Relationship between sleep quality and cognitive function and the mediating role of depression for older adults in the rural areas of Guizhou Province
-
摘要:
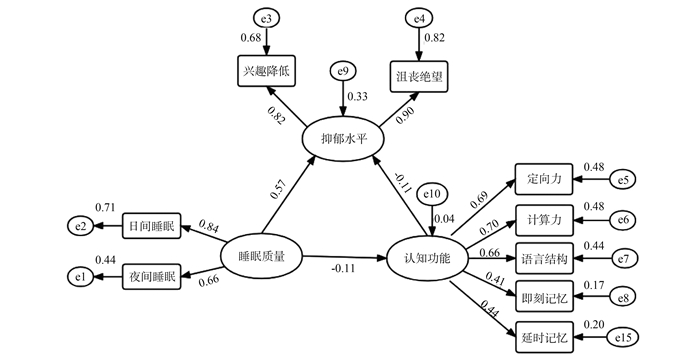
目的 了解贵州省农村老年人睡眠质量对认知功能的影响,并分析抑郁状态在其中的中介作用。 方法 采用一般资料调查表、简易精神状态检测量表(mini-mental state examination, MMSE)、阿森斯失眠量表(Athens insomnia scale, AIS)和患者健康问卷-2(the patient health questionnaire-2, PHQ-2)对1 615名贵州省农村老年人进行调查。构建结构方程模型(structural equation model, SEM)分析抑郁状态在睡眠质量与认知功能间的中介作用。 结果 不同性别、年龄、职业、婚姻状况及文化程度的老年人,其认知功能差异有统计学意义(均P<0.001)。睡眠质量与认知功能存在直接关联(β=-0.061, 95% CI: -0.109~-0.015),并存在由抑郁状态介导的间接关联(β=-0.113, 95% CI: -0.203~-0.024),且抑郁状态的相对中介效应(64.94%)大于睡眠质量对认知功能的直接效应(35.06%)。 结论 贵州省农村老年人睡眠质量与认知功能密切相关,抑郁状态可能是它们之间重要的中介因素。 Abstract:Objective This research seeks to examine how sleep quality influences the cognitive function of elderly individuals in rural areas of Guizhou Province, with a particular focus on the mediating role of depression. Methods We conducted a survey on 1 615 older adults living in rural areas of Guizhou Province using a general data questionnaire, the mini-mental state examination (MMSE), the Athens insomnia scale (AIS), and the patient health questionnaire-2 (PHQ-2). The structural equation model (SEM) was used to analyze the indirect effect of depression on the relationship between sleep quality and cognitive function. Results There were significant differences in cognitive function among older adults with different gender, ages, occupations, marital statuses, and educational levels (all P < 0.001). A direct association was identified between sleep quality and cognitive function (β=-0.061, 95% CI: -0.109-0.015), and depression displayed an indirect association between sleep quality and cognitive function (β=-0.113, 95% CI: -0.203-0.024). In addition, the mediating effect of depression (64.94%) on the correlation between sleep quality and cognitive function was greater than the direct effect of sleep quality on cognitive function (35.06%). Conclusions Sleep quality significantly affects the cognitive function of elderly individuals in rural areas of Guizhou Province. Additionally, depression plays a crucial mediating role in the relationship between sleep quality and cognitive function. -
Key words:
- Sleep quality /
- Depressive state /
- Cognitive function /
- Elderly
-
表 1 贵州省不同特征老年人认知功能情况比较(n=1 615)
Table 1. Comparison of cognitive function of older adults with different characteristics in Guizhou Province (n=1 615)
变量 人数
(占比/%)MMSE评分
(x±s)/分t/F值 P值 变量 人数
(占比/%)MMSE评分
(x±s)/分t/F值 P值 性别 16.56 <0.001 文化程度 174.17 <0.001 男 688(42.60) 23.39±4.58 文盲或半文盲 1 255(77.71) 19.91±5.02 女 927(57.40) 19.37±4.99 小学 222(13.75) 24.91±3.34 年龄组/岁 42.64 <0.001 初中及以上 138(8.54) 25.61±3.88 60~<65 228(14.12) 22.88±4.83 婚姻 8.95 <0.001 65~<70 486(30.09) 22.21±4.78 在婚 998(61.80) 21.98±4.94 70~<75 425(26.32) 21.21±4.99 非在婚 617(38.20) 19.64±5.32 75~<80 291(18.02) 19.93±4.94 职业 -7.63 <0.001 ≥80 185(11.45) 17.44±5.55 务农 1 471(91.08) 20.82±5.21 非务农 144(8.92) 23.80±4.39 注:1. MMSE:简易精神状态检测量表。 表 2 老年人睡眠质量、抑郁状态与认知功能各领域的关联(x±s)
Table 2. Association between sleep quality, depression status and various domains of cognitive function in the elderly (x±s)
项目/分 MMSE评分 定向力 注意力和计算力 语言结构模仿能力 即刻记忆力 延时记忆力 PHQ-2 非抑郁 21.66±5.07 7.46±2.18 2.40±1.95 7.74±1.00 2.70±0.77 1.35±1.27 抑郁状态 20.20±5.31 7.03±2.27 1.94±1.88 7.50±1.10 2.54±0.92 1.18±1.26 t值 5.55 3.82 4.82 4.29 3.64 2.63 P值 <0.001 <0.001 <0.001 <0.001 <0.001 0.009 AIS 睡眠正常 21.50±5.03 7.40±2.15 2.37±1.94 7.73±0.97 2.70±0.75 1.31±1.27 失眠 20.12±5.50 7.05±2.38 1.88±1.89 7.46±1.19 2.51±0.97 1.22±1.28 t值 4.91 2.80 4.71 4.37 3.71 1.27 P值 <0.001 0.005 <0.001 <0.001 <0.001 0.205 注:1. MMSE:简易精神状态检测量表。2. PHQ-2:患者健康问卷-2。3. AIS:阿森斯失眠量表。 表 3 贵州省农村老年人睡眠质量、抑郁状态与认知功能的多重线性回归
Table 3. Multiple linear regression of sleep quality, depression status and cognitive function in rural elderly in Guizhou
项目/分 MMSE评分 定向力 注意力和计算力 语言结构模仿能力 即刻记忆力 延时记忆力 β1 β2 β1 β2 β1 β2 β1 β2 β1 β2 β1 β2 AIS -0.160 ① -0.064 ② -0.039 ③ -0.001 -0.055 ① -0.023 ② -0.032 ① -0.019 ③ -0.020 ① -0.016 ③ -0.014 -0.006 PHQ-2 -0.429 ① -0.182 ③ -0.157 ① -0.060 ② -0.155 ① -0.066 ③ -0.050 ③ -0.016 -0.021 -0.012 -0.046 ② -0.028 注:1. β1:未调整人口学变量因素。2. β2:在模型1的基础上调整年龄、性别、文化程度、婚姻、职业。3. MMSE:简易精神状态检测量表。4. PHQ-2:患者健康问卷-2。5. AIS:阿森斯失眠量表。
①代表P<0.001。②代表P<0.05。③代表P<0.01。表 4 中介效应的Bootstrap检验(标准化系数)
Table 4. Bootstrap test for mediation effect (standardized coefficients)
效应 路径 效应值 中介效应占比/% 95% CI ① 偏差校正95% CI ② 直接 睡眠-认知 -0.061 35.06 -0.109~-0.015 -0.109~-0.015 中介 睡眠-抑郁-认知 -0.113 64.94 -0.203~-0.024 -0.202~-0.023 总效应 -0.174 注:①用百分位数法计算的95% CI。②经Bootstrap参数估计进行偏差校正后的95% CI。 -
[1] 王振杰, 于海军, 唐婧, 等. 中国老年人认知障碍率的Meta分析[J]. 中国循证医学杂志, 2020, 20(11): 1295-1300. DOI: 10.7507/1672-2531.202006099.Wang ZJ, Yu HJ, Tang J, et al. Cognitive impairment rate of the elderly in China: a meta-analysis[J]. Chin J Evid Based Med, 2020, 20(11): 1295-1300. DOI: 10.7507/1672-2531.20200609. [2] Smith L, Shin JI, Jacob L, et al. Sleep problems and mild cognitive impairment among adults aged≥ 50 years from low-and middle-income countries[J]. Exp Gerontol, 2021, 154: 111513. DOI: 10.1016/j.exger.2021.111513. [3] Stojek MMK, Montoya AK, Drescher CF, et al. Fitness, sleep-disordered breathing, symptoms of depression, and cognition in inactive overweight children: mediation models[J]. Public Health Rep, 2017, 132(2_suppl): 65S-73S. DOI: 10.1177/0033354917731308. [4] 熊风, 赖玉清, 涂嘉欣, 等. 中国老年人群睡眠障碍流行特征的Meta分析[J]. 中国循证医学杂志, 2019, 19(4): 398-403. DOI: 10.7507/1672-2531.201808151.Xiong F, Lai YQ, Tu JX, et al. Epidemiological characteristics of sleep disorders in the Chinese elderly: a meta-analysis[J]. Chin J Evid Based Med, 2019, 19(4): 398-403. DOI: 10.7507/1672-2531.201808151. [5] 杨婷, 汪敬轩, 谢志豪, 等. 中国老年居民抑郁症状现状及其影响因素分析[J]. 现代预防医学, 2021, 48(19): 3461-3465, 3599.Yang T, Wang JX, Xie ZH, et al. Current status of depressive symptoms and their influencing factors among elderly Chinese residents[J]. Mod Prev Med, 2021, 48(19): 3461-3465, 3599. [6] 郑培, 薛蓉. 睡眠对类淋巴系统清除β淀粉样蛋白的影响[J]. 中华老年心脑血管病杂志, 2019, 21(1): 100-102. DOI: 10.3969/j.issn.1009-0126.2019.01.026.Zheng P, Xue R. Effect of sleep on the clearance of β-amyloid by lymphoid system[J]. Chin J Geriatr Heart Brain Vessel Dis, 2019, 21(1): 100-102. DOI: 10.3969/j.issn.1009-0126.2019.01.026. [7] Mac Giollabhui N. Inflammation and depression: research designs to better understand the mechanistic relationships between depression, inflammation, cognitive dysfunction, and their shared risk factors[J]. Brain Behav Immun Health, 2021, 15: 100278. DOI: 10.1016/j.bbih.2021.100278. [8] Goldstone A, Javitz HS, Claudatos SA, et al. Sleep disturbance predicts depression symptoms in early adolescence: initial findings from the adolescent brain cognitive development study[J]. J Adolesc Health, 2020, 66(5): 567-574. DOI: 10.1016/j.jadohealth.2019.12.005. [9] 周小炫, 谢敏, 陶静, 等. 简易智能精神状态检查量表的研究和应用[J]. 中国康复医学杂志, 2016, 31(6): 694-696, 706. DOI: 10.3969/j.issn.1001-1242.2016.06.019.Zhou XX, Xie M, Tao J, et al. Study and application of mini-mental state examination[J]. Chin J Rehabil Med, 2016, 31(6): 694-696, 706. DOI: 10.3969/j.issn.1001-1242.2016.06.019. [10] Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens insomnia scale: validation of an instrument based on ICD-10 criteria[J]. J Psychosom Res, 2000, 48(6): 555-560. DOI: 10.1016/s0022-3999(00)00095-7. [11] Silverberg JI, Lee B, Lei D, et al. Measurement properties of patient health questionnaire 9 and patient health questionnaire 2 in adult patients with atopic dermatitis[J]. Dermatitis, 2021, 32(4): 225-231. DOI: 10.1097/DER.0000000000000653. [12] 张骏, 宋瑞远, 苏明宏, 等. 安徽省合肥市农村人群睡眠质量与认知功能的相关性分析[J]. 中华疾病控制杂志, 2015, 19(8): 819-823. DOI: 10.16462/j.cnki.zhjbkz.2015.08.016.Zhang J, Song RY, Su MH, et al. Correlation analysis of sleep quality and cognitive function among the Hefei rural population in Anhui Province[J]. Chin J Dis Control Prev, 2015, 19(8): 819-823. DOI: 10.16462/j.cnki.zhjbkz.2015.08.016. [13] Xu Y, Wen H, Li J, et al. The relationship between sleep disorders, anxiety, depression, and cognitive function with restless legs syndrome (RLS) in the elderly[J]. Sleep Breath, 2022, 26(3): 1309-1318. DOI: 10.1007/s11325-021-02477-y. [14] Schmidt MH, Dekkers MPJ, Baillieul S, et al. Measuring sleep, wakefulness, and circadian functions in neurologic disorders[J]. Sleep Med Clin, 2021, 16(4): 661-671. DOI: 10.1016/j.jsmc.2021.08.005. [15] Rahmani M, Rahmani F, Rezaei N. The brain-derived neurotrophic factor: missing link between sleep deprivation, insomnia, and depression[J]. Neurochem Res, 2020, 45(2): 221-231. DOI: 10.1007/s11064-019-02914-1. [16] Zhao S, Wang X, Chen Z, et al. Sex differences in the association between symptom profiles and cognitive functioning in patients with depressive disorder[J]. J Affect Disord, 2021, 287: 1-7. DOI: 10.1016/j.jad.2021.03.020. [17] Fonseca E, Campos Blanco DM, Castro Vilanova MD, et al. Relationship between sleep quality and cognitive performance in patients with epilepsy[J]. Epilepsy Behav, 2021, 122: 108127. DOI: 10.1016/j.yebeh.2021.108127. [18] Song D, Zhou J, Ma J, et al. Sleep disturbance mediates the relationship between depressive symptoms and cognitive function in older adults with mild cognitive impairment[J]. Geriatr Nurs, 2021, 42(5): 1019-1023. DOI: 10.1016/j.gerinurse.2021.06.004. [19] Xu WQ, Lin LH, Ding KR, et al. The role of depression and anxiety in the relationship between poor sleep quality and subjective cognitive decline in Chinese elderly: exploring parallel, serial, and moderated mediation[J]. J Affect Disord, 2021, 294: 464-471. DOI: 10.1016/j.jad.2021.07.063. [20] Guan Q, Hu X, Ma N, et al. Sleep quality, depression, and cognitive function in non-demented older adults[J]. J Alzheimer's Dis, 2020, 76(4): 1637-1650. DOI: 10.3233/JAD-190990. [21] Akers KG, Chérasse Y, Fujita Y, et al. Concise review: regulatory influence of sleep and epigenetics on adult hippocampal neurogenesis and cognitive and emotional function[J]. Stem cells, 2018, 36(7): 969-976. DOI: 10.1002/stem.2815. -





 下载:
下载: