Exploring the influencing factors of antenatal depression based on random forest algorithm and multivariate logistic regression model
-
摘要:
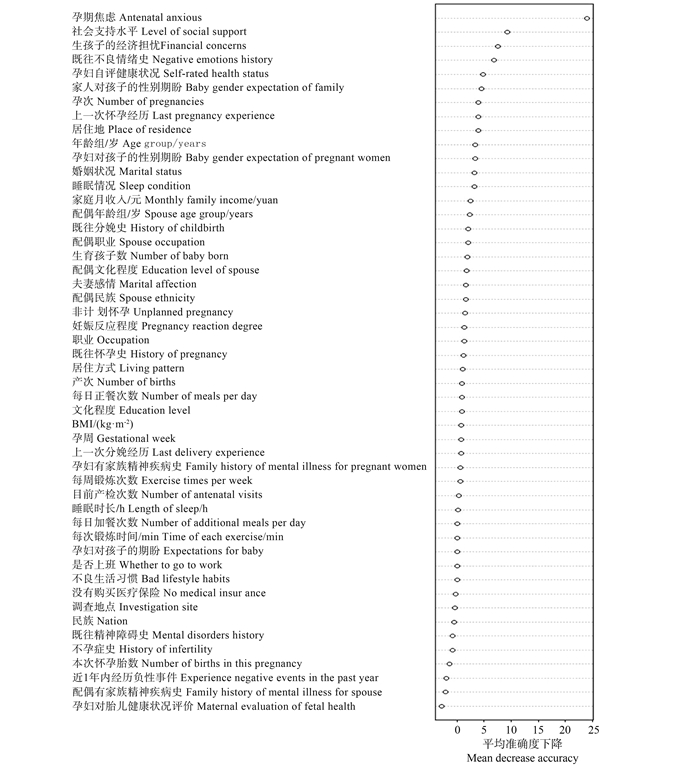
目的 分析孕期抑郁检出率探讨可能的影响因素,识别高危人群为预防抑郁症提供科学依据。 方法 对云南省某县2022年5月处于孕期的女性人群采用爱丁堡产后抑郁症量表(Edinburgh Postnatal Depression Scale,EPDS)进行抑郁筛查,利用随机森林算法对影响因素进行重要性排序,用滑动窗口序贯向前选择法降维,将重要性评分最高且平均袋外估算误差率最小的影响因素纳入多因素logistic回归分析模型,估计影响因素的作用方向及效应值。 结果 732名孕妇接受问卷筛查,孕期抑郁检出率为13.8%(101/732)。随机森林算法分析显示,变量数为7时平均袋外估算误差率最小。将重要性排名前7的影响因素纳入多因素logistic回归分析模型,结果显示:孕期焦虑、既往不良情绪史、生孩子的经济担忧、家人对孩子有性别期盼是孕期抑郁的危险因素,第2次怀孕、高社会支持水平是孕期抑郁的保护因素,孕妇自评健康状况不满意与孕期抑郁无关。 结论 孕期有焦虑的女性很可能伴有抑郁,对生育费用、孩子性别的担忧和既往的不良情绪史会增加孕期抑郁的风险,足够的社会支持和既往的孕育史可以减少孕期抑郁发生的风险。建议加强孕期抑郁筛查,早期识别孕期抑郁症的高危人群。 -
关键词:
- 孕期抑郁 /
- 随机森林算法 /
- 多因素logistic回归分析模型 /
- 影响因素
Abstract:Objective To analyze the prevalence of antenatal depression, to explore the possible influencing factors of antenatal depression, and and to recognize high-risk groups, thereby contributing to prevention strategies. Methods In May 2022, pregnant women in a county of Yunnan Province were surveyed and antenatal depression were screened by Edinburgh Postpartum Depression Scale (EPDS). Random forest algorithm was adopted to rank the importance of the influencing factors of antenatal depression. The sliding window sequential forward selection method was employed to decide the number of influencing factors. The influencing factors with the highest importance score and the lowest out-of-bag error were incorporated into the Multivariate logistic regression model to estimate the effect size. Results A total of 732 pregnant women were screened by questionnaire, the prevalence of antenatal depression was 13.8% (101/732).The out-of-bag error was lowest when the number of influencing factors was 7 based on random forest algorithm and sliding window sequential forward selection. We included the top 7 influencing factors in the logistic regression model, and the results showed that antenatal anxious, history of negative emotions, financial concerns of having children, and baby gender expectation were the risk factors for antenatal depression. In contrast, the second pregnancy, high social support were the protective factors. Self-reported poor health was found unrelated to antenatal depression. Conclusions Women with anxiety during pregnancy are more likely to develop depression. The concerns of financial costs, baby gender and bad emotions experience increase the risk of triggering depression during pregnancy, while the adequate social support and pregnancy experience reduce the risk. It is recommended that high-risk group screening should be given to women during the pregnancy to prevent antenatal depression. -
表 1 孕期抑郁影响因素及赋值
Table 1. Influencing factors for antenatal depression and variable assignments
影响因素Influencing factor 赋值情况Assignment situation 年龄组/岁Age group/years 1=<25,2=25~<30,3=30~<35,4=≥35 BMI/(kg·m-2) 1=<18.5,2=18.5~<24.0,3=24.0~<28.0,4=≥28.0 职业Occupation 1=公务员/企事业/教师/医务人员,2=农民/工人,3=个体从业/自由/其他,4=待业/无业
1=Civil servants/Enterprises/Teachers/Medical personnel, 2=Farmers/Workers, 3=Self-employed/Free/Other, 4=Unemployed/Unemployed居住方式Living pattern 1=与丈夫,2=与丈夫及其父母,3=与丈夫及自己父母,4=独自一人/与其他亲朋好友
1=Husband, 2=Husband and his parents, 3=Husband and my parents, 4=Alone/With other family and friends配偶年龄组/岁Spouse age group/years 1=<25,2=25~<30,3=30~<35,4=≥35 配偶职业Spouse occupation 1=公务员/企事业/教师/医务人员,2=农民/工人,3=个体从业/自由/其他,4=待业/无业
1=Civil servants/Enterprises/Teachers/Medical personnel, 2=Farmers/Workers, 3=Self-employed/Free/Other, 4=Unemployed/Unemployed调查地点Investigation site 0=入户,1=医疗机构,2=基层卫生机构,3=社区
0=Household, 1=Medical institution, 2=Primary health institution, 3=Community婚姻状况Marital status 1=未婚/离婚,2=初婚,3=再婚
1=Unmarried/Divorced, 2=First marriage, 3=Remarriage文化程度Education level 0=初中及以下,1=高中及以上
0=Junior high school or below, 1=High school or above每日加餐次数Number of additional meals per day 1=0, 2=1~<3, 3=≥3 孕周Gestational week 1=4~<13, 2=13~<28, 3=≥28 孕次Number of pregnancies 1=1, 2=2, 3=3~<7, 4=≥7 民族Nation 0=汉族,1=壮族,2=苗族,3=其他少数民族
0=Han, 1=Zhuang, 2=Miao, 3=Other Ethnic Minorities配偶民族Spouse ethnicity 0=汉族,1=壮族,2=苗族,3=其他少数民族
0=Han, 1=Zhuang, 2=Miao, 3=Other ethnic minorities每日正餐次数Number of meals per day 1=1,2=2,3=3 睡眠情况Sleep condition 0=正常,1=不正常0 = Normal, 1 = Abnormal 夫妻感情Marital affection 0=好,1=差/一般0=Good, 1=Poor/Average 居住地Place of residence 0=城镇,1=农村0 = Town, 1 = Country 产次Number of births 1=0,2=≥1 非计划怀孕Unplanned pregnancy 0=无,1=有0=No, 1=Yes 既往怀孕史History of pregnancy 0=无,1=有0=No, 1=Yes 是否上班Whether to go to work 0=否,1=是0=No, 1=Yes 睡眠时长/h Length of sleep/h 0=<7,1=7~<9,2=≥9 不孕症史History of infertility 0=无,1=有0=No, 1=Yes 孕期焦虑Antenatal anxious 0=无,1=有0=No, 1=Yes 孕妇对胎儿健康状况评价Maternal evaluation of fetal health 0=满意,1=不满意0=Satisfied, 1=Dissatisfied 孕妇自评健康状况Self-rated health status 0=满意,1=不满意0=Satisfied, 1=Dissatisfied 上一次分娩经历Last delivery experience 0=无,1=顺产,2=剖宫产/难产,3=死产,4=婴儿畸形/先天性疾病
0=None, 1=Natural delivery, 2=Cesarean section/Difficult delivery, 3=Stillbirth, 4=Infant malformation/Congenital disease孕妇对孩子的期盼Expectations for baby 0=很期盼,1=一般,2=无所谓0=Expected, 1=Average, 2=Indifferent 家庭月收入/元Monthly family income/yuan 0=<5000, 1=≥5000 上一次怀孕经历Last pregnancy experience 0=无,1=正常,2=不正常0=No, 1=Normal, 2=Abnormal 配偶文化程度Education level of spouse 0=初中及以下,1=高中及以上0=Junior high school or below, 1=High school or above 目前产检次数Number of antenatal visits 1=1,2=2~<5,3=≥5 妊娠反应程度Pregnancy reaction degree 1=轻度,2=中度,3=重度1=Mild, 2=Moderate, 3=Severe 生育孩子数Number of baby born 1=0, 2=1, 3=2, 4=≥3 每次锻炼时间/min Time of each exercise/min 1=<30,2=≥30 每周锻炼次数Exercise times per week 1=<3,2=≥3 社会支持水平Level of social support 0=低度,1=高度0=Low degree, 1=High degree 本次怀孕胎数Number of births in this pregnancy 0=单胎,1=多胎0=Single birth, 1=Multiple birth 近1年内经历负性事件Experience negative events in the past year 0=无,1=有0=No, 1=Yes 孕妇对孩子的性别期盼Baby gender expectation of pregnant women 0=无,1=有0=No, 1=Yes 家人对孩子的性别期盼Baby gender expectation of family 0=无,1=有0=No, 1=Yes 孕妇有家族精神疾病史
Family history of mental illness for pregnant women0=否,1=是0=No, 1=Yes 配偶有家族精神疾病史Family history of mental illness for spouse 0=否,1=是0=No, 1=Yes 购买医疗保险Purchase medical insurance 0=否,1=是0=No, 1=Yes 生孩子的经济担忧Financial concerns 0=无,1=有0=No, 1=Yes 既往不良情绪史Negative emotions history 0=无,1=有0=No, 1=Yes 既往精神障碍史Mental disorders history 0=无,1=有0=No, 1=Yes 不良生活习惯Bad lifestyle habits 0=无,1=有0=No, 1=Yes 既往分娩史History of childbirth 0=无,1=有0=No, 1=Yes -
[1] Umuziga MP, Gishoma D, Hynie M, et al. Antenatal depressive symptoms in Rwanda: rates, risk factors, and social support[J]. BMC Pregnancy Childbirth, 2022, 22(1): 193. DOI: 10.1186/s12884-022-04522-4. [2] 胡焕青, 张继, 赵薇, 等. 中国6个县/区孕妇孕期焦虑、抑郁发生状况及影响因素[J]. 中华预防医学杂志, 2017, 51(1): 47-52. DOI: 10.3760/cma.j.issn.0253-9624.2017.01.010.Hu HQ, Zhang J, Zhao W, et al. The occurrence and determinants of anxiety and depression symptoms in women of six counties/districts in China during pregnancy[J]. Chin J Prev Med, 2017, 51(1): 47-52. DOI: 10.3760/cma.j.issn.0253-9624.2017.01.010. [3] Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item edinburgh postnatal depression scale[J]. Br J Psychiatry, 1987, 150(6): 782-786. DOI: 10.1192/bjp.150.6.782. [4] Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7[J]. Arch Intern Med, 2006, 166(10): 1092-1097. DOI: 10.1001/archinte.166.10.1092. [5] Zimet GD, Dahlem NW, Zimet SG, et al. The multidimensional scale of perceived social support[J]. J Pers Assess, 1988, 52(1): 30-41. DOI: 10.1207/s15327752jpa5201_2. [6] Jiang R, Tang WW, Wu XB, et al. A random forest approach to the detection of epistatic interactions in case-control studies[J]. BMC Bioinformatics, 2009, 10(Suppl 1): S65. DOI: 10.1186/1471-2105-10-S1-S65. [7] Tang X, Lu Z, Hu DH, et al. Influencing factors for prenatal Stress, anxiety and depression in early pregnancy among women in Chongqing, China[J]. J Affect Disord, 2019, 253: 292-302. DOI: 10.1016/j.jad.2019.05.003. [8] Zhang YD, Muyiduli X, Wang SJ, et al. Prevalence and relevant factors of anxiety and depression among pregnant women in a cohort study from south-east China[J]. J Reprod Infant Psychol, 2018, 36(5): 519-529. DOI: 10.1080/02646838.2018.1492098. [9] 王懿俏. 某省妇女产前保健服务可及性及影响因素研究[D]. 大连: 大连医科大学, 2017.Wang YQ. Study on the accessibility and influencing factors of prenatal health care services for women in a Province[D]. Dalian: Dalian Medical University, 2017. [10] Verreault N, Da Costa D, Marchand A, et al. Rates and risk factors associated with depressive symptoms during pregnancy and with postpartum onset[J]. J Psychosom Obstet Gynecol, 2014, 35(3): 84-91. DOI: 10.3109/0167482X.2014.947953. [11] 王颖, 王玉琼. 孕妇妊娠各期抑郁发生状况的纵向研究[J]. 解放军护理杂志, 2020, 37(7): 6-10. DOI: 10.3969/j.issn.1008-9993.2020.07.002.Wang Y, Wang YQ. Prenatal depression during different trimester of pregnancy: a prospective study[J]. Nurs J Chin PLA, 2020, 37(7): 6-10. DOI: 10.3969/j.issn.1008-9993.2020.07.002. [12] 张晓盼. 妊娠晚期孕妇产前抑郁的现状及主要影响因素的研究[D]. 合肥: 安徽医科大学, 2022.Zhang XP. Current situation of prenatal depression and main influencing factors of pregnant pregnant women[D]. Hefei: Anhui Medical University, 2022. [13] 龚瑜, 凌芝, 肖湘怡, 等. S-100B蛋白与妊娠抑郁焦虑状态的相关性研究[J]. 浙江医学, 2022, 44(9): 990-992. DOI: 10.12056/j.issn.1006-2785.2022.44.9.2021-2666.Gong Y, Ling Z, Xiao XY, et al. Study on the correlation between S-100B protein and pregnancy depression and anxiety[J]. Zhejiang Med J, 2022, 44(9): 990-992. DOI: 10.12056/j.issn.1006-2785.2022.44.9.2021-2666. [14] Philpott LF, Corcoran P. Paternal postnatal depression in Ireland: prevalence and associated factors[J]. Midwifery, 2018, 56: 121-127. DOI: 10.1016/j.midw.2017.10.009. [15] 刘晓, 孔令磷, 武倩, 等. 健康素养对围生期孕妇身体健康和心理健康状况的影响[J]. 中国妇幼保健, 2019, 34(6): 1224-1227. DOI: 10.7620/zgfybj.j.issn.1001-4411.2019.06.05.Liu X, Kong LL, Wu Q, et al. Influence of health literacy on physical health and mental health of perinatal pregnant women[J]. Maternal and Child Health Care of China, 2019, 34(6): 1224-1227. DOI: 10.7620/zgfybj.j.issn.1001-4411.2019.06.05. -





 下载:
下载: