A cross-sectional study of the association between low-carbohydrate diet and fasting hyperglycemia
-
摘要:
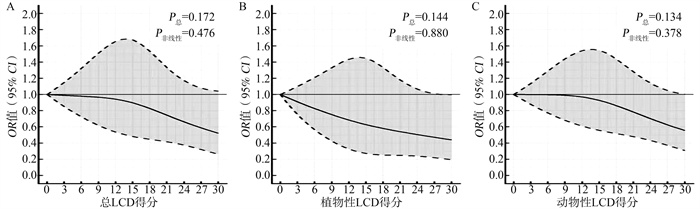
目的 构建低碳水化合物饮食(low-carbohydrate diet, LCD)依从性得分并评估其与高血糖间的关联。 方法 在安徽省六安市进行以人群为基础的横断面调查,根据三大宏量营养素及其亚型的供能比构建膳食总LCD得分、植物性LCD及动物性LCD膳食得分。FPG≥6.1 mmol/L定义为高血糖。采用多重logistic回归分析模型计算OR值及其95%CI。 结果 本次研究最终纳入2 574例研究对象,高血糖者232例,占9.01%。与总LCD依从性得分最低三分位数研究对象相比,最高三分位数研究对象患高血糖的风险更低(OR=0.69,95% CI:0.49~0.99)。植物性LCD(OR=0.61,95% CI: 0.43~0.87)和动物性LCD(OR=0.68,95% CI:0.47~0.98)依从性得分与高血糖的罹患风险呈负相关。替代分析提示:利用饱和脂肪酸(saturated fatty acid, SFA)替代等能量(占总热能的5%)的碳水化合物与降低高血糖风险相关(OR=0.50,95% CI:0.28~0.90),但单不饱和脂肪酸(monounsaturated fatty acid, MUFA)替代碳水化合物与增加高血糖风险相关(OR=1.69,95% CI:1.06~2.68)。 结论 总LCD、植物性LCD、动物性LCD饮食与更低的患高血糖的风险相关。在膳食结构中适当减少碳水化合物,同时增加饱和脂肪的摄入与较低的高血糖患病风险有关。 Abstract:Objective We developed a low-carbohydrate diet (LCD) score and estimated its association with fasting hyperglycemia. Methods Data from a population-based cross-sectional study in Lu'an City, Anhui Province was used to calculate overall LCD, plant LCD, and animal LCD score, based on the percentage of energy from total carbohydrate, total and subtypes of fat, and total and subtypes of protein. Hyperglycemia was defined as fasting glucose ≥ 6.1 mmol/L. Multivariate logistic regression was used to estimate ORs and 95% CIs. Results Of the 2 574 participants included in this study, 232 (9.01%) had hyperglycemia. When comparing the highest with the lowest tertile, the multivariable-adjusted ORs of hyperglycemia were 0.69(0.49-0.99) for overall LCD score, 0.61(0.43-0.87) for plant LCD score, and 0.68(0.47-0.98) for animal LCD score. The isocaloric substitution of 5% energy from saturated fat for carbohydrate was associated with lower odds of hyperglycemia (OR=0.50, 95% CI: 0.28-0.90), while increasing monounsaturated fat in place of carbohydrate was associated with increased odds of hyperglycemia (OR=1.69, 95% CI: 1.06-2.68). Conclusions Greater adherence to overall LCD, plant LCD, and animal LCD score was associated with lower odds of hyperglycemia. An appropriate reduction in carbohydrate intake, and increase in saturated fat intake might yield a lower risk of hyperglycemia. -
Key words:
- Low-carbohydrate diet /
- Hyperglycemia /
- Cross-sectional study
-
表 1 血糖正常与高血糖研究对象的基本特征[n(%)]
Table 1. Characteristics of study participants according to status of glucose [n(%)]
变量 合计(N=2 574) 血糖情况 t/$\chi$2/W值 P值 血糖正常(n=2 342) 高血糖(n=232) FPG(mmol/L) 5.22±1.14 4.96±0.48 7.72±2.25 18.63 < 0.001 性别 < 0.001 女 1 525(59.25) 1 419(60.59) 106(45.69) 18.80 男 1 049(40.75) 923(39.41) 126(54.31) 年龄组(岁) 206 468 < 0.001 a 18~ < 40 748(29.06) 724(30.91) 24(10.34) 40~ < 50 481(18.69) 432(18.45) 49(21.12) 50~ < 60 626(24.32) 558(23.83) 68(29.31) ≥60 719(27.93) 628(26.81) 91(39.22) BMI(kg/m2) 211 646 < 0.001 a < 18.5 120(4.66) 112(4.78) 8(3.45) 18.5~ < 24.0 1 169(45.42) 1 101(47.01) 68(29.31) 24.0~ < 28.0 905(35.16) 809(34.54) 96(41.38) ≥28.0 380(14.76) 320(13.66) 60(25.86) 教育程度b 269 703 0.006 小学及以下 1 301(50.60) 1 167(49.87) 134(58.01) 初中 701(27.27) 639(27.31) 62(26.84) 高中及以上 569(22.13) 534(22.82) 53(15.15) 吸烟b 10.21 0.001 从不吸烟 1 882(73.17) 1 734(74.07) 148(64.07) 曾经或现在吸烟 690(26.83) 607(25.93) 83(35.93) 饮酒b 22.39 < 0.001 从不饮酒 1 959(76.20) 1 812(77.47) 147(63.36) 曾经或现在饮酒 612(23.80) 527(22.53) 85(36.64) 体力活动b 283 982 0.177 a Tertile 1 857(33.33) 771(32.95) 86(37.23) Tertile 2 857(33.33) 782(33.42) 75(32.47) Tertile 3 857(33.33) 787(33.63) 70(30.30) 地区 0.00 1.000 农村 1 915(74.40) 1 742(74.38) 173(74.57) 城市 659(25.60) 600(25.62) 59(25.43) 糖尿病家族史b 0.62 0.431 有家族史 184(7.20) 164(7.05) 20(8.70) 无家族史 2 372(92.80) 2 162(92.95) 210(91.30) 总能量 263 092 0.399 a Tertile 1 858(33.33) 789(33.69) 69(29.74) Tertile 2 858(33.33) 774(33.05) 84(36.21) Tertile 3 858(33.33) 779(33.26) 79(34.05) 总LCD得分 290 320 0.067 a Tertile 1 830(32.25) 742(31.68) 88(37.93) Tertile 2 873(33.92) 799(34.12) 74(31.90) Tertile 3 871(33.84) 801(34.20) 70(30.17) 植物LCD得分 286 225 0.153 a Tertile 1 896(34.81) 809(34.54) 87(37.50) Tertile 2 778(30.23) 703(30.02) 75(32.33) Tertile 3 900(34.97) 830(35.44) 70(30.17) 动物LCD得分 297 177 0.012 a Tertile 1 880(34.19) 786(33.56) 94(40.52) Tertile 2 874(33.95) 795(33.95) 79(34.05) Tertile 3 820(31.86) 761(32.49) 59(25.43) 注: a Wilcoxon秩和检验; b研究对象特征数据存在缺失。 表 2 总LCD得分、植物性LCD得分和动物性LCD得分与空腹高血糖的关联性分析
Table 2. The ORs and 95% CIs of hyperglycemia according to overall LCD, plant LCD, and animal LCD score
低碳水饮食 OR值(95 % CI) P趋势 a Tertile 1 Tertile 2 Tertile 3 每增加5分 总LCD 模型1 b 1.00 0.78(0.56~1.08) 0.74(0.53~1.02) 0.92(0.83~1.02) 0.103 模型2 c 1.00 0.77(0.55~1.08) 0.69(0.49~0.99) 0.90(0.81~1.01) 0.076 植物性LCD 模型1 b 1.00 0.99(0.72~1.37) 0.78(0.56~1.09) 0.98(0.86~1.11) 0.740 模型2 c 1.00 0.89(0.63~1.25) 0.61(0.43~0.87) 0.87(0.76~1.00) 0.051 动物性LCD 模型1 b 1.00 0.83(0.61~1.14) 0.65(0.46~0.91) 0.90(0.83~0.98) 0.018 模型2 c 1.00 0.88(0.64~1.23) 0.68(0.47~0.98) 0.92(0.83~1.01) 0.065 注:a低碳水化合物饮食得分除以5之后以连续性变量进行分析;b没有调整协变量;c调整了性别、年龄、BMI、受教育程度、吸烟状况、饮酒状况、体力活动、地区、糖尿病家族史和总能量。 -
[1] Frank LK, Jannasch F, Kr|ger J, et al. A dietary pattern derived by reduced rank regression is associated with type 2 diabetes in an urban Ghanaian population [J]. Nutrients, 2015, 7(7): 5497-5514. DOI: 10.3390/nu7075233. [2] Shan Z, Rehm CD, Rogers G, et al. Trends in dietary carbohydrate, protein, and fat intake and diet quality among US adults, 1999-2016 [J]. JAMA, 2019, 322(12): 1178-1187. DOI: 10.1001/jama.2019.13771. [3] Zhu Z, Yang X, Fang Y, et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: a Series of National Surveys, 1982-2012 [J]. Nutrients, 2020, 12(8): 2168. DOI: 10.3390/nu12082168. [4] Dehghan M, Mente A, Zhang X, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study [J]. Lancet, 2017, 390(10107): 2050-2062. DOI: 10.1016/S0140-6736(17)32252-3. [5] Halton TL, Willett WC, Liu S, et al. Low-carbohydrate-diet score and the risk of coronary heart disease in women [J]. N Engl J Med, 2006, 355(19): 1991-2002. DOI: 10.1056/nejmoa055317. [6] 雷文慧, 何诗琪, 王豪, 等. 中老年男性吸烟状况与心血管疾病发生风险的关联性[J]. 中华疾病控制杂志, 2019, 23(7): 774-779. DOI: 10.16462/j.cnki.zhjbkz.2019.07.007.Lei WH, He SQ, Wang H, et al. Association of smoking status with incident cardiovascular disease in the middle-aged and older male populations [J]. Chin J Dis Control Prev, 2019, 23(7): 774-779. DOI: 10.16462/j.cnki.zhjbkz.2019.07.007. [7] 李亚茹, 王婧, 赵丽云, 等. 中国成年人饮酒习惯及影响因素[J]. 中华流行病学杂志, 2018, 39(7): 898-903. DOI: 10.3760/cma.j.issn.0254-6450.2018.07.007.Li YR, Wang J, Zhao LY, et al. The drinking status and associated factors in adults in China [J]. Chin J Epidemiol, 2018, 39(7): 898-903. DOI: 10.3760/cma.j.issn.0254-6450.2018.07.007. [8] Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities [J]. Med Sci Sports Exerc, 1993, 25(1): 71-80. DOI: 10.1249/00005768-199301000-00011. [9] Bolla AM, Caretto A, Laurenzi A, et al. Low-carb and ketogenic diets in type 1 and type 2 diabetes [J]. Nutrients, 2019, 11(5): 962. DOI: 10.3390/nu11050962. [10] Zhou C, Zhang Z, Liu M, et al. Dietary carbohydrate intake and new-onset diabetes: a nationwide cohort study in China [J]. Metabolism, 2021, 123: 154865. DOI: 10.1016/j.metabol.2021.154865. [11] Alhazmi A, Stojanovski E, McEvoy M, et al. Macronutrient intakes and development of type 2 diabetes: a systematic review and meta-analysis of cohort studies [J]. J Am Coll Nutr, 2012, 31(4): 243-258. DOI: 10.1080/07315724.2012.10720425. [12] Nanri A, Mizoue T, Kurotani K, et al. Low-carbohydrate diet and type 2 diabetes risk in Japanese men and women: the Japan Public Health Center-Based Prospective Study [J]. PLoS One, 2015, 10(2): e0118377. DOI: 10.1371/journal.pone.0118377. [13] Halton TL, Liu S, Manson JE, et al. Low-carbohydrate-diet score and risk of type 2 diabetes in women [J]. Am J Clin Nutr, 2008, 87(2): 339-346. DOI: 10.1093/ajcn/87.2.339. [14] de Koning L, Fung TT, Liao X, et al. Low-carbohydrate diet scores and risk of type 2 diabetes in men [J]. Am J Clin Nutr, 2011, 93(4): 844-850. DOI: 10.3945/ajcn.110.004333. [15] van Dam RM, Willett WC, Rimm EB, et al. Dietary fat and meat intake in relation to risk of type 2 diabetes in men [J]. Diabetes Care, 2002, 25(3): 417-424. DOI: 10.2337/diacare.25.3.417. [16] Risérus U, Willett WC, Hu FB. Dietary fats and prevention of type 2 diabetes [J]. Prog Lipid Res, 2009, 48(1): 44-51. DOI: 10.1016/j.plipres.2008.10.002. [17] Nanri A, Mizoue T, Noda M, et al. Rice intake and type 2 diabetes in Japanese men and women: the Japan public health center-based prospective study [J]. Am J Clin Nutr, 2010, 92(6): 1468-1477. DOI: 10.3945/ajcn.2010.29512. [18] Hu EA, Pan A, Malik V, et al. White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review [J]. BMJ, 2012, 344: e1454. DOI: 10.1136/bmj.e1454. [19] Morris E, Aveyard P, Dyson P, et al. A food-based, low-energy, low-carbohydrate diet for people with type 2 diabetes in primary care: a randomized controlled feasibility trial [J]. Diabetes Obes Metab, 2020, 22(4): 512-520. DOI: 10.1111/dom.13915. [20] Han Y, Cheng B, Guo Y, et al. A low-carbohydrate diet realizes medication withdrawal: a possible opportunity for effective glycemic control [J]. Front Endocrinol (Lausanne), 2021, 12: 779636. DOI: 10.3389/fendo.2021.779636. [21] Satija A, Bhupathiraju SN, Rimm EB, et al. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies [J]. PLoS Med, 2016, 13(6): e1002039. DOI: 10.1371/journal.pmed.1002039. [22] Merino J, Guasch-Ferré M, Ellervik C, et al. Quality of dietary fat and genetic risk of type 2 diabetes: individual participant data meta-analysis [J]. BMJ, 2019, 7: l5612. DOI: 10.1136/bmj.l5612. [23] Neuenschwander M, Barbaresko J, Pischke CR, et al. Intake of dietary fats and fatty acids and the incidence of type 2 diabetes: a systematic review and dose-response meta-analysis of prospective observational studies [J]. PLoS Med, 2020, 17(12): e1003347. DOI: 10.1371/journal.pmed.1003347. [24] Parr EB, Devlin BL, Callahan MJ, et al. Effects of providing high-fat versus high-carbohydrate meals on daily and postprandial physical activity and glucose patterns: a randomised controlled trial [J]. Nutrients, 2018, 10(5): 557. DOI: 10.3390/nu10050557. [25] Tsunoda N, Ikemoto S, Takahashi M, et al. High-monounsaturated fat diet-induced obesity and diabetes in C57BL/6J mice [J]. Metabolism, 1998, 47(6): 724-730. DOI: 10.1016/S0026-0495(98)90037-3. [26] Sarabhai T, Kahl S, Szendroedi J, et al. Monounsaturated fat rapidly induces hepatic gluconeogenesis and whole-body insulin resistance [J]. JCI Insight, 2020, 5(10): e134520. DOI: 10.1172/jci.insight.134520. -





 下载:
下载: