Transmission modes and influencing factors of Streptococcus pneumoniae among preschool children in Foshan
-
摘要:
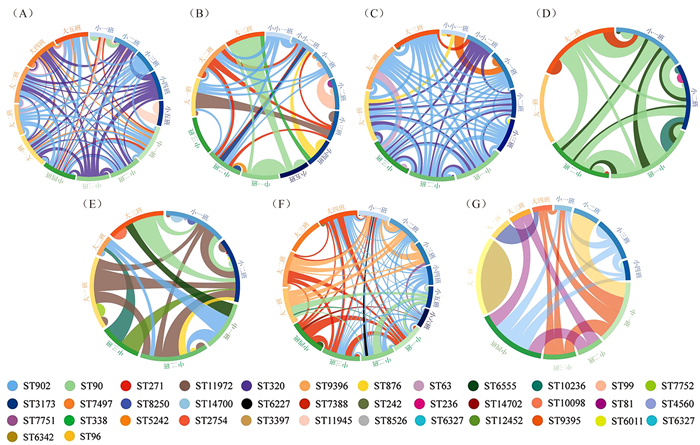
目的 掌握学龄前儿童肺炎链球菌的传播模式及其影响因素,为揭示传播模式和控制传播提供重要的科学依据。 方法 采用分层整群抽样法,抽取佛山市顺德区7所幼儿园2 031名健康儿童,进行鼻拭子采样并分离鉴定肺炎链球菌。儿童肺炎链球菌携带的聚集性分析采用随机效应模型,运用分子型别的同源性分析揭示传播模式,肺炎链球菌携带的影响因素采用χ2检验与随机效应logistic回归分析模型相结合方法。 结果 儿童鼻腔肺炎链球菌携带率为21.8%。随机效应模型分析提示,儿童肺炎链球菌携带存在班级聚集性(Z=4.34, P < 0.001);7所幼儿园菌株班级内同源率分别为60.9%、79.2%、76.0%、80.0%、82.8%、75.9%和33.3%;班级间同源率分别为90.6%、91.7%、88.0%、82.9%、63.8%、93.1%和76.2%。影响因素分析表明,非佛山市户籍(OR=1.36, 95% CI: 1.04~1.79, P=0.027)、农村地区(OR=1.60, 95% CI: 1.09~2.35, P=0.017)、鼻腔携带卡他莫拉杆菌(OR=1.91, 95% CI: 1.49~2.45, P < 0.001)是肺炎链球菌携带的危险因素;年级升高(OR=0.66, 95% CI: 0.52~0.83, P < 0.001)、鼻腔携带金黄色葡萄球菌(OR=0.41, 95% CI: 0.31~0.55, P < 0.001)是肺炎链球菌携带的保护因素。 结论 儿童肺炎链球菌存在较高的班级内和班级间传播风险,年级、户籍、地区以及鼻腔其他细菌携带情况是学龄前儿童肺炎链球菌携带的重要影响因素。 Abstract:Objective To urderstand the transmission mode and influencing factors of Streptococcus pneumoniae (S. pneumoniae) in preschool children, and to provide an important scientific basis for revealing the transmission pattern and controlling the transmission. Methods Stratified cluster sampling method was used to select 2 031 healthy children from seven kindergartens in Shunde District, Foshan City. Nasal swabs were taken and tested for S. pneumoniae. The random-effect model was used to explore the clustering of S. pneumoniae carriage in children, and homology analysis of molecular types was used to reveal the transmission mode. Both χ2 test and random-effect logistic regression were used to analyze the effects of multiple influencing factors. Results The nasal carriage rate of S. pneumoniae in children was 21.8%. Random-effect model indicated that there was a class-level clustering effect of S. pneumoniae carriage in children (Z=4.34, P < 0.001). The within-class homology rates of strains in seven kindergartens were 60.9%, 79.2%, 76.0%, 80.0%, 82.8%, 75.9% and 33.3%, respectively. The between-class homology rates were 90.6%, 91.7%, 88.0%, 82.9%, 63.8%, 93.1% and 76.2%, respectively. The analysis of influencing factors showed that non-household registration (OR=1.36, 95% CI: 1.04-1.79, P=0.027), rural area (OR=1.60, 95% CI: 1.09-2.35, P=0.017) and nasal carrying Moraxella catarrhalis (OR=1.91, 95% CI: 1.49-2.45, P < 0.001) were risk factors for S. pneumoniae carriage, while grade (OR=0.66, 95% CI: 0.52-0.83, P < 0.001) and nasal Staphylococcus aureus carriage (OR=0.41, 95% CI: 0.31-0.55, P < 0.001) were protective factors. Conclusions There is a high risk of S. pneumoniae transmission among children within and between classes. Grade, household registration, area and nasal carriage of other bacteria are important influencing factors for S. pneumoniae carriage in preschool children. -
Key words:
- Streptococcus pneumoniae /
- Clustering /
- Influencing factors /
- Children
-
表 1 儿童肺炎链球菌携带的聚集性分析
Table 1. Clustering analysis of Streptococcus pneumoniae carriage in children
分层变量 固定效应 随机效应 β0值 sx值 Z值 P值 σu02值 sx值 Z值 P值 ICC值(%) 总体 -1.40 0.12 -12.05 < 0.001 0.74 0.17 4.34 < 0.001 18.4 性别 男 -1.41 0.13 -10.70 < 0.001 0.76 0.23 3.37 < 0.001 18.8 女 -1.48 0.15 -9.90 < 0.001 0.92 0.28 3.24 0.001 21.9 年级 小班 -0.93 0.20 -4.64 < 0.001 0.92 0.33 2.84 0.004 21.9 中班 -1.58 0.19 -8.34 < 0.001 0.51 0.24 2.15 0.031 13.5 大班 -1.79 0.11 -16.39 < 0.001 < 0.01 < 0.01 < 0.01 1.000 < 0.1 户籍 佛山市 -1.61 0.15 -10.75 < 0.001 0.98 0.28 3.50 < 0.001 23.0 其他 -1.18 0.12 -9.60 < 0.001 0.53 0.19 2.81 0.005 13.9 地区 城镇 -1.67 0.14 -11.68 < 0.001 0.45 0.17 2.56 0.010 12.0 农村 -1.13 0.17 -6.67 < 0.001 0.84 0.26 3.23 0.001 20.3 表 2 儿童肺炎链球菌携带的单因素分析结果[n(%)]
Table 2. Results of univariate analysis of Streptococcus pneumoniae carriage in children [n(%)]
影响因素 携带人数 χ2值 P值 影响因素 携带人数 χ2值 P值 年级 62.13 a < 0.001 近两周抗生素使用史 2.04 0.361 小班(n=690) 220(31.9) 无(n=1 521) 321(21.1) 中班(n=657) 125(19.0) 有(n=319) 74(23.2) 大班(n=684) 98(14.3) 不详(n=191) 48(25.1) 性别 0.02 0.875 近三月呼吸道感染史 4.77 0.029 男(n=1 112) 244(21.9) 无(n=783) 151(19.3) 女(n=919) 199(21.7) 有(n=1 248) 292(23.4) 户籍 7.06 0.008 肺炎球菌疫苗接种史 3.02 0.221 佛山市(n=1 144) 225(19.7) 无(n=801) 162(20.2) 其他(n=887) 218(24.6) 有(n=637) 153(24.0) 地区 26.53 < 0.001 不详(n=593) 128(21.6) 城镇(n=1 054) 182(17.3) 总居住面积(m2) 9.80 a 0.002 农村(n=977) 261(26.7) ≤50(n=282) 81(28.7) 同住儿童 3.22 0.073 >50~100(n=940) 206(21.9) 无(n=140) 39(27.9) >100(n=809) 156(19.3) 有(n=1 891) 404(21.4) 单独睡觉频率 7.26a 0.007 鼻腔携带金葡菌 64.04 < 0.001 从未(n=1 775) 402(22.7) 否(n=1 346) 364(27.0) 偶尔(n=136) 26(19.1) 是(n=685) 79(11.5) 经常(n=120) 15(12.5) 鼻腔携带卡他菌 56.24 < 0.001 参加托管班 3.67 0.055 否(n=966) 141(14.6) 无(n=1 720) 388(22.6) 是(n=1 065) 302(28.4) 有(n=311) 55(17.7) 注:a表示采用趋势χ2检验。 表 3 儿童肺炎链球菌携带影响因素的随机效应logistic回归分析模型分析
Table 3. Random-effect logistic model for influencing factors of Streptococcus pneumoniae carriage in children
影响因素 β值 sx值 Z值 OR(95% CI)值 P值 固定部分 截距 -1.87 0.76 -2.46 0.15(0.03~0.69) 0.014 年级(小班=1,中班=2,大班=3) -0.42 0.12 -3.55 0.66(0.52~0.83) < 0.001 户籍(其他=1,佛山市=0) 0.31 0.14 2.21 1.36(1.04~1.79) 0.027 地区(农村=1,城镇=0) 0.47 0.20 2.39 1.60(1.09~2.35) 0.017 鼻腔携带卡他菌(是=1,否=0) 0.65 0.13 5.08 1.91(1.49~2.45) < 0.001 鼻腔携带金葡菌(是=1,否=0) -0.89 0.15 -6.07 0.41(0.31~0.55) < 0.001 总居住面积(≤50 m2=1,>50~100 m2=2,>100 m2=3) -0.10 0.10 -0.95 0.91(0.75~1.11) 0.340 单独睡觉频率(经常=1,偶尔=2,从未=3) 0.16 0.13 1.22 1.17(0.91~1.52) 0.224 同住儿童(是=1,否=0) -0.22 0.22 -1.01 0.80(0.52~1.23) 0.315 近三个月呼吸道感染史(是=1,否=0) -0.11 0.13 -0.85 0.90(0.70~1.15) 0.395 参加托管班(有=1,无=0) 0.06 0.18 0.32 1.06(0.75~1.50) 0.751 随机部分 水平2方差 0.41 0.12 3.48 < 0.001 水平1尺度参数 1.00 -
[1] Mohamed YH, Toizumi M, Uematsu M, et al. Prevalence of Streptococcus pneumoniae in conjunctival flora and association with nasopharyngeal carriage among children in a Vietnamese community[J]. Sci Rep, 2021, 11(1): 337. DOI: 10.1038/s41598-020-79175-4. [2] Koliou MG, Andreou K, Lamnisos D, et al. Risk factors for carriage of Streptococcus pneumoniae in children[J]. BMC Pediatr, 2018, 18(1): 144. DOI: 10.1186/s12887-018-1119-6. [3] 张慧芬, 李基明, 吴佳音, 等. 儿童侵袭性肺炎链球菌病35例临床特征和分离株耐药性分析[J]. 中国感染与化疗杂志, 2021, 21(2): 152-157. DOI: 10.16718/j.1009-7708.2021.02.005.Zhang HF, Li JM, Wu JY, et al. Clinical characteristics and antibiotic resistance profile of invasive Streptococcus pneumoniae disease in 35 children[J]. Chin J Infect Chemother, 2021, 21(2): 152-157. DOI: 10.16718/j.1009-7708.2021.02.005. [4] Narwortey DK, Owusu-Ofori A, Slotved HC, et al. Nasopharyngeal carriage of Streptococcus pneumoniae among healthy children in Kassena-Nankana Districts of Northern Ghana[J]. BMC Infect Dis, 2021, 21(1): 661. DOI: 10.1186/s12879-021-06302-5. [5] Hu JY, Sun XD, Huang ZY, et al. Streptococcus pneumoniae and Haemophilus influenzae type b carriage in Chinese children aged 12-18 months in Shanghai, China: a cross-sectional study[J]. BMC Infect Dis, 2016, 16: 149. DOI: 10.1186/s12879-016-1485-3. [6] Xie N, Chen ZY, Chen T, et al. A cross-sectional survey assessing carriage of Streptococcus pneumoniae in a healthy population in Xinjiang Uygur Autonomous Region of China[J]. Biomed Environ Sci, 2018, 31(3): 233-237. DOI: 10.3967/bes2018.029. [7] Dunne EM, Murad C, Sudigdoadi S, et al. Carriage of Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Staphylococcus aureus in Indonesian children: a cross-sectional study[J]. PLoS One, 2018, 13(4): e0195098. DOI: 10.1371/journal.pone.0195098. [8] Wada FW, Tufa EG, Berheto TM, et al. Nasopharyngeal carriage of Streptococcus pneumoniae and antimicrobial susceptibility pattern among school children in South Ethiopia: post-vaccination era[J]. BMC Res Notes, 2019, 12(1): 306. DOI: 10.1186/s13104-019-4330-0. [9] Malfroot A, Verhaegen J, Dubru JM, et al. A cross-sectional survey of the prevalence of Streptococcus pneumoniae nasopharyngeal carriage in Belgian infants attending day care centres[J]. Clin Microbiol Infect, 2004, 10(9): 797-803. DOI: 10.1111/j.1198-743X.2004.00926.x. [10] 吴本权, 唐英春, 朱家馨, 等. 广州市区两幼儿园2~6岁健康儿童肺炎链球菌携带状况调查[J]. 中国当代儿科杂志, 2001, 3(5): 529-531. DOI: 10.3969/j.issn.1008-8830.2001.05.013.Wu BQ, Tang YC, Zhu JX, et al. Carrier rate of Streptococcus pneumoniae in healthy children aged 2-6 in two kindergartens in Guangzhou City[J]. Chin J Contemp Pediatr, 2001, 3(5): 529-531. DOI: 10.3969/j.issn.1008-8830.2001.05.013. [11] 陈惠玲, 熊剑辉, 廖志云, 等. 广东部分地区儿童肺炎链球菌携带株耐药性调查[J]. 广州医学院学报, 2001, 29(4): 10-13. DOI: 10.3969/j.issn.1008-1836.2001.04.004.Chen HL, Xiong JH, Liao ZY, et al. Investigation on drug resistance of Streptococcus pneumoniae strains in children in some areas of Guangdong Province[J]. Academic Journal of Guangzhou Medical College, 2001, 29(4): 10-13. DOI: 10.3969/j.issn.1008-1836.2001.04.004. [12] Gounder PP, Bruce MG, Bruden DJT, et al. Effect of the 13-valent pneumococcal conjugate vaccine on nasopharyngeal colonization by Streptococcus pneumoniae--Alaska, 2008-2012[J]. J Infect Dis, 2014, 209(8): 1251-1258. DOI: 10.1093/infdis/jit642. [13] Kovács E, Sahin-tóth J, Tóthpál A, et al. Co-carriage of Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis among three different age categories of children in Hungary[J]. PLoS One, 2020, 15(2): e0229021. DOI: 10.1371/journal.pone.0229021. [14] Spijkerman J, Prevaes SM, Gils EJM, et al. Long-term effects of pneumococcal conjugate vaccine on nasopharyngeal carriage of S. pneumoniae, S. aureus, H. influenzae and M. catarrhalis[J]. PLoS One, 2012, 7(6): e39730. DOI: 10.1371/journal.pone.0039730. -





 下载:
下载: