The common genetic characteristics and molecular mechanisms of systemic lupus erythematosus and primary Sjogren's syndrome
-
摘要:
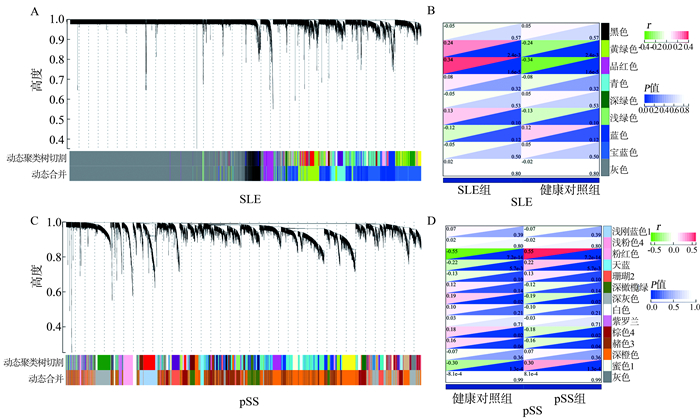
目的 初步探究系统性红斑狼疮(systemic lupus erythematosus, SLE)和原发性干燥综合征(primary Sjögren’s syndrome, pSS)的共同基因表达特征和分子机制。 方法 利用基因表达综合数据库(Gene Expression Omnibus, GEO)获取SLE和pSS基因表达数据集,进行加权基因共表达网络分析(weighted gene co-expression network analysis, WGCNA)和差异表达基因分析(differentially expressed genes, DEGs),初步确认SLE和pSS的共同关键基因和基因表达特征。 结果 WGCNA和DEGs分析结果都显示SLE和pSS的共同基因主要富集在Ⅰ型干扰素(interferon, IFN)和病毒免疫相关的通路上(均有P<0.05);分析得到9个关键基因,分别是ISG15、IFIT3、OASL、OAS2、SERPING1、GBP1、DDX60、XAF1和DDX58,其中大部分是Ⅰ型IFN相关基因。 结论 研究结果提示SLE和pSS的共同基因表达特征主要与Ⅰ型IFN和病毒免疫相关基因以及通路有关,这为未来的机制研究提供了一定的参考。 -
关键词:
- 系统性红斑狼疮 /
- 原发性干燥综合征 /
- Ⅰ型干扰素 /
- 加权基因共表达网络分析 /
- 差异表达基因分析
Abstract:Objective To initially investigate the common gene expression characteristic and molecular mechanism of systemic lupus erythematosus (SLE) and primary Sjögren's syndrome (pSS). Methods The SLE and pSS gene expression datasets were obtained from the Gene Expression Omnibus (GEO) database. Weighted gene co-expression network analysis (WGCNA) and differentially expressed genes (DEGs) were performed on the data to preliminarily identify the common key genes and gene expression characteristics of SLE and pSS. Results Both WGCNA and DEGs analysis showed that the common genes of SLE and pSS were mainly enriched in type Ⅰ interferon (IFN) and viral immune-related pathways (all P < 0.05). The analysis identified nine key genes, namely ISG15, IFIT3, OASL, OAS2, SERPING1, GBP1, DDX60, XAF1, and DDX58, most of which were type Ⅰ IFN-related genes. Conclusion The findings suggest that the common gene expression signatures of SLE and pSS are mainly related to type Ⅰ IFN and viral immune-related genes and pathways, which will provide some reference for future mechanistic studies. -
表 1 GEO数据集基本信息
Table 1. The basic information of GEO datasets
GSE编号 平台 病例(n) 对照(n) 样本类型 疾病类型 分组 GSE110174 GPL13158 144 10 全血 SLE 研究组 GSE66795 GPL10558 131 29 全血 pSS 研究组 GSE20864 GPL570 21 45 全血 SLE 验证组 GSE51092 GPL6884 190 32 全血 pSS 验证组 -
[1] Theofilopoulos AN, Dixon FJ. Murine models of systemic lupus erythematosus[J]. Adv Immunol, 1985, 37: 269-390. DOI: 10.1016/s0065-2776(08)60342-9. [2] Kotzin BL. Systemic lupus erythematosus[J]. Cell, 1996, 85(3): 303-306. DOI: 10.1016/s0092-8674(00)81108-3. [3] Davidson A, Diamond B. Autoimmune diseases[J]. N Engl J Med, 2001, 345(5): 340-350. DOI: 10.1056/NEJM200108023450506. [4] Wakeland EK, Liu K, Graham RR, et al. Delineating the genetic basis of systemic lupus erythematosus[J]. Immunity, 2001, 15(3): 397-408. DOI: 10.1016/s1074-7613(01)00201-1. [5] Miller GW, Nussenzweig V. A new complement function: solubilization of antigen-antibody aggregates[J]. Proc Natl Acad Sci U S A, 1975, 72(2): 418-422. DOI: 10.1073/pnas.72.2.418. [6] Izmirly PM, Wan I, Sahl S, et al. The incidence and prevalence of systemic lupus erythematosus in New York County (Manhattan), New York: the Manhattan lupus surveillance program[J]. Arthritis Rheumatol, 2017, 69(10): 2006-2017. DOI: 10.1002/art.40192. [7] Fox RI. Sjögren's syndrome[J]. Lancet, 2005, 366(9482): 321-331. DOI: 10.1016/s0140-6736(05)66990-5. [8] Hansen A, Lipsky PE, Dörner T. Immunopathogenesis of primary Sjögren's syndrome: implications for disease management and therapy[J]. Curr Opin Rheumatol, 2005, 17(5): 558-565. DOI: 10.1097/01.bor.0000172801.56744.c3. [9] Kassan SS, Moutsopoulos HM. Clinical manifestations and early diagnosis of Sjögren syndrome[J]. Arch Intern Med, 2004, 164(12): 1275-1284. DOI: 10.1001/archinte.164.12.1275. [10] Ramos-Casals M, Brito-Zerón P, Sisó-Almirall A, et al. Primary sjogren syndrome[J]. BMJ, 2012, 344: e3821. DOI: 10.1136/bmj.e3821. [11] Brito-Zerón P, Baldini C, Bootsma H, et al. Sjögren syndrome[J]. Nat Rev Dis Primers, 2016, 2: 16047. DOI: 10.1038/nrdp.2016.47. [12] Qin B, Wang J, Yang Z, et al. Epidemiology of primary sjögren's syndrome: a systematic review and meta-analysis[J]. Ann Rheum Dis, 2015, 74(11): 1983-1989. DOI: 10.1136/annrheumdis-2014-205375. [13] Stefanski AL, Tomiak C, Pleyer U, et al. The diagnosis and treatment of sjögren's syndrome[J]. Dtsch Arztebl Int, 2017, 114(20): 354-361. DOI: 10.3238/arztebl.2017.0354. [14] Moutsopoulos HM, Webber BL, Vlagopoulos TP, et al. Differences in the clinical manifestations of sicca syndrome in the presence and absence of rheumatoid arthritis[J]. Am J Med, 1979, 66(5): 733-736. DOI: 10.1016/0002-9343(79)91110-0. [15] Yao Q, Altman RD, Wang X. Systemic lupus erythematosus with sjögren syndrome compared to systemic lupus erythematosus alone: a meta-analysis[J]. J Clin Rheumatol, 2012, 18(1): 28-32. DOI: 10.1097/rhu.0b013e31823ecbdf. [16] Alani H, Henty JR, Thompson NL, et al. Systematic review and meta-analysis of the epidemiology of polyautoimmunity in sjögren's syndrome (secondary sjögren's syndrome) focusing on autoimmune rheumatic diseases[J]. Scand J Rheumatol, 2018, 47(2): 141-154. DOI: 10.1080/03009742.2017.1324909. [17] Sieiro Santos C, Moriano Morales C, Álvarez Castro C, et al. Polyautoimmunity in systemic lupus erythematosus: secondary Sjogren syndrome[J]. Z Rheumatol, 2021. DOI: 10.1007/s00393-021-01051-x. [18] Isaacs A, Lindenmann J, Virus interference I. The interferon[J]. Proc R Soc Lond B Biol Sci, 1957, 147(927): 258-267. DOI: 10.1098/rspb.1957.0048. [19] Gallucci S, Lolkema M, Matzinger P. Natural adjuvants: endogenous activators of dendritic cells[J]. Nat Med, 1999, 5(11): 1249-1255. DOI: 10.1038/15200. [20] Lepelley A, Wai T, Crow YJ. Mitochondrial nucleic acid as a driver of pathogenic type Ⅰ interferon induction in Mendelian disease[J]. Front Immunol, 2021, 12: 729-763. DOI: 10.3389/fimmu.2021.729763. [21] Crow MK, Olferiev M, Kirou KA. Type Ⅰ Interferons in Autoimmune Disease[J]. Annu Rev Pathol, 2019, 14: 369-393. DOI: 10.1146/annurev-pathol-020117-043952. [22] Pestka S, Krause CD, Walter MR. Interferons, interferon-like cytokines, and their receptors[J]. Immunol Rev, 2004, 202: 8-32. DOI: 10.1111/j.0105-2896.2004.00204.x. [23] Mavragani CP, Niewold TB, Moutsopoulos NM, et al. Augmented interferon-alpha pathway activation in patients with sjögren's syndrome treated with etanercept[J]. Arthritis Rheum, 2007, 56(12): 3995-4004. DOI: 10.1002/art.23062. [24] Le Bon A, Schiavoni G, D'Agostino G, et al. Type Ⅰ interferons potently enhance humoral immunity and can promote isotype switching by stimulating dendritic cells in vivo[J]. Immunity, 2001, 14(4): 461-470. DOI: 10.1016/s1074-7613(01)00126-1. [25] Hervas-Stubbs S, Perez-Gracia JL, Rouzaut A, et al. Direct effects of type Ⅰ interferons on cells of the immune system[J]. Clin Cancer Res, 2011, 17(9): 2619-2627. DOI: 10.1158/1078-0432.ccr-10-1114. [26] Catalina MD, Bachali P, Geraci NS, et al. Gene expression analysis delineates the potential roles of multiple interferons in systemic lupus erythematosus[J]. Commun Biol, 2019, 2: 140. DOI: 10.1038/s42003-019-0382-x. [27] Gallucci S, Meka S, Gamero AM. Abnormalities of the type Ⅰ interferon signaling pathway in lupus autoimmunity[J]. Cytokine, 2021, 146: 155633. DOI: 10.1016/j.cyto.2021.155633. [28] Crow MK, Kirou KA, Wohlgemuth J. Microarray analysis of interferon-regulated genes in SLE[J]. Autoimmunity, 2003, 36(8): 481-490. DOI: 10.1080/08916930310001625952. [29] Bennett L, Palucka AK, Arce E, et al. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood[J]. J Exp Med, 2003, 197(6): 711-723. DOI: 10.1084/jem.20021553. [30] Niewold TB, Hua J, Lehman TJ, et al. High serum IFN-alpha activity is a heritable risk factor for systemic lupus erythematosus[J]. Genes Immun, 2007, 8(6): 492-502. DOI: 10.1038/sj.gene.6364408. [31] Sriram U, Varghese L, Bennett HL, et al. Myeloid dendritic cells from B6. NZM Sle1/Sle2/Sle3 lupus-prone mice express an IFN signature that precedes disease onset[J]. J Immunol, 2012, 189(1): 80-91. DOI: 10.4049/jimmunol.1101686. [32] Jog NR, Young KA, Munroe ME, et al. Association of Epstein-Barr virus serological reactivation with transitioning to systemic lupus erythematosus in at-risk individuals[J]. Ann Rheum Dis, 2019, 78(9): 1235-1241. DOI: 10.1136/annrheumdis-2019-215361. [33] Gallo PM, Rapsinski GJ, Wilson RP, et al. Amyloid-DNA composites of bacterial biofilms stimulate autoimmunity[J]. Immunity, 2015, 42(6): 1171-1184. DOI: 10.1016/j.immuni.2015.06.002 [34] Azzouz D, Omarbekova A, Heguy A, et al. Lupus nephritis is linked to disease-activity associated expansions and immunity to a gut commensal[J]. Ann Rheum Dis, 2019, 78(7): 947-956. DOI: 10.1136/annrheumdis-2018-214856. [35] Båve U, Nordmark G, Lövgren T, et al. Activation of the type Ⅰ interferon system in primary Sjögren's syndrome: a possible etiopathogenic mechanism[J]. Arthritis Rheum, 2005, 52(4): 1185-1195. DOI: 10.1002/art.20998. [36] Bodewes ILA, Versnel MA. Interferon activation in primary Sjögren's syndrome: recent insights and future perspective as novel treatment target[J]. Expert Rev Clin Immunol, 2018, 14(10): 817-829. DOI: 10.1080/1744666x.2018.1519396. [37] Marketos N, Cinoku I, Rapti A, et al. Type Ⅰ interferon signature in Sjögren's syndrome: pathophysiological and clinical implications[J]. Clin Exp Rheumatol, 2019, 118(3): 185-191. [38] Meyer O. Interferons and autoimmune disorders[J]. Joint Bone Spine, 2009, 76(5): 464-473. DOI: 10.1016/j.jbspin.2009.03.012. [39] Provost TT. Anti-Ro(SSA) and anti-La(SSB) antibodies in lupus erythematosus and Sjögren's syndrome[J]. Keio J Med, 1991, 40(2): 72-77. DOI: 10.2302/kjm.40.72. [40] Alexander EL, Malinow K, Lejewski JE, et al. Primary Sjögren's syndrome with central nervous system disease mimicking multiple sclerosis[J]. Ann Intern Med, 1986, 104(3): 323-330. DOI: 10.7326/0003-4819-104-3-323. [41] Pease CT, Shattles W, Barrett NK, et al. The arthropathy of Sjögren's syndrome[J]. Br J Rheumatol, 1993, 32(7): 609-613. DOI: 10.1093/rheumatology/32.7.609. [42] Baechler EC, Batliwalla FM, Karypis G, et al. Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus[J]. Proc Natl Acad Sci U S A, 2003, 100(5): 2610-2615. DOI: 10.1073/pnas.0337679100. [43] Farkas L, Beiske K, Lund-Johansen F, et al. Plasmacytoid dendritic cells (natural interferon- alpha/beta-producing cells) accumulate in cutaneous lupus erythematosus lesions[J]. Am J Pathol, 2001, 159(1): 237-243. DOI: 10.1016/s0002-9440(10)61689-6. [44] Merrill JT, Furie R, Werth VP, et al. Anifrolumab effects on rash and arthritis: impact of the type Ⅰ interferon gene signature in the phase Ⅱb MUSE study in patients with systemic lupus erythematosus[J]. Lupus Sci Med, 2018, 5(1): e000284. DOI: 10.1136/lupus-2018-000284. [45] Kabeerdoss J, Sandhya P, Danda D. Y RNA derived small RNAs in Sjögren's syndrome: Candidate biomarkers?[J]. Int J Rheum Dis, 2017, 20(11): 1763-1766. DOI: 10.1111/1756-185X.13229. [46] Jiang J, Zhao M, Chang C, et al. Type Ⅰ interferons in the pathogenesis and treatment of autoimmune diseases. Clin Rev Allergy Immunol, 2020, 59(2): 248-272. DOI: 10.1007/s12016-020-08798-2. [47] Roger G, Pavot A, Bonnet I, et al. Phenotypic switch from non-active primary Sjögren's syndrome to severe systemic lupus erythematosus after COVID-19 infection in an elderly man[J]. Joint Bone Spine, 2021, 88(6): 105228. DOI: 10.1016/j.jbspin.2021.105228. [48] Totani Y, Demura Y, Ameshima S, et al. A case of lymphocytic interstitial pneumonia with Sjögren's syndrome and systemic lupus erythematosus in which human herpes virus-6 infection was the suspected pathogen[J]. Nihon Kokyuki Gakkai Zasshi, 2001, 39(10): 763-769. -





 下载:
下载: