 2 diabetes mellitus [J]. Adv Cardiovasc Dis, 2018, 39(6): 1064-1068. DOI: 10.16806/j.cnki.issn.1004-3934.2018.06.049. [6] Tuomilehto H, Seppa J, Uusitupa M. Obesity and obstructive sleep apnea--clinical significance of weight loss [J]. Sleep Med Rev, 2013, 17(5): 321-329. DOI: 10.1016/j.smrv.2012.08.002. [7] Reutrakul S, Van Cauter E. Interactions between sleep, circadian function, and glucose metabolism: implications for risk and severity of diabetes [J]. Ann N Y Acad Sci, 2014, 1311: 151-173. DOI: 10.1111/nyas.12355. [8] Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design [J]. Am J Epidemiol, 2002, 156(9): 871-881. DOI: 10.1093/aje/kwf113. [9] Chen X, Wang R, Zee P, et al. Racial/Ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA) [J]. Sleep, 2015, 38(6): 877-888. DOI: 10.5665/sleep.4732. [10] Geovanini GR, Wang R, Weng J, et al. Elevations in neutrophils with obstructive sleep apnea: The Multi-Ethnic Study of Atherosclerosis (MESA) [J]. Int J Cardiol, 2018, 257: 318-323. DOI: 10.1016/j.ijcard.2017.10.121. [11] Thomas IC, Takemoto ML, Forbang NI, et al. Associations of recreational and non-recreational physical activity with coronary artery calcium density vs. volume and cardiovascular disease events: the Multi-Ethnic Study of Atherosclerosis [J]. Eur Heart J Cardiovasc Imaging, 2020, 21(2): 132-140. DOI: 10.1093/ehjci/jez271. [12] 《中国高血压防治指南》修订委员会. 中国高血压防治指南(2018年修订版) [J]. 中国心血管杂志, 2019, 24(1): 24-56. https://www.cnki.com.cn/Article/CJFDTOTAL-XIXG201901003.htmAmendment Committee of Guidelines for the Prevention and Treatment of Hypertension. Guidelines for the prevention and treatment of hypertension in China (2018 revised edition) [J]. Chin J Cardiovase Med, 2019, 24(1): 24-56. https://www.cnki.com.cn/Article/CJFDTOTAL-XIXG201901003.htm [13] Ruehland WR, Rochford PD, O'Donoghue FJ, et al. The new AASM criteria for scoring hypopneas: impact on the apnea hypopnea index [J]. Sleep, 2009, 32(2): 150-157. DOI: 10.1093/sleep/32.2.150. [14] Genuth S, Alberti KG, Bennett P, et al. Follow-up report on the diagnosis of diabetes mellitus [J]. Diabetes Care, 2003, 26(11): 3160-3167. DOI: 10.2337/diacare.26.11.3160. [15] Kendzerska T, Gershon AS, Hawker G, et al. Obstructive sleep apnea and incident diabetes. A historical cohort study [J]. Am J Respir Crit Care Med, 2014, 190(2): 218-225. DOI: 10.1164/rccm.201312-2209OC. [16] Wei DYW, Chew M, Sabanayagam C. Obstructive sleep apnoea, other sleep parameters and diabetic retinopathy [J]. Curr Diab Rep, 2021, 21(12): 58. DOI: 10.1007/s11892-021-01425-0. [17] Vanderweele TJ. Mediation analysis: a practitioner's guide [J]. Annu Rev Public Health, 2016, 37: 17-32. DOI: 10.1146/annurev-publhealth-032315-021402. [18] Drager LF, Polotsky VY, O'Donnell CP, et al. Translational approaches to understanding metabolic dysfunction and cardiovascular consequences of obstructive sleep apnea [J]. Am J Physiol Heart Circ Physiol, 2015, 309(7): H1101-H1111. DOI: 10.1152/ajpheart.00094.2015. [19] Tobaldini E, Florelli EM, Solbiati M, et al. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence [J]. Nat Rev Cardiol, 2019, 16(4): 213-224. DOI: 10.1038/s41569-018-0109-6. [20] Poroyko VA, Carreras A, Khalyfa A, et al. Chronic sleep disruption alters gut microbiota, induces systemic and adipose tissue inflammation and insulin resistance in mice [J]. Sci Rep, 2016, 6: 35405. DOI: 10.1038/srep35405. [21] Ciriello J, Moreau JM, Caverson MM, et al. Leptin: A potential link between obstructive sleep apnea and obesity [J]. Front Physiol, 2021, 12: 767318. DOI: 10.3389/fphys.2021.767318. [22] Nigro E, Scudiero O, Monaco ML, et al. New insight into adiponectin role in obesity and obesity-related diseases [J]. Biomed Res Int, 2014, 2014: 658913. DOI: 10.1155/2014/658913. [23] Zhang FL, Ren JX, Zhang P, et al. Strong association of waist circumference (WC), body mass index (BMI), waist-to-height ratio (WHtR), and waist-to-hip ratio (WHR) with diabetes: a population-based cross-sectional study in Jilin Province, China [J]. J Diabetes Res, 2021, 2021: 8812431. DOI: 10.1155/2021/8812431. [24] Brown RE, Kuk JL, Libma I, et al. Associations between visceral fat and liver fat with insulin sensitivity and metabolic risk in obese adolescents [J]. Biochem Cell Biol, 2015, 93(5): 466-471. DOI: 10.1139/bcb-2014-0064. [25] Samuel VT, Shulman GI. Mechanisms for insulin resistance: common threads and missing links [J]. Cell, 2012, 148(5): 852-871. DOI: 10.1016/j.cell.2012.02.017. [26] Kosseifi S, Bailey B, Price R, et al. The association between obstructive sleep apnea syndrome and microvascular complications in well-controlled diabetic patients [J]. Mil Med, 2010, 175(11): 913-916. DOI: 10.7205/milmed-d-10-00131. -





 下载:
下载: