Evaluating self-management types in hypertensive patients and their effect on blood pressure using latent profile analysis
-
摘要:
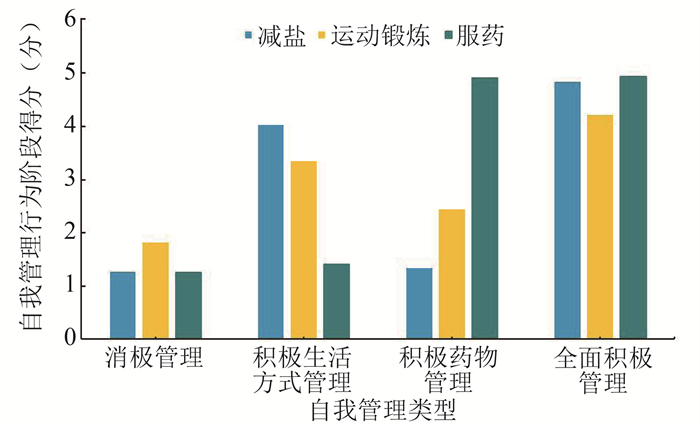
目的 探究高血压患者的自我管理类型、血压控制现状及二者之间的关系。 方法 选取北京市大兴区的高血压患者作为研究对象, 对其进行问卷调查和身体检查。采用潜剖面分析探究高血压患者的自我管理类型, 采用一般线性回归探究其与血压水平的关系, 采用χ2检验探究自我管理类型的特征。 结果 共纳入高血压患者1 260名, 其自我管理类型可以分为消极管理(21.98%)、积极生活方式管理(9.68%)、积极药物管理(32.22%)、全面积极管理(36.12%)4类。相比于消极管理型, 全面积极管理的患者SBP水平降低(β=-4.948, t=-2.098, P=0.012)。男性、文化程度在小学及以下的、年龄在35岁及以下的患者更倾向为消极管理型。 结论 根据生活方式管理、药物管理行为的不同, 高血压患者自我管理类型可以分成4类。全面积极管理的患者SBP水平低于消极管理型, 未来对于高血压患者的管理应注重依需求提升患者自我管理能力。 Abstract:Objective This study aims to identify the types of self-management employed by hypertensive patients, to assess their blood pressure control status, and to examine the relationship between the two. Methods A questionnaire survey and physical examinations were administered to hypertensive patients from the Daxing District in Beijing.Latent profile analysis was used to explore the self-management types.General linear regression was used to investigate the relationships between self-management types and blood pressure levels.Chi-square tests were used to examine the characteristics of self-management types. Results A total of 1 260 patients with hypertension were included in this study.Their self-management types could be categorized into four types: negative management (21.98%), lifestyle-positive management (9.68%), medication-positive management (32.22%) and comprehensive-positively management (36.12%).Compared with negative management type, the level of SBP in patients with comprehensive-positively management was significantly lower (β=-4.948, t=-2.098, P=0.012).Male patients, those with education below primary school level, and individuals under 35 years of age showed a tendency toward negative management practices. Conclusions According to different behaviors in lifestyle management and medication-taking, the self-management types of patients with hypertension can be divided into four types.Notably, the SBP levels in patients utilizing comprehensive-positive management were significantly lower compared to those following negative management practices.Future efforts should concentrate on enhancing patients′ self-management capabilities according to their specific needs. -
Key words:
- Hypertensive patients /
- Self-management types /
- Latent profile analysis /
- Blood pressure
-
表 1 血压水平影响因素的一般线性回归
Table 1. General linear regression of factors influencing blood pressure
变量 SBP/mmHg DBP/mmHg β sx t值 β sx t值 性别 男 4.003 1.199 3.338 ① 5.168 0.778 6.639 ① 女 年龄/岁 0.177 0.056 3.147 ② -0.304 0.036 -0.855 ① 病程/年 0.168 0.073 2.285 ② 0.087 0.478 1.821 文化程度 初中 -1.366 1.734 -0.787 0.660 1.122 0.588 高中 -3.580 1.912 -1.872 -0.885 1.235 -0.717 大专及以上 -6.014 2.262 -2.658 ② -3.043 1.466 -2.074 ② 小学及以下 自我管理类型 全面积极管理 -4.948 2.358 -2.098 ② 积极药物管理 -3.943 2.388 -1.651 积极生活方式管理 -0.047 2.614 -0.182 消极管理 注: ① P<0.001。② P<0.05。 表 2 高血压患者自我管理类型与一般人口学特征的关系
Table 2. Relationship between self-management types and demographic characteristics in hypertensive patients
一般人口学特征 消极管理/[人数(占比/%)] 积极生活方式管理/[人数(占比/%)] 积极药物管理/[人数(占比/%)] 全面积极管理/[人数(占比/%)] χ2值 P值 性别 11.516 0.009 男 175(24.93) 62(8.83) 232(33.05) 233(33.19) 女 102(18.28) 60(10.75) 174(31.18) 222(39.79) 年龄组/岁 188.120 <0.001 ≤35 81(53.64) 30(19.87) 17(11.26) 23(15.23) >35~45 40(24.54) 27(16.56) 39(23.93) 57(34.97) >45~55 63(18.64) 40(11.83) 105(31.07) 130(38.46) >55~65 44(13.97) 16(5.08) 127(40.32) 128(40.63) >65 49(16.73) 9(3.07) 118(40.27) 117(39.93) 人均月收入/元 18.400 0.005 <3 000 133(21.66) 42(6.84) 217(35.34) 222(36.16) 3 000~<5 000 94(21.66) 47(10.83) 134(30.87) 159(36.64) ≥5 000 50(23.58) 33(15.57) 55(25.94) 74(34.91) 文化程度 32.738 <0.001 小学及以下 38(18.10) 15(7.14) 92(43.81) 65(30.95) 初中 116(22.18) 44(8.41) 178(34.04) 185(35.37) 高中 59(20.07) 31(10.54) 80(27.21) 124(42.18) 大专及以上 27(16.98) 19(11.95) 50(31.45) 63(39.62) 婚姻状况 3.121 0.373 已婚 260(21.96) 119(10.05) 379(32.01) 426(35.98) 未婚 17(22.36) 3(3.95) 27(35.53) 29(38.16) 病程① /年 48.243 <0.001 ≤5 84(18.58) 53(11.73) 153(33.85) 162(35.84) >5~10 38(13.29) 8(2.80) 105(36.71) 135(47.20) >10 17(7.30) 9(3.86) 99(42.49) 108(46.35) 注:①表示采用有效应答样本。 -
[1] Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015[J]. Circulation, 2018, 137(22): 2344-2356. DOI: 10.1161/CIRCULATIONAHA.117.032380. [2] Li R, Liang N, Bu F, et al. The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis[J]. JMIR Mhealth Uhealth, 2020, 8(3): e17776. DOI: 10.2196/17776. [3] Van Truong P, Wulan Apriliyasari R, Lin MY, et al. Effects of self-management programs on blood pressure, self-efficacy, medication adherence and body mass index in older adults with hypertension: Meta-analysis of randomized controlled trials[J]. Int J Nurs Pract, 2021, 27(2): e12920. DOI: 10.1111/ijn.12920. [4] 谢菁, 张晨韵, 林皞, 等. 自我管理干预对高血压患者血压影响的Meta分析[J]. 中国预防医学杂志, 2019, 20(2): 92-97. DOI: 10.16506/j.1009-6639.2019.02.003.Xie J, Zhang CY, Lin G, et al. The impact of self-management intervention on blood pressure control: A meta analysis[J]. Chin Prev Med, 2019, 20(2): 92-97. DOI: 10.16506/j.1009-6639.2019.02.003. [5] 中国高血压防治指南修订委员会, 高血压联盟(中国), 中华医学会心血管病学分会, 等. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019, 24(1): 24-56. DOI: 10.3969/j.issn.1007-5410.2019.01.002.Writing Group of 2018 Chinese Guidelines for the Management of Hypertension, Chinese Hypertension League, Chinese Society of Cardiology, et al. 2018 Chinese guidelines for the management of hypertension[J]. Chin J Cardiovasc Med, 2019, 24(1): 24-56. DOI: 10.3969/j.issn.1007-5410.2019.01.002. [6] 吕金林, 李慧慧, 单雨薇, 等. 高血压患者自我管理干预模式的研究进展[J]. 中国慢性病预与防制, 2020, 28(1): 64-66. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.01.016.Lyu JL, Li HH, Shan YW, et al. Research progress of self-management intervention model for hypertensive patients[J]. Chin J Preve Contr Chron Dis, 2020, 28(1): 64-66. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.01.016. [7] Prochaska JO, Velicer WF. The transtheoretical model of health behavior change[J]. Am J Health Promot, 1997, 12(1): 38-48. DOI: 10.4278/0890-1171-12.1.38. [8] Mastellos N, Gunn LH, Felix LM, et al. Transtheoretical model Q16 stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults[J]. Cochrane DB Syst Rev, 2014, 2(2): CD008066, DOI: 10.1002/14651858.CD008066.pub3. [9] Vilamala-Orra M, Vaque-Crusellas C, Foguet-Boreu Q, et al. Applying the stages of change model in a nutrition education programme for the promotion of fruit and vegetable consumption among people with severe mental disorders (DIETMENT)[J]. Nutrients, 2021, 13(6): 2105. DOI: 10.3390/nu13062105. [10] 洪秀敏, 刘倩倩. 父母养育压力的类型及其影响因素——基于一孩父母和两孩父母的潜在剖面分析[J]. 中国临床心理学杂志, 2020, 28(4): 766-772. DOI: 10.16128/j.cnki.1005-3611.2020.04.025.Hong XM, Liu QQ. Types of parenting stress and its influencing factors——Based on latent profile analysis of one-child parents and two-child parents[J]. Chin J Clin Psychol, 2020, 28(4): 766-772. DOI: 10.16128/j.cnki.1005-3611.2020.04.025. [11] 王孟成, 毕向阳. 潜变量建模与Mplus应用: 进阶篇[M]. 重庆: 重庆大学出版社, 2018: 13-15.Wang MC, Bi XY. Latent variable modeling and Mplus application: Advanced[M]. Chongqing: Chongqing university press, 2018: 13-15. [12] N. Guess, L. Vasantharajah, M. Gulliford, et al. Improvements in stage of change correlate to changes in dietary intake and clinical outcomes in a 5-year lifestyle intervention in young high-risk Sri Lankans[J]. Prev Med, 2016, 90: 193-200. DOI: 10.1016/j.ypmed.2016.07.011. [13] Pérez-Tortosa S, Roig L, Manresa JM, et al. Continued smoking abstinence in diabetic patients in primary care: a cluster randomized controlled multicenter study[J]. Diabetes Res Clin Pract, 2015, 107(1): 94-103. DOI: 10.1016/j.diabres.2014.09.009. [14] Shen Y, Wang T, Gao M, et al. Association of glucose control and stages of change for multiple self-management behaviors in patients with diabetes: A latent profile analysis[J]. Patient Educ Couns, 2020, 103(1): 214-219. DOI: 10.1016/j.pec.2019.08.020. [15] 程学娟. 高血压患者自我管理行为及影响因素的健康生态学模型解释[D]. 济南: 山东大学, 2014.Cheng XJ. The predicators of self-management behavior in patients with hypertension based on Health Ecological Model[D]. Jinan: Shandong University, 2014. [16] Zhang XN, Qiu C, Zhang YZ, et al. Self-management Among Elderly Patients With Hypertension and Its Association With Individual and Social Environmental Factors in China[J]. J Cardiovasc Nurs, 2020, 35(1): 45-53. DOI: 10.1097/JCN.0000000000000608. [17] Neal B, Wu Y, Feng X, et al. Effect of Salt Substitution on Cardiovascular Events and Death[J]. N Engl J Med, 2021, 385(12): 1067-1077. DOI: 10.1056/NEJMoa2105675. [18] 刘晓, 赵秋利, 李金秀, 等. 高血压患者的自我管理水平及其影响因素[J]. 解放军护理杂志, 2013, 30(20): 5-8. DOI: 10.3969/j.issn.1008-9993.2013.20.002.Liu X, Zhao QL, Li JX, et al. Self-management level and its influencing factors among patients with hypertension[J]. Nurs J Chin PLA, 2013, 30(20): 5-8. DOI: 10.3969/j.issn.1008-9993.2013.20.002. -





 下载:
下载: