Relationship between hemoglobin level in early pregnancy and gestational diabetes mellitus: a birth cohort study
-
摘要:
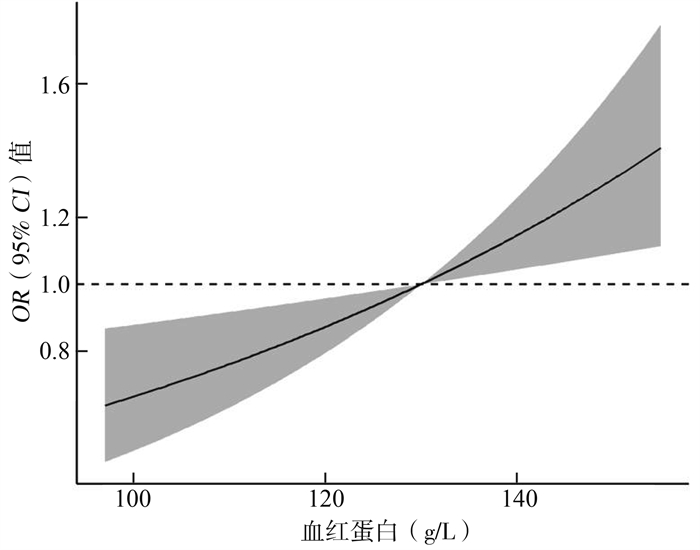
目的 探究中国西北地区孕妇孕早期血红蛋白水平与妊娠期糖尿病(gestational diabetes mellitus, GDM)的关系。 方法 连续纳入2018年7月-2019年7月加入西北妇女儿童医院出生人口队列的孕早期孕妇,调查其基本人口学特征、生活行为方式等资料,并对研究对象的孕早期血红蛋白水平、口服葡萄糖耐量试验(oral glucose tolerance test, OGTT)结果进行随访。首先使用logistic回归分析模型分析孕早期血红蛋白水平对GDM的影响,进一步采用限制性三次立方样条来呈现血红蛋白水平与GDM的非线性关系。 结果 在调整了混杂因素后,孕早期高血红蛋白水平(血红蛋白≥135 g/L)增加了GDM的发生风险(OR=1.44,95% CI:1.13~1.83);孕早期血红蛋白水平每升高10 g/L,FPG、OGTT 1h血糖、OGTT 2h血糖水平分别升高0.03 mmol/L(95% CI:0.01~0.05)、0.14 mmol/L(95% CI:0.07~0.21)、0.13 mmol/L(95% CI:0.08~0.19);限制性立方样条结果显示,随着孕早期血红蛋白水平升高,GDM的发生风险逐渐升高。 结论 孕早期血红蛋白水平升高将增加GDM的发病风险,应积极对孕妇孕早期血红蛋白水平进行监测,促进母婴健康。 Abstract:Objective To investigate the relationship between hemoglobin levels in early pregnancy and gestational diabetes mellitus (GDM) in pregnant women in northwest China. Methods In Northwest Women's and Children's Hospital from July 2018 to July 2019, women in early pregnancy were recruited to birth cohort. A questionnaire was used to collect their basic demographic characteristics and lifestyle behaviors, and to follow up the hemoglobin levels and oral glucose tolerance test (OGTT) in early pregnancy. The association of hemoglobin levels in early pregnancy with GDM was first explored using a logistic regression model, and the nonlinear relationship between hemoglobin levels and GDM was further investigated by restricted cubic splines. Results After adjusting for confounders, high hemoglobin levels (Hb ≥135 g/L) in early pregnancy increased the risk of GDM (OR=1.44, 95% CI: 1.13-1.83). For every 10g/L increase in hemoglobin levels in early pregnancy, FPG, OGTT 1h glucose, and OGTT 2h glucose levels increased by 0.03 mmol/L (95% CI: 0.01-0.05), 0.14 mmol/L (95% CI: 0.07-0.21), and 0.13 mmol/L (95% CI: 0.08-0.19), respectively. The results of the restricted cubic strip showed that the risk of GDM progressively increased with increasing hemoglobin levels in early pregnancy. Conclusions Elevated hemoglobin levels in early pregnancy will increase the risk of GDM. Women hemoglobin levels in early pregnancy should be actively monitored to promote maternal and infant health. -
表 1 研究对象的一般特征(N=2 059)[n(%)]
Table 1. General characteristics of study subjects(N=2 059)[n(%)]
变量 血红蛋白水平(g/L) F/χ2值 P值 < 125(n=668) 125~ < 135(n=701) ≥135(n=690) 年龄(x±s, 岁) 29.38±3.99 29.45±3.38 29.40±3.25 0.073 0.929 育龄妇女受教育程度 2.683 0.262 a 高中及以下 104(15.57) 90(12.84) 98(14.18) 大专及本科 460(68.86) 489(69.76) 488(70.72) 研究生及以上 104(15.57) 122(17.40) 104(15.07) 家庭经济状况 2.932 0.231 a 贫穷(< 5万/家庭年收入) 85(12.72) 79(11.27) 87(12.61) 中等(5~ < 20万/家庭年收入) 448(67.07) 474(67.62) 483(70.00) 富裕(≥20万/家庭年收入) 135(20.21) 148(21.11) 120(17.39) 孕前BMI(kg/m2) 7.293 0.026 a 消瘦 161(24.10) 117(16.69) 104(15.07) 正常 440(65.87) 496(70.76) 451(65.36) 超重 67(10.03) 88(12.55) 135(19.57) 孕期增重(x±s, kg) 14.35±4.02 14.13±4.03 13.31±4.18 12.511 < 0.001 二手烟暴露 7.123 0.028 否 504(75.45) 522(74.47) 553(80.14) 是 164(24.55) 179(25.53) 137(19.86) 产史(次) 0.450 0.799 a 0 540(80.84) 571(81.46) 567(82.17) 1 121(18.11) 123(17.55) 119(17.25) ≥2 7(1.05) 7(0.99) 4(0.58) 人工流产 6.777 0.034 否 561(83.98) 563(80.31) 589(85.36) 是 107(16.02) 138(19.69) 101(14.64) 是否初次妊娠 4.693 0.096 否 299(44.76) 332(47.36) 287(41.59) 是 369(55.24) 369(52.64) 403(58.41) RBC(x±s, ×1012/L) 3.98±0.35 4.30±1.39 4.56±0.26 80.212 < 0.001 HCT(x±s, %) 35.36±2.29 38.44±3.69 41.15±2.08 729.184 < 0.001 注:a秩和检验。 表 2 孕早期血红蛋白水平与GDM单因素分析(N=2 059)
Table 2. Univariate analysis of haemoglobin levels and GDM in early pregnancy (N=2 059)
指标 血红蛋白水平(g/L) F/χ2值 P值 < 125(n=668) 125~ < 135(n=701) ≥135(n=690) GDM[n(%)] 167(25.00) 201(28.67) 225(32.61) 9.591 0.008 FPG(x±s, mmol/L) 4.80±0.45 4.84±0.47 4.87±0.47 3.806 0.022 OGTT 1h血糖(x±s, mmol/L) 7.50±1.70 7.64±1.75 7.88±1.86 7.471 0.001 OGTT 2h血糖(x±s, mmol/L) 6.73±1.30 6.77±1.26 6.98±1.40 6.370 0.002 FPG异常[n(%)] 117(18.93) 154(23.62) 176(27.46) 12.790 0.002 OGTT 1h异常[n(%)] 53(8.59) 64(9.83) 79(12.36) 5.060 0.080 OGTT 2h异常[n(%)] 56(9.06) 50(7.67) 79(12.34) 8.477 0.014 表 3 孕早期血红蛋白水平与GDM多因素分析(N=2 059)
Table 3. Multifactorial analysis of haemoglobin levels and GDM in early pregnancy(N=2 059)
血红蛋白水平 GDM调整OR (95% CI)值 FPG调整β (95% CI)值 OGTT 1h血糖调整β (95% CI)值 OGTT 2h血糖调整β (95% CI)值 血红蛋白水平-每“10g/L” 1.11(1.01~1.22) 0.03(0.01~0.05) 0.14(0.07~0.21) 0.13(0.08~0.19) 血红蛋白水平(g/L)-分组 < 125 1.00 1.00 1.00 1.00 125~ < 135 1.21(0.95~1.54) 0.04(-0.01~0.09) 0.15(-0.04~0.34) 0.03(-0.11~0.17) ≥135 1.44(1.13~1.83) 0.07(0.02~0.12) 0.36(0.17~0.55) 0.23(0.09~0.37) 注:调整了年龄、受教育程度、家庭经济状况、孕前BMI、孕期增重、二手烟暴露、孕次、产次。 -
[1] Du HY, Jiang H, Kamin O, et al. Association of dietary pattern during pregnancy and gestational diabetes mellitus: a prospective cohort study in northern China[J]. Biomed Environ Sci, 2017, 30(12): 887-897. DOI: 10.3967/bes2017.119. [2] Hildén K, Hanson U, Persson M, et al. Gestational diabetes and adiposity are independent risk factors for perinatal outcomes: a population based cohort study in Sweden[J]. Diabet Med, 2019, 36(2): 151-157. DOI: 10.1111/dme.13843. [3] Gortazar L, Flores-Le Roux JA, Benaiges D, et al. Trends in prevalence of gestational diabetes and perinatal outcomes in Catalonia, Spain, 2006 to 2015: the diagestcat study[J]. Diabetes Metab Res Rev, 2019, 35(5): e3151. DOI: 10.1002/dmrr.3151. [4] Zhang ZJ, Zhao G, Yu C, et al. Diabetic women suffer more years of life lost than diabetic men[J]. Int J Endocrinol, 2014, 2014: 208369. DOI: 10.1155/2014/208369. [5] 姚观昀. 血糖控制对妊娠期糖尿病孕妇母婴结局的影响分析[J]. 糖尿病新世界, 2017, 20(19): 66-67, 139. DOI: 10.16658/j.cnki.Yao GY. Influence of blood glucose control on maternal and neonatal outcomes in pregnant women with gestational diabetes mellitus[J]. Diabetes New World, 2017, 20 (19): 66-67, 139. DOI: 10.16658/j.cnki. [6] Granada C, Forbes J, Sangi-Haghpeykar H, et al. Can overt diabetes mellitus be predicted by an early A1C value in gestational diabetics?[J]. J Reprod Med, 2014, 59(7-8): 343-347. [7] Siddappa AM, Rao R, Logn JD, et al. The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations[J]. Neonatology, 2007, 92(2): 73-82. DOI: 10.1159/000100805. [8] Chen X, Scholl TO, Stein TP. Association of elevated serum ferritin levels and the risk of gestational diabetes mellitus in pregnant women: the Camden study[J]. Diabetes Care, 2006, 29(5): 1077-1082. DOI: 10.2337/diacare.2951077. [9] 中华人民共和国卫生部. 妊娠期糖尿病诊断: WS 331-2011[S]. 北京: 中国标准出版社, 2011: 2.Ministry of health of People's Republic of China. Diagnosis of gestational diabetes mellitus: WS 331-2011[S]. Beijing: Standards Press of China, 2011: 2. [10] 中华人民共和国国家卫生和计划生育委员会. 成人体重标准: WS/T 428-2013[S]. 北京: 中国标准出版社, 2013, 3-4.National Health and Family Planning Commission of the People's Republic of China. Criteria of weight for adults: WS/T 428-2013[S]. Beijing: Standards Press of China, 2013, 3-4. [11] Silva-Zolezzi I, Samuel TM, Spieldenner J. Maternal nutrition: opportunities in the prevention of gestational diabetes[J]. Nutr Reviews, 2017, 75(suppl 1): 32-50. DOI: 10.1093/nutrit/nuw033. [12] 关怀, 尚丽新. 妊娠期糖尿病流行现状[J]. 中国实用妇科与产科杂志, 2015, 31(1): 91-94. DOI: 10.7504/fk2014120120.Guan H, Shang LX. Prevalence of gestational diabetes mellitus[J]. Chin J Pract Gynecol Obstetr, 2015, 31(1): 91-94. DOI: 10.7504/fk2014120120. [13] 韩娜, 刘珏, 金楚瑶, 等. 2013-2017年北京市通州区34 637例孕妇妊娠期糖尿病流行情况及其影响因素研究[J]. 中华疾病控制杂志, 2019, 23(2): 156-161. DOI: 10.16462/j.cnki.zhjbkz.2019.02.007.Han N, Liu J, Jin CY, et al. Study on the prevalence of gestational diabetes mellitus and its influencing factors in 34 637 pregnant women in Tongzhou District, Beijing from 2013-2017[J]. Chin J Dis Control, 2019, 23(2): 156-161. DOI: 10.16462/j.cnki.zhjbkz.2019.02.007. [14] 王婧, 陈卓, 马润玫, 等. 昆明地区妊娠早期母体红细胞参数与妊娠期糖尿病的关系[J]. 中华围产医学杂志, 2012, 15(12): 705-709. DOI: 10.3760/cma.j.issn.Wang J, Chen Z, Ma RM, et al. Relationship between maternal erythrocyte parameters and gestational diabetes mellitus in early pregnancy in Kunming Area[J]. Chin J Perinat Med, 2012, 15(12): 705-709. DOI: 10.3760/cma.j.issn. [15] Lao TT, Chan LY, Tam KF, et al. Maternal hemoglobin and risk of gestational diabetes mellitus in Chinese women[J]. Obstet Gynecol, 2002, 99(5 Pt 1): 807-812. DOI: 10.1016/s0029-7844(02)01941-5. [16] Lao TT, Ho LF. Impact of iron deficiency anemia on prevalence of gestational diabetes mellitus[J]. Diabetes Care, 2004, 27(3): 650-656. DOI: 10.2337/diacare.27.3.650. [17] Mehrabian F, Hosseini SM. Comparison of gestational diabetes mellitus and pre-eclampsia in women with high hemoglobin in the first trimester of pregnancy: a longitudinal study[J]. Paki J Med Sci, 2013, 29(4): 986-990. DOI: 10.12669/pjms.294.4012. [18] Zein S, Rachidi S, Awada S, et al. High iron level in early pregnancy increased glucose intolerance[J]. J Trace Elem Med Biol, 2015, 30: 220-225. DOI: 10.1016/j.jtemb.2014.09.004. [19] Helin A, Kinnunen TI, Raitanen J, et al. Iron intake, haemoglobin and risk of gestational diabetes: a prospective cohort study[J]. BMJ Open, 2012, 2(5): e001730. DOI: 10.1136/bmjopen-2012-001730. [20] Bo S, Menato G, Villois P, et al. Iron supplementation and gestational diabetes in midpregnancy[J]. Am J Obstet Gynecol, 2009, 201(2): 158. DOI: 10.1016/j.ajog.2009.04.049. [21] White SL, Pasupathy D, Sattar N, et al. Metabolic profiling of gestational diabetes in obese women during pregnancy[J]. Diabetologia, 2017, 60(10): 1903-1912. DOI: 10.1007/s00125-017-4380-6. [22] Buchanan TA, Xiang A, Kjos SL, et al. What is gestational diabetes?[J]. Diabetes Care, 2007, 30(Suppl 2): s105-s111. DOI: 10.2337/dc07-s201. -





 下载:
下载: