Associations between albumin, globulin, albumin to globulin ratio and electrocardiographic abnormalities among people living with HIV
-
摘要:
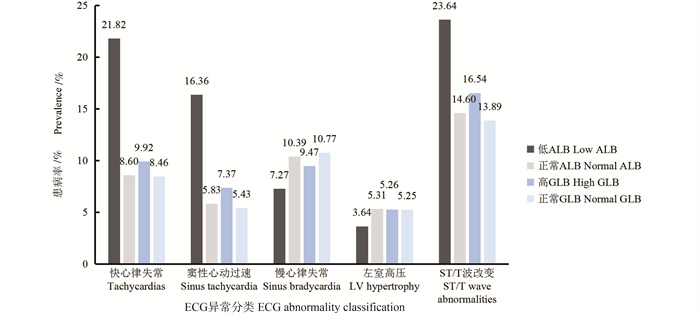
目的 了解HIV感染者的血清白蛋白(albumin, ALB)、球蛋白(globulin, GLB)和白球蛋白比例(albumin to globulin ratio, AGR)与心电图(electrocardiograph, ECG)异常之间的关联性。 方法 采用横断面研究的方法,选自2017-2018年“HIV与衰老相关疾病前瞻性队列研究”基线数据,纳入1 788例18~<75岁的HIV感染者进行分析。低ALB定义为血清ALB < 38 g/L,高GLB定义为血清GLB>35 g/L,低AGR定义为AGR≤1.5,ECG异常定义为出现任何心电图结果异常。采用多因素logistic回归分析模型分析ALB、GLB和AGR与ECG异常的关联性。 结果 ECG异常、快心律失常、窦性心动过速、ST/T段异常和左室高电压的患病率分别为41.16%(736/1 788)、9.00%(161/1 788)、6.15%(110/1 788)、14.88%(266/1 788)和5.26%(94/1 788)。3.08%(55/1 788)的研究对象为低ALB,37.19%(665/1 788)为高GLB,65.49%(1 171/1 788)为低AGR。多因素logistic回归分析模型结果显示,调整年龄、性别、ALT、AST、BMI、高血压、HIV特异性变量等之后,低ALB是窦性心动过速(aOR=4.89, 95% CI: 1.96~12.20, P=0.001)和快心律失常(aOR=3.24, 95% CI: 1.50~6.99, P=0.003)的独立影响因素。高GLB是窦性心动过速的独立影响因素(aOR=1.66, 95% CI: 1.00~2.74, P=0.049),而与其他ECG异常差异均无统计学意义(均P>0.05)。AGR降低与窦性心动过速差异均无统计学意义(均P>0.05)。 结论 HIV感染者存在较高比例的白球蛋白水平异常。低ALB和高GLB是窦性心动过速的独立危险因素,提示异常的白球蛋白水平可能侧面反映较高的炎症反应状态,可为预测该人群心血管疾病的发病风险提供新的线索和依据,但其中的因果关系和机制需要进一步研究。 Abstract:Objective To investigate the associations of serum albumin (ALB), globulin (GLB), albumin to globulin ratio (AGR) with electrocardiographic (ECG) abnormalities among people living with HIV. Methods This cross-sectional investigation included 1 788 between 18- < 75 years old from the baseline survey of Comparative HIV and Aging Research in Taizhou (CHART) cohort China from 2017 to 2018. We defined low ALB as serum ALB < 38 g/L, high GLB as serum GLB>35 g/L, low AGR as AGR≤1.5, ECG abnormalities as the presence of any ECG abnormal manifestations. Multivariable logistic regression model was used to analyze the associations of ALB, GLB, AGR with ECG abnormalities. Results The prevalence of ECG abnormalities, tachycardia, sinus tachycardia, ST/T wave abnormalities and LV hypertrophy was 41.16% (736/1 788), 9.00% (161/1 788), 6.15% (110/1 788), 14.88% (266/1 788) and 5.26% (94/1 788), respectively. About 3.08% (55/1 788) of participants had low ALB, 37.19% (665/1 788) had high GLB and 65.49% (1 171/1 788) had low AGR. After adjusting for traditional risk factors including age, sex, ALT, AST, BMI, hypertension and HIV-specific factors, low ALB was independently associated with sinus tachycardia (aOR=4.89, 95% CI: 1.96-12.20, P=0.001) and tachycardia (aOR =3.24, 95% CI: 1.50-6.99, P=0.003), and high GLB was independently associated with sinus tachycardia only (aOR=1.66, 95% CI: 1.00-2.74, P=0.049). However, no statistically significant association was found for any other ECG abnormalities (all P>0.05). And there was no statistical significance between low AGR and sinus tachycardia (all P>0.05). Conclusions Abnormal ALB and/or GLB levels are common among PLWH. The independently positive associations of low ALB, high GLB and low AGR with sinus tachycardia suggest that abnormal albumin and globulin levels may reflect the elevated inflammatory state in PLWH and thus may provide new evidence for better predicting cardiovascular disease risk among PLWH. However, the causation and underlying mechanisms need to be further investigated. -
Key words:
- HIV /
- Electrocardiographic abnormalities /
- Sinus tachycardia /
- Albumin /
- Globulin /
- Albumin to globulin ratio /
- Association
-
图 2 低ALB(A)和高GLB(B)与各ECG异常的关联分析
模型1为校正年龄和性别; 模型2为模型1基础上加入校正AST、ALT、BMI、腹部肥胖、吸烟、饮酒、高血压、糖尿病、血脂、运动; 模型3为模型2基础上加入校正HIV特异性变量。
Figure 2. Associations between ALB (A), GLB (B) and ECG abnormalities
Model 1 adjusted for age and sex; Model 2 adjusted for all variables in model 1 plus AST, ALT, BMI, abdominal obesity, smoking status, alcohol, hypertension, diabetes, dyslipidemia and exercise; Model 3 adjusted for all variables in model 2 plus HIV-specific determinants.
表 1 不同ALB和GLB水平HIV感染者基本特征
Table 1. Basic characteristics of people living with HIV at different ALB and GLB levels
特征Feature 合计(n=1 788)Total(n=1 788) ALB t/Z/χ2值t/Z/χ2 value P值P value GLB t/Z/χ2值t/Z/χ2 value P值P value 正常(n=1 733)Normal(n=1 733) < 38/(g·L-1)(n=55) 正常(n=1 123)Normal(n=1 123) >35/(g·L-1)(n=665) 年龄组/岁, (x±s) Age group/years, (x±s) 43.8±14.1 43.5±14.1 53.4±13.4 5.15 < 0.001 42.4±13.6 46.2±14.6 5.53 < 0.001 性别Sex 0.01 0.969 4.75 0.029 女Female 394(22.04) 382(96.95) 12(3.05) 229(58.12) 165(41.88) 男Male 1 394(77.96) 1 351(96.92) 43(3.08) 894(64.13) 500(35.86) 腹部肥胖① Abdominal obesity 2.38 0.123 4.45 0.035 否No 961(53.84) 937(97.50) 24(2.50) 625(65.04) 336(35.96) 是Yes 824(96.16) 793(96.24) 31(3.76) 496(60.19) 328(39.81) BMI/(kg·m-2), [M(P25, P75)] 22.0(20.0, 24.1) 22.0(20.1, 24.2) 19.6(18.0, 22.2) 27.49 < 0.001 21.8(20.0, 24.0) 22.2(20.2, 24.2) 2.45 0.118 吸烟Smoking status 0.83 0.661 1.95 0.378 从不Never 1 068(59.73) 1 038(97.19) 30(2.81) 665(62.27) 403(37.73) 曾经Ever 229(12.81) 222(96.94) 7(3.06) 138(60.26) 91(39.74) 现在Current 491(27.46) 473(96.33) 18(3.67) 320(65.17) 171(34.83) 饮酒Alcohol - 0.514 ③ 0.34 0.559 否No 1 706(95.41) 1 652(96.83) 54(3.17) 1 069(62.66) 637(37.34) 是Yes 82(4.59) 81(98.78) 1(1.22) 54(65.85) 28(34.15) 运动Exercise 1.99 0.159 5.64 0.018 否No 1 244(69.57) 1 201(96.54) 43(3.46) 759(61.01) 485(38.99) 是Yes 544(30.43) 532(97.79) 12(2.21) 364(66.91) 180(33.09) 糖尿病Diabetes - < 0.001 ③ 4.80 0.028 否No 1 682(94.07) 1 640(97.50) 42(2.50) 1 067(63.44) 615(36.56) 是Yes 106(5.93) 93(87.74) 13(12.26) 56(52.83) 50(47.17) 血脂异常Dyslipidemia 18.73 < 0.001 2.11 0.147 否No 760(42.51) 721(94.87) 39(5.13) 492(64.74) 268(35.26) 是Yes 1 028(57.49) 1 012(98.44) 16(1.56) 631(61.38) 397(38.62) 高血压Hypertension 1.08 0.298 2.76 0.097 否No 1 393(77.91) 1 347(96.70) 46(3.30) 889(63.82) 504(36.18) 是Yes 395(22.09) 386(97.72) 9(2.28) 234(59.24) 161(40.76) AST/(U·L-1)[M(P25, P75)] 29.0(22.0, 41.0) 29.0(22.0, 40.0) 39.0(26.0, 60.0) 17.30 < 0.001 28.0(21.0, 39.0) 32.0(25.0, 44.0) 42.62 < 0.001 ALT/(U·L-1)[M(P25, P75)] 17.0(12.0, 27.0) 17.0(12.0, 27.0) 16.0(10.0, 32.0) 0.75 0.385 18.0(12.0, 27.0) 17.0(12.0, 27.0) 0.25 0.621 AGR, (x±s) 1.40±0.30 1.42±0.28 0.78±0.20 23.32 < 0.001 1.57±0.22 1.13±0.19 44.84 < 0.001 低AGR Low AGR 29.90 < 0.001 553.02 < 0.001 否No 617(34.51) 614(99.51) 3(0.49) 616(99.84) 1(0.16) 是Yes 1 171(65.49) 1 116(95.30) 55(4.70) 507(43.30) 664(56.70) HIV特异性变量HIV-specific determinants HIV诊断时间/年Time since HIV diagnosis/years 3.70 0.055 27.49 < 0.001 < 3 1 077(60.23) 1 037(96.29) 40(3.71) 624(57.94) 453(42.06) ≥3 711(39.77) 696(97.89) 15(2.11) 499(70.18) 212(29.82) 当前CD4计数/(个·μL-1) Current CD4 count /(cells·μL-1) 67.78 < 0.001 125.51 < 0.001 < 200 296(16.55) 265(89.53) 31(10.47) 118(39.86) 178(60.14) 200~ < 350 437(24.44) 425(97.25) 12(2.75) 237(54.23) 200(45.77) ≥350 1 055(59.00) 1 043(98.86) 12(1.14) 768(72.80) 287(27.20) 病毒载量/(拷贝·mL-1) Viral load /(copies·mL-1) 4.18 0.124 33.71 < 0.001 缺失None 1 406(78.64) 1 366(97.15) 40(2.84) 913(64.94) 493(35.06) < 200 149(8.33) 146(97.99) 3(2.01) 103(69.13) 46(30.87) ≥200 233(13.03) 221(94.84) 12(5.15) 107(45.92) 126(54.08) cART开始时间/年cART initiation time /years 4.95 0.084 41.30 < 0.001 未接受过Never 14(0.78) 14(100.00) 0(0) 6(42.90) 8(57.10) < 3 1 221(68.29) 1 176(96.31) 45(3.69) 710(58.15) 511(41.85) ≥3 553(30.93) 543(98.19) 10(1.81) 407(73.60) 146(26.40) cART用药方案② cART medication regimen - 0.152 ③ - 0.054 ③ 2NRTIs+1NNRTI (NVP/EFV) 1 751(98.70) 1 698(96.97) 53(3.03) 1 104(63.05) 647(36.95) 2NRTIs/NNRTI+PI 11(0.62) 10(90.91) 1(9.09) 9(81.82) 2(18.18) 其他Other 12(0.68) 11(91.67) 1(8.33) 4(33.33) 8(66.67) 注:AST,谷草转氨酶; ALT,谷丙转氨酶; AGR, 白球比; cART:联合抗病毒治疗; NRTI, 核苷类反转录酶抑制剂; NNRTI, 非核苷类反转录酶抑制剂; NVP, 奈韦拉平; EFV, 依菲伦韦; PI, 蛋白酶抑制剂; ALB, 血清白蛋白; GLB, 血清球蛋白; cART类型中的“其他”包括均为NRTI或整合酶抑制剂+2NRTIs。
①为数据缺失,腹部肥胖缺失3例。②为排除未进行cART后样本量为1 774。③为采用Fisher确切概率法。
Note:AST: aspartate aminotransferase; ALT, alanine aminotransferase; AGR, albumin to globulin ratio; cART: combined antiretroviral therapy; NRTI, nucleoside reverse transcriptase inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor; NVP: Nevirapine; EFV: Efavirenz; PI: protease inhibitor; ALB, albumin; GLB, globulin; Others: both NRTI or integrated inhibitors+2NRTIs.
① data not applicable,cases were not measured for abdominal obesity. ② after excluded the no cART, 1 774 were included. ③ Fisher′s Exact Test.表 2 ALB、GLB、AGR与窦性心动过速的关联分析
Table 2. Associations between ALB, GLB, AGR and sinus tachycardia
模型Model ALB GLB AGR 正常Normal < 38/(g·L-1) 正常Normal >35/(g·L-1) >1.5 ≤1.5 模型1 Model 1 1.00 4.78(2.20~10.39) ① 1.00 1.58(1.07~2.35) ② 1.00 1.35(0.88~2.05) 模型2 Model 2 1.00 4.76(1.97~11.54) ① 1.00 1.69(1.02~2.82) ② 1.00 1.35(0.88~2.07) 模型3 Model 3 1.00 4.89(1.96~12.20) ① 1.00 1.66(1.00~2.74) ② 1.00 1.37(0.88~2.13) 模型4 Model 4 1.00 1.00(0.94~1.05) 1.00 1.05(1.02~1.08) ① 1.00 1.99(1.02~3.89) ② 模型5 Model 5 1.00 1.00(0.94~1.06) 1.00 1.04(1.01~1.07) ② 1.00 1.91(0.96~3.77) ③ 模型6 Model 6 1.00 1.00(0.94~1.06) 1.00 1.04(1.01~1.08) ① 1.00 2.03(0.96~4.29) ③ 注:1. ALB, 血清白蛋白; GLB, 血清球蛋白; AGR, 白球比。
2. 模型1和4调整年龄和性别; 模型2和5为在模型1和4的基础上加入AST、ALT、BMI、吸烟、饮酒、高血压、糖尿病、血脂、运动; 模型3和6为在模型2和5的基础上加入HIV特异性变量; 模型1~3为ALB、GLB和AGR以分类变量纳入; 模型4~6为ALB、GLB和AGR以连续性变量纳入。
① P < 0.01。② P < 0.05。③ P < 0.10。
Note: 1. ALB, albumin; GLB, globulin; ECG, electrocardiograph.
2. Model 1 and model 4 adjusted for age and sex; Model 2 and model 5 adjusted for all variables in model 1 and 4 plus AST, ALT, BMI, abdominal obesity, smoking status, alcohol, hypertension, diabetes, dyslipidemia and exercise; Model 3 and model 6 adjusted for all variables in model 2 and 5 plus HIV-specific determinants; Model 1-3 adjusted for ALB, GLB and AGR as binomial; Model 4-6 adjusted for ALB, GLB and AGR as continuous.
① P < 0.01. ② P < 0.05. ③ P < 0.10. -
[1] Shah ASV, Stelzle D, Lee KK, et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: systematic review and meta-analysis[J]. Circulation, 2018, 138(11): 1100-1112. DOI: 10.1161/CIRCULATIONAHA.117.033369. [2] Alonso A, Barnes AE, Guest JL, et al. HIV infection and incidence of cardiovascular diseases: an analysis of a large healthcare database[J]. J Am Heart Assoc, 2019, 8(14): e012241. DOI: 10.1161/JAHA.119.012241. [3] Auer R, Bauer DC, Marques-Vidal P, et al. Association of major and minor ECG abnormalities with coronary heart disease events[J]. JAMA, 2012, 307(14): 1497-1505. DOI: 10.1001/jama.2012.434. [4] Soliman EZ, Prineas RJ, Roediger MP, et al. Prevalence and prognostic significance of ECG abnormalities in HIV-infected patients: results from the Strategies for Management of Antiretroviral Therapy study[J]. J Electrocardiol, 2011, 44(6): 779-785. DOI: 10.1016/j.jelectrocard.2010.10.027. [5] Niedziela JT, Hudzik B, Szygula-Jurkiewicz B, et al. Albumin-to-globulin ratio as an independent predictor of mortality in chronic heart failure[J]. Biomark Med, 2018, 12(7): 749-757. DOI: 10.2217/bmm-2017-0378. [6] Nozarian Z, Mehrtash V, Abdollahi A, et al. Serum protein electrophoresis pattern in patients living with HIV: frequency of possible abnormalities in Iranian patients[J]. Iran J Microbiol, 2019, 11(5): 440-447. [7] Chwiki S, Campos MM, McLaughlin ME, et al. Adverse effects of antiretroviral therapy on liver hepatocytes and endothelium in HIV patients: an ultrastructural perspective[J]. Ultrastruct Pathol, 2017, 41(2): 186-195. DOI: 10.1080/01913123.2017.1282066. [8] 刘宝莲, 康英芳, 王花, 等. 艾滋病患者血液学检验异常的临床价值研究[J]. 中国药物与临床, 2020, 20(17): 2947-2948. DOI: 10.11655/zgywylc2020.17.057.Liu BL, Kang YF, Wang H, et al. Study on the clinical value of abnormal hematology test in AIDS patients[J]. Chinese Remedies Clinics, 2020, 20(17): 2947-2948. DOI: 10.11655/zgywylc2020.17.057. [9] 杨婧, 方永辉, 谢周华. 获得性免疫缺陷综合征患者心电图临床特征分析[J]. 医学综述, 2016, 22(13): 2627-2629, 2636. DOI: 10.3969/j.issn.1006-2084.2016.13.038.Yang J, Fang YH, Xie ZH. Analysis of the characteristic of electrocardiograms with abnormal biochemical indexes of AIDS patients[J]. Med Recapitul, 2016, 22(13): 2627-2629, 2636. DOI: 10.3969/j.issn.1006-2084.2016.13.038. [10] Pignatelli P, Farcomeni A, Menichelli D, et al. Serum albumin and risk of cardiovascular events in primary and secondary prevention: a systematic review of observational studies and Bayesian meta-regression analysis[J]. Intern Emerg Med, 2020, 15(1): 135-143. DOI: 10.1007/s11739-019-02204-2. [11] Prineas RJ, Crow RS, Zhang ZM. The minnesota code manual of electrocardiographic findings[M]. London: Springer London, 2010: 16-186. [12] Cai Y, Zhao Y, Dai QX, et al. Prognostic value of the albumin-globulin ratio and albumin-globulin score in patients with multiple myeloma[J]. J Int Med Res, 2021, 49(3): 300060521997736. DOI: 10.1177/0300060521997736. [13] Li K, Fu WR, Bo YC, et al. Effect of albumin-globulin score and albumin to globulin ratio on survival in patients with heart failure: a retrospective cohort study in China[J]. BMJ Open, 2018, 8(7): e022960. DOI: 10.1136/bmjopen-2018-022960. [14] Yu LP, Ye XJ, Yang ZJ, et al. Prevalences and associated factors of electrocardiographic abnormalities in Chinese adults: a cross-sectional study[J]. BMC Cardiovasc Disord, 2020, 20(1): 414. DOI: 10.1186/s12872-020-01698-5. [15] Krishnan MN, Geevar Z, Venugopal KN, et al. A community-based study on electrocardiographic abnormalities of adult population from South India - Findings from a cross sectional survey[J]. Indian Heart J, 2022, 74(3): 187-193. DOI: 10.1016/j.ihj.2022.05.001. [16] Osna N, Poluektova L. hepatitis C (HCV) and human immunodeficiency virus (HIV) infections promote liver fibrosis development by potentiation of liver cell death[J]. Gastroenterol Hepatol Open Access, 2018, 9(2): 72-73. DOI: 10.15406/ghoa.2018.09.00297. [17] Koethe JR, Blevins M, Nyirenda C, et al. Nutrition and inflammation serum biomarkers are associated with 12-week mortality among malnourished adults initiating antiretroviral therapy in Zambia[J]. J Int AIDS Soc, 2011, 14: 19. DOI: 10.1186/1758-2652-14-19. [18] Zemlin AE, Ipp H, Maleka S, et al. Serum protein electrophoresis patterns in human immunodeficiency virus-infected individuals not on antiretroviral treatment[J]. Ann Clin Biochem, 2015, 52(Pt 3): 346-351. DOI: 10.1177/0004563214565824. [19] Khan H, Kunutsor S, Kalogeropoulos AP, et al. Resting heart rate and risk of incident heart failure: three prospective cohort studies and a systematic meta-analysis[J]. J Am Heart Assoc, 2015, 4(1): e001364. DOI: 10.1161/JAHA.114.001364. [20] Opdahl A, Venkatesh BA, Fernandes VRS, et al. Resting heart rate as predictor for left ventricular dysfunction and heart failure: mesa (Multi-Ethnic Study of Atherosclerosis)[J]. J Am Coll Cardiol, 2014, 63(12): 1182-1189. DOI: 10.1016/j.jacc.2013.11.027. -





 下载:
下载: