The prevalence and risk factors of gestational diabetes mellitus among 23 896 pregnant women in Chongqing
-
摘要:
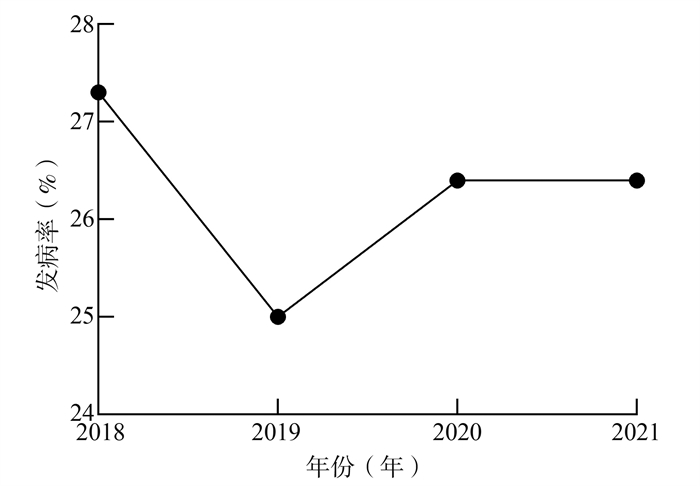
目的 分析重庆市区2018-2021年孕妇妊娠期糖尿病(gestational diabetes mellitus, GDM)的发病现况及其相关危险因素,为GDM的防控提供依据。 方法 收集2018年1月-2021年6月在重庆医科大学附属妇女儿童医院进行产前检查的孕妇临床资料,并采用logistic回归分析模型分析不同危险因素对GDM的影响。 结果 本研究共纳入来自重庆市区23 896名孕妇为研究对象,确诊为GDM的患者有6 269例,占26.2%。2018-2021年GDM的发病率分别为27.3%、25.0%、26.4%和26.4%。多因素logistic回归分析模型分析结果表明,在调整相关变量之后,年龄(OR=1.47, 95% CI: 1.41~1.54, P < 0.001)、BMI (OR=1.74, 95% CI: 1.65~1.83, P < 0.001)和内分泌疾病史(OR=9.32, 95% CI: 8.68~10.01, P < 0.001)是导致GDM患病风险增加的危险因素。 结论 本研究发现重庆市区GDM的发病率较高,且高龄孕妇、孕前超重或肥胖和内分泌疾病史是GDM的高危因素。重庆市区应加强系统性的产科护理,关注孕期这些危险因素的变化,以减少GDM的发生。 Abstract:Objective To analyze the changes in the morbidity gestational diabetes mellitus (GDM) and related risk factors in Chongqing from 2018 to 2021, and provide evidence for prevention and control of gestational diabetes mellitus. Methods Clinical data of pregnant women who attended prenatal care in Women and Children's Hospital of Chongqing Medical University from January 2018 to June 2021 were collected, and 6269 pregnant women were diagnosed with GDM. The incidence of GDM and risk factors were investigated. The multivariate logistic regression was used for statistical analysis. Results A total of 23 896 subjects were included in this study. There were 6 269 pregnant women with GDM, with a ratio of 26.2%, and the incidence rates of GDM in pregnant women from 2018 to 2021 were 27.3%, 25.0%, 26.4%, and 26.4%, respectively. Multivariate logistic regression analysis showed that age (OR=1.47, 95% CI: 1.41-1.54, P < 0.001), BMI (OR=1.74, 95% CI: 1.65-1.83, P < 0.001) and history of endocrine disease (OR=9.32, 95% CI: 8.68-10.01, P < 0.001) were risk factors of GDM. Conclusions The incidence of GDM is relatively high in Chongqing, and advanced maternal age and pre-pregnancy overweight or obesity are high risk factors for GDM. Systematic obstetric care should be intensified in Chongqing and more attention should be paid to changes of these risk factors during pregnancy to reduce the occurrence of GDM. -
Key words:
- Gestational diabetes mellitus /
- Incidence /
- Risk factors
-
表 1 研究对象的基线特征[n(%)]
Table 1. Baseline characteristics of study subjects [n(%)]
变量 2018年 2019年 2020年 2021年 合计 H/χ2值 P值 年龄(岁) 616.54 < 0.001 < 35 4 557(62.6) 5 430(68.5) 5 137(74.3) 1 401(83.8) 16 538(69.2) ≥35 2 723(37.4) 2 495(31.5) 1 775(25.7) 270(16.2) 7 358(30.8) BMI (kg/m2) 85.89 < 0.001 < 25 5 550(82.9) 6 198(83.1) 5 590(85.9) 1 414(79.5) 18 739(83.9) ≥25 1 143(17.1) 1 262(16.9) 917(14.1) 365(20.5) 3 592(16.1) 孕次(次) 12.32 0.006 1 2 353(32.3) 2 588(32.7) 2 338(33.8) 617(34.8) 7 896(33.1) 2 1 966(27.0) 2 169(27.4) 1 918(27.8) 498(28.1) 6 551(27.4) ≥3 2 961(40.7) 3 165(40.0) 2 651(38.4) 658(37.1) 9 435(39.5) 产次(次) 5.58 0.134 0 4 589(63.0) 5 008(63.2) 4 352(63.0) 1 069(60.3) 15 018(62.9) ≥1 2 691(37.0) 2 914(36.8) 2 556(37.0) 704(39.7) 8 865(37.1) 吸烟史 27.85 < 0.001 是 157(2.3) 277(3.5) 217(3.2) 35(2.0) 686(2.9) 否 6 801(97.7) 7 579(96.5) 6 631(96.8) 1 729(98.0) 22 740(95.2) 饮酒史 250.79 < 0.001 是 680(9.4) 1 426(18.3) 1 074(15.8) 240(13.6) 3 420(14.5) 否 6 527(90.6) 6 359(81.7) 5 717(84.2) 1 521(86.4) 20 124(85.5) 是否服用叶酸 1 105.12 < 0.001 是 6 572(90.3) 7 786(98.5) 6 860(99.7) 1 738(98.8) 22 956(96.4) 否 703(9.7) 116(1.5) 24(0.3) 21(1.2) 864(3.4) 内分泌疾病史 56.53 < 0.001 是 1 782(24.5) 1 657(20.9) 1 787(25.9) 449(25.2) 5 675(23.7) 否 5 498(75.5) 6 268(79.1) 5 125(74.1) 1 330(74.8) 18 221(76.3) 多胎妊娠 8.69 0.034 是 349(4.8) 368(4.6) 266(3.8) 77(4.3) 1 060(4.4) 否 6 931(95.2) 7 557(95.4) 6 646(96.2) 1 702(95.7) 22 836(95.6) 巨大儿分娩史 27.14 < 0.001 是 9(0.1) 3(0.0) 26(0.4) 2(0.1) 40(0.2) 否 7 271(99.9) 7 922(100.0) 6 886(99.6) 1 777(99.9) 23 856(99.8) 辅助生殖 10.20 0.017 是 609(8.4) 639(8.1) 484(7.0) 135(7.6) 1 867(7.8) 否 6 671(91.6) 7 286(91.9) 6 428(93.0) 1 644(92.4) 22 029(92.2) 表 2 单因素和多因素logistic回归分析模型分析不同危险因素对GDM发病的影响
Table 2. Univariate and multivariate logistic regression analysis of the effects of different risk factors on the incidence of GDM
变量 OR(95% CI)值 P值 变量 OR(95% CI)值 P值 单因素logistic回归 单因素logistic回归 年龄(岁) 1.53(1.44~1.62) < 0.001 巨大儿分娩史 0.82(0.39~1.72) 0.059 BMI (kg/m2) 1.74(1.62~1.88) < 0.001 辅助生殖 0.83(0.74~0.93) 0.001 孕次 0.99(0.93~1.05) 0.708 多因素logistic回归 产次 0.97(0.91~1.03) 0.246 年龄(岁) 1.47(1.41~1.54) < 0.001 吸烟史 1.13(0.96~1.34) 0.150 BMI (kg/m2) 1.74(1.65~1.83) < 0.001 饮酒史 0.95(0.87~1.03) 0.193 是否服用叶酸 0.81(0.68~0.97) 0.019 是否服用叶酸 0.81(0.70~0.94) 0.005 内分泌疾病史 9.32(8.68~10.01) < 0.001 内分泌疾病史 8.71(8.15~9.31) < 0.001 多胎妊娠 1.19(1.00~1.43) 0.056 多胎妊娠 0.84(0.73~0.98) 0.022 辅助生殖 1.06(0.92~1.21) 0.460 -
[1] Juan J, Yang H. Prevalence, prevention, and lifestyle intervention of gestational diabetes mellitus in China[J]. Int J Environ Res Public Health, 2020, 17(24): 9517. DOI: 10.3390/ijerph17249517. [2] Damm P, Houshmand-Oeregaard A, Kelstrup L, et al. Gestational diabetes mellitus and long-term consequences for mother and offspring: a view from Denmark[J]. Diabetologia, 2016, 59(7): 1396-1399. DOI: 10.1007/s00125-016-3985-5. [3] Bianco ME, Josefson JL. Hyperglycemia during pregnancy and long-term offspring outcomes[J]. Curr Diab Rep, 2019, 19(12): 143. DOI: 10.1007/s11892-019-1267-6. [4] Buchanan TA, Xiang AH, Page KA. Gestational diabetes mellitus: risks and management during and after pregnancy[J]. Nat Rev Endocrinol, 2012, 8(11): 639-649. DOI: 10.1038/nrendo.2012.96. [5] Gao C, Sun X, Lu L, et al. Prevalence of gestational diabetes mellitus in mainland China: a systematic review and meta-analysis[J]. J Diabetes Investig, 2019, 10(1): 154-162. DOI: 10.1111/jdi.12854. [6] Wang M, Hu RY, Gong WW, et al. Trends in prevalence of gestational diabetes mellitus in Zhejiang Province, China, 2016-2018[J]. Nutr Metab (Lond), 2021, 18(1): 12. DOI: 10.1186/s12986-020-00539-8. [7] Yan B, Yu Y, Lin M, et al. High, but stable, trend in the prevalence of gestational diabetes mellitus: a population-based study in Xiamen, China[J]. J Diabetes Investig, 2019, 10(5): 1358-1364. DOI: 10.1111/jdi.13039. [8] 赵豆豆, 单莉, 米阳, 等. 基于出生人口队列的妊娠期糖尿病及孕中期血糖水平对孕周的影响[J]. 西安交通大学学报(医学版), 2021, 42(4): 623-627. DOI: 10.7652/jdyxb202104023.Zhao DD, Shan L, Mi Y, et al. Effects of gestational diabetes mellitus and second-trimester blood glucose level on gestational age based on birth cohort[J]. Journal of Xi'an Jiaotong University (Medical Sci), 2021, 42(4): 623-627. DOI: 10.7652/jdyxb202104023. [9] 张楠, 陈宇, 刘东方, 等. 2005年至2009年重庆市区妊娠糖尿病发病率趋势回顾性调查及相关因素比较[J]. 中华内分泌代谢杂志, 2011, 27(5): 404-407. DOI: 10.3760/cma.j.issn.1000-6699.2011.05.011.Zhang N, Chen Y, Liu DF, et al. A retrospective survey on the incidence of gestational diabetes mellitus in Chongqing urban area from 2005 to 2009 and comparison of related factors[J]. Chin J Endocrinol Metab, 2011, 27(5): 404-407. DOI: 10.3760/cma.j.issn.1000-6699.2011.05.011. [10] Su FL, Lu MC, Yu SC, et al. Increasing trend in the prevalence of gestational diabetes mellitus in Taiwan[J]. J Diabetes Investig, 2021, 12(11): 2080-2088. DOI: 10.1111/jdi.13595. [11] Wu L, Han L, Zhan Y, et al. Prevalence of gestational diabetes mellitus and associated risk factors in pregnant Chinese women: a cross-sectional study in Huangdao, Qingdao, China[J]. Asia Pac J Clin Nutr, 2018, 27(2): 383-388. DOI: 10.6133/apjcn.032017.03. [12] Leng J, Shao P, Zhang C, et al. Prevalence of gestational diabetes mellitus and its risk factors in Chinese pregnant women: a prospective population-based study in Tianjin, China[J]. PLoS One, 2015, 10(3): e0121029. DOI: 10.1371/journal.pone.0121029. [13] Yong HY, Mohd Shariff Z, Mohd Yusof BN, et al. Independent and combined effects of age, body mass index and gestational weight gain on the risk of gestational diabetes mellitus[J]. Sci Rep, 2020, 10(1): 8486. DOI: 10.1038/s41598-020-65251-2. [14] Lee CS, Zhu S, Wu Q, et al. Independent and joint associations of age, pre-pregnancy BMI, and gestational weight gain with adverse pregnancy outcomes in gestational diabetes mellitus[J]. Diabetes Ther, 2022: epub aheat of print. DOI: 10.1007/s13300-022-01352-7. [15] Li Y, Ren X, He L, et al. Maternal age and the risk of gestational diabetes mellitus: a systematic review and meta-analysis of over 120 million participants[J]. Diabetes Res Clin Pract, 2020, 162: 108044. DOI: 10.1016/j.diabres.2020.108044. [16] Xu X, Liu Y, Liu D, et al. Prevalence and determinants of gestational diabetes mellitus: a cross-sectional study in China[J]. Int J Environ Res Public Health, 2017, 14(12): 1532. DOI: 10.3390/ijerph14121532. [17] Yang H, Wei Y, Gao X, et al. Risk factors for gestational diabetes mellitus in Chinese women: a prospective study of 16, 286 pregnant women in China[J]. Diabet Med, 2009, 26(11): 1099-1104. DOI: 10.1111/j.1464-5491.2009.02845.x. [18] Read SH, Rosella LC, Berger H, et al. BMI and risk of gestational diabetes among women of South Asian and Chinese ethnicity: a population-based study[J]. Diabetologia, 2021, 64(4): 805-813. DOI: 10.1007/s00125-020-05356-5. [19] 林晶, 陈蕾, 沈梦尘, 等. 妊娠期糖尿病孕前体质量指数对糖代谢及妊娠结局的影响[J]. 实用妇产科杂志, 2021, 37(6): 466-470.Lin J, Chen Li, Shen MC, et al. The effect of pre-pregnancy body mass index on glucose metabolism and pregnancy outcome in gestational diabetes mellitus[J]. J Prac Obste Gynecol, 2021, 37(6): 466-470. [20] 李雪姣, 陈淑琴. 妊娠期糖尿病OGTT结果与孕前体重指数的相关研究及危险因素分析[J]. 现代妇产科进展, 2020, 29(9): 694-696. DOI: 10.13283/j.cnki.xdfckjz.2020.09.009.Li XJ, Chen SQ. Correlation study and risk factor analysis between OGTT results and pre-pregnancy body mass index in gestational diabetes mellitus[J]. Prog Obstet Gynecol, 2020, 29(9): 694-696. DOI: 10.13283/j.cnki.xdfckjz.2020.09.009. [21] Luo J, Wang X, Yuan L, et al. Association of thyroid disorders with gestational diabetes mellitus: a meta-analysis[J]. Endocrine, 2021, 73(3): 550-560. DOI: 10.1007/s12020-021-02712-2. [22] Yang S, Shi FT, Leung PC, et al. Low thyroid hormone in early pregnancy is associated with an increased risk of gestational diabetes mellitus[J]. J Clin Endocrinol Metab, 2016, 101(11): 4237-4243. DOI: 10.1210/jc.2016-1506 -





 下载:
下载: