The effect of chronic disease, disability, and dementia on all-cause mortality among older adults in China: a population-based prospective cohort study
-
摘要:
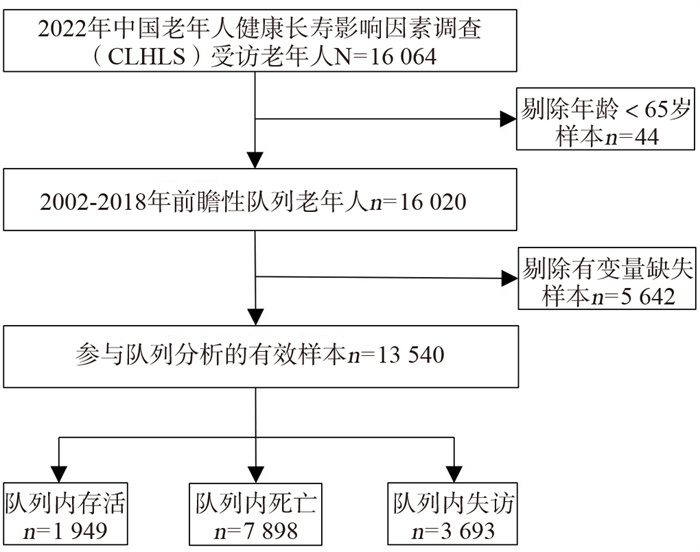
目的 利用基于人群的前瞻性队列研究,分析协同控制后中国老年人慢性病患病、失能和失智对死亡风险的影响。 方法 基于中国老年健康影响因素,跟踪调查2002―2018年共6期数据中13 540位65岁及以上老年人,采用Cox比例风险模型分析慢性病患病、失能和失智与死亡风险的关系。 结果 65岁及以上老年人的生存平均时间为5.75(2.33. 13.00)年。在充分调整混杂因素并协同控制三个维度健康因素后,本研究发现在慢性病患病维度,癌症患者比未患癌症者死亡风险高50%(HR=1.50, 95% CI: 1.16~1.94),而非癌慢性病患病与否与死亡风险的关系差异无统计学意义。在失能维度,日常活动能力受限者比不受限者死亡风险高40%(HR=1.40, 95% CI: 1.32~1.47)。在失智维度,认知受损者相较于未受损者死亡风险高30%(HR=1.30, 95% CI: 1.23~1.37),痴呆患者相较于未患痴呆者死亡风险高26%(HR=1.26, 95% CI: 1.09~1.46)。 结论 在过去20年里,中国老年人健康相关的死亡风险因素主要来自患癌、日常活动能力受限、认知受损和罹患痴呆,提示对于老年人的死亡风险,相较于疾病特别是非癌慢性病患病本身,罹患疾病后的失能与失智尤为值得关注。 Abstract:Objective To analyze the effects of chronic diseases, disability, and dementia on all-cause mortality among older adults in China using a prospective population-based cohort study. Methods Based on 13 540 older adults aged 65 years and above from the Chinese Longitudinal Healthy Longevity Survey, the Cox proportional hazard model was used to analyze the relationship between chronic diseases, disability as well as dementia, and all-cause mortality. Results The median survival time of older adults aged 65 years old and above was 5.75(2.33. 13.00) years. After adjusting for confounders, cancer respondents had a 50% risk of mortality than those without cancer (HR=1.50, 95% CI: 1.16-1.94), while the relationship between noncancerous chronic disease and mortality risk was not statistically significant. With a view to a disability, the mortality risk increased by 40% in subjects with activities of daily living (ADL) restriction than in those without ADL restriction (HR=1.40, 95% CI: 1.32-1.47). In terms of cognitive ability, subjects with cognitive impairment had a 30% higher risk of mortality than those without cognitive impairment (HR=1.30, 95% CI: 1.23-1.37), and those with dementia had a 26% risk of mortality than those without dementia (HR=1.26, 95% CI: 1.09-1.46). Conclusions During the past 20 years, the health factors associated with all-cause mortality risk among older adults in China are mainly cancer, ADL restriction, cognitive impairment, and dementia, suggesting that for the all-cause mortality risk of the older adults, compared with diseases, especially noncancerous chronic diseases themselves, the disability and dementia after suffering from diseases are particularly worthy of attention. -
Key words:
- Older adults /
- Death /
- Chronic diseases /
- Disability /
- Dementia
-
表 1 队列基线受访者的基本特征(N=13 540)
Table 1. Basic characteristics of cohort baseline respondents (N=13 540)
变量 n(%) 变量 n(%) 变量 n(%) 变量 n(%) 人口学特征 婚姻状况 健康及健康行为特征 是否锻炼 年龄(岁) 离异/丧偶/不婚 8 918(65.86) 自评健康与否 否 8 950(66.10) 65~ < 75 3 096(22.87) 已婚 4 622(34.14) 健康 11 312(83.55) 是 4 590(33.90) 75~ < 85 3 383(24.98) 生育孩子数量(个) 不健康 2 228(16.45) 是否经常做家务 85~ < 95 3 746(27.67) 0 558(4.12) 有无抑郁症状 否 6 574(48.55) ≥95 3 315(24.48) 1~2 2 242(16.56) 无 13 492(99.65) 是 6 966(51.45) 性别 3~5 6 247(46.14) 有 48(0.35) 慢性病-失能-失智 女 7 609(56.20) ≥6 4 493(33.18) 是否经常摄入水果 非癌慢性病患病与否 男 5 931(43.80) 受教育年限 否 8 826(65.18) 否 6 466(47.75) 居住地 小学以下 8 109(59.89) 是 4 714(34.82) 是 7 074(52.25) 城镇 6 342(46.84) 小学 3 971(29.33) 是否经常摄入蔬菜 癌症患病与否 农村 7 198(53.16) 中学及以上 1 460(10.78) 否 1 797(13.27) 否 13 484(99.59) 民族 (退休前)职业 是 11 743(86.73) 是 56(0.41) 非汉族 760(5.61) 农民及其他类别 9 789(72.30) 吸烟行为 ADL受限与否 汉族 12 780(94.39) 一般职员类别 2 486(18.36) 从不吸烟 8 721(64.41) 不受限 9 951(73.49) 地区 专业技术人员类别 1 265(9.34) 目前吸烟 2 603(19.22) 受限 3 589(26.51) 东部 8 254(60.96) 是否有退休金 过去吸烟 2 216(16.37) 认知受损与否 中部 3 246(23.97) 否 10 594(78.24) 饮酒行为 未受损 10 636(78.55) 西部 2 040(15.07) 是 2 946(21.76) 从不饮酒 9 004(66.50) 受损 2 904(21.45) 家庭及社会经济特征 收入是否足够生活 目前饮酒 2 866(21.17) 痴呆患病与否 居住安排 否 2 518(18.60) 过去饮酒 1 670(12.33) 否 13 359(98.66) 与他人同住 11 695(86.37) 是 11 022(81.40) 是 181(1.34) 独居 1 845(13.63) 表 2 中国老年人的慢性病患病、失能、失智状况与死亡风险的Cox回归结果(基线n=13 540)
Table 2. Cox regression analysis of chronic diseases, disability, dementia, and all-cause mortality among Chinese older adults (baseline n=13 540)
健康维度 自变量 模型1 模型2 模型3 模型4 HR(95% CI)值 P值 HR(95% CI)值 P值 HR(95% CI)值 P值 HR(95% CI)值 P值 慢性病 非癌慢性病患病与否 < 0.001 0.320 0.717 0.705 否 1.00 1.00 1.00 1.00 是 0.86(0.82~0.90) 0.98(0.93~1.02) 0.99(0.95~1.04) 0.99(0.95~1.04) 癌症患病与否 0.043 0.001 < 0.001 0.002 否 1.00 1.00 1.00 1.00 是 1.30(1.01~1.68) 1.54(1.19~1.99) 1.60(1.24~2.07) 1.50(1.16~1.94) 失能 ADL受限与否 < 0.001 < 0.001 < 0.001 < 0.001 不受限 1.00 1.00 1.00 1.00 受限 2.22(2.11~2.33) 1.58(1.50~1.66) 1.57(1.49~1.65) 1.40(1.32~1.47) 失智 认知受损与否 < 0.001 < 0.001 < 0.001 < 0.001 未受损 1.00 1.00 1.00 1.00 受损 2.01(1.91~2.11) 1.39(1.32~1.47) 1.39(1.31~1.46) 1.30(1.23~1.37) 痴呆患病与否 0.003 < 0.001 < 0.001 0.002 否 1.00 1.00 1.00 1.00 是 1.24(1.08~1.44) 1.30(1.12~1.50) 1.30(1.13~1.50) 1.26(1.09~1.46) 注:模型1仅纳入所有维度健康指标,未调整其他控制变量;模型2=模型1+年龄、性别、居住地、民族和地区;模型3=模型2+居住安排、婚姻状况、生育孩子数量、受教育年限、(退休前)职业、是否有退休金和收入是否足够生活;模型4=模型3+自评健康与否、有无抑郁症状、是否经常摄入水果、是否经常摄入蔬菜、吸烟行为、饮酒行为、是否锻炼和是否经常做家务。 -
[1] Tu H, Wen CP, Tsai SP, et al. Cancer risk associated with chronic diseases and disease markers: prospective cohort study[J]. BMJ, 2018, 360: k134. DOI: 10.1136/bmj.k134. [2] 曹志, 程杨杨, 王媛, 等. 高发慢性病对老年人全因死亡影响的前瞻性研究[J]. 中国慢性病预防与控制, 2020, 28(1): 20-23. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.01.005.Cao Z, Cheng YY, Wang Y, et al. The prospective cohort study for all cause death effects of high incidence chronic diseases on the elderly[J]. Chin J Prevent Control Chron Dis, 2020, 28(1): 20-23. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.01.005. [3] Nakazawa A, Nakamura K, Kitamura K, et al. Association between activities of daily living and mortality among institutionalized elderly adults in Japan[J]. J Epidemiol, 2012, 22(6): 501-507. DOI: 10.2188/jea.JE20110153. [4] Wu CY, Chou YC, Huang N, et al. Cognitive impairment assessed at annual geriatric health examinations predicts mortality among the elderly[J]. Prev Med, 2014, 67: 28-34. DOI: 10.1016/j.ypmed.2014.06.027. [5] Aliberti MJR, Cenzer IS, Smith AK, et al. Assessing risk for adverse outcomes in older adults: the need to include both physical frailty and cognition[J]. J Am Geriatr Soc, 2019, 67(3): 477-483. DOI: 10.1111/jgs.15683. [6] Perna L, Wahl HW, Mons U, et al. Cognitive impairment, all-cause and cause-specific mortality among non-demented older adults[J]. Age Ageing, 2014, 44(3): 445-451. DOI: 10.1093/ageing/afu188. [7] Zeng Y. Chinese Longitudinal Healthy Longevity Survey and some research findings[J]. Geriatr Gerontol Int, 2004, 4: S49-S52. DOI: 10.1111/j.1447-0594.2004.00147.x. [8] Zeng Y, Jr DP, Vlosky DA, et al. Healthy longevity in China : demographic, socioeconomic, and psychological dimensions[J]. Springer Ebooks, 2008, 63(3): 312-313. DOI: 10.1080/00324720903216903. [9] Zeng Y. Towards deeper research and better policy for healthy aging --using the unique data of Chinese longitudinal healthy longevity survey[J]. China Econ J, 2012, 5(2-3): 131-149. DOI: 10.1080/17538963.2013.764677. [10] Katz S, Ford AB, Moskowitz RW, et al. Studies of Illness in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial Function[J]. JAMA, 1963, 185(12): 914-919. DOI: 10.1001/jama.1963.03060120024016. [11] 高明月, 杨珉, 况伟宏, 等. 简易精神状态量表得分的影响因素和正常值的筛查效度评价[J]. 北京大学学报(医学版), 2015, 47(3): 443-449. DOI: 10.3969/j.issn.1671-167X.2015.03.014.Gao MY, Yang M, Kuang WH, et al. Factors and validity analysis of Mini-Mental State Examination in Chinese elderly people[J]. J Peking Univ Health Sci, 2015, 47(3): 443-449. DOI: 10.3969/j.issn.1671-167X.2015.03.014. [12] 易伟宁, 康晓平. 中国高龄老人认知功能影响因素的多水平分析[J]. 中国心理卫生杂志, 2008, 22(7): 538-542. DOI: 10.3321/j.issn:1000-6729.2008.07.019.Yi WN, Kang XP. A Multilevel Analysis on Influential Factors of Cognitive Change among Chinese Oldest-old[J]. Chin Mental Health J, 2008, 22(7): 538-542. DOI: 10.3321/j.issn:1000-6729.2008.07.019. [13] Stein J, Luppa M, Maier W, et al. Assessing cognitive changes in the elderly: Reliable Change Indices for the Mini-Mental State Examination[J]. Acta Psychiatr Scand, 2012, 126(3): 208-218. DOI: 10.1111/j.1600-0447.2012.01850.x. [14] Yang HL, Li FR, Chen PL, et al. Tooth Loss, Denture use and cognitive impairment in Chinese oder adults: A community cohort study[J]. J Gerontol A Biol Sci Med Sci, 2022, 77(1): 180-187. DOI: 10.1093/gerona/glab056. [15] Zhang MY, Katzman R, Salmon D, et al. The prevalence of dementia and Alzheimer's disease in Shanghai, China: impact of age, gender, and education[J]. Ann Neurol, 1990, 27(4): 428-437. DOI: 10.1002/ana.410270412. [16] Feng Q, Son J, Zeng Y. Prevalence and correlates of successful ageing: a comparative study between China and South Korea[J]. Eur J Ageing, 2014, 12(2): 83-94. DOI: 10.1007/s10433-014-0329-5. [17] Shen K, Zhang B, Feng Q. Association between tea consumption and depressive symptom among Chinese older adults[J]. BMC Geriatr, 2019, 19(1): 246. DOI: 10.1186/s12877-019-1259-z. [18] Yi Z, Vaupel J. Association of late childbearing with healthy longevity among the oldest-old in China[J]. Popul Stud (Camb), 2004, 58(1): 37-53. DOI: 10.1080/0032472032000175437. [19] Chen CI, Kuan CF, Miser J, et al. Comorbidity as an independent risk factor in patients with cancer: An 8-year population-based study[J]. Asia Pac J Public Health, 2015, 27(2): NP590-NP599. DOI: 10.1177/1010539513481491. [20] Kvale E, Ekundayo OJ, Zhang Y, et al. History of cancer and mortality in community-dwelling older adults[J]. Cancer Epidemiol, 2011, 35(1): 30-36. DOI: 10.1016/j.canep.2010.07.011. [21] Tsai AC, Lee LC, Wang JY. Complementarity of the mini-nutritional assessment and activities of daily living for predicting follow-up mortality risk in elderly taiwanese[J]. Br J Nutr, 2013, 109(4): 658-666. DOI: 10.1017/S0007114512001730. [22] Ryg J, Engbere H, Mariadas P, et al. Barthel Index at hospital admission is associated with mortality in geriatric patients: a Danish nationwide population-based cohort study[J]. Clin Epidemiol, 2018, 10: 1789-1800. DOI: 10.2147/CLEP.S176035. [23] Wetterberg H, Najar J, Rydén L, et al. Dementia remains the major predictor of death among octogenarians. A study of two population cohorts of 85-year-olds examined 22 years apart[J]. Eur J Epidemiol, 2021, 36(5): 507-517. DOI: 10.1007/s10654-021-00745-5. [24] Ganguli M, Dodge HH, Shen C, et al. Alzheimer disease and mortality: a 15-year epidemiological study[J]. Arch Neurol, 2005, 62(5): 779-784. DOI: 10.1001/archneur.62.5.779. [25] Perruccio AV, Power JD, Badley EM. The relative impact of 13 chronic conditions across three different outcomes[J]. J Epidemiol Community Health, 2007, 61(12): 1056-1061. DOI: 10.1136/jech.2006.047308. [26] Samaras K, Sachdev PS. Diabetes and the elderly brain: sweet memories?[J]. Ther Adv Endocrinol Metab, 2012, 3(6): 189-196. DOI: 10.1177/2042018812469645. [27] Salihović D, Smajlović D, Mijajlović M, et al. Cognitive syndromes after the first stroke[J]. Neurol Sci, 2018, 39(8): 1445-1451. DOI: 10.1007/s10072-018-3447-6. [28] Pathan SS, Gottesman RF, Mosley TH, et al. Association of lung function with cognitive decline and dementia: the Atherosclerosis Risk in Communities (ARIC) Study[J]. Eur J Neurol, 2011, 18(6): 888-898. DOI: 10.1111/j.1468-1331.2010.03340.x. -





 下载:
下载: