-
摘要:
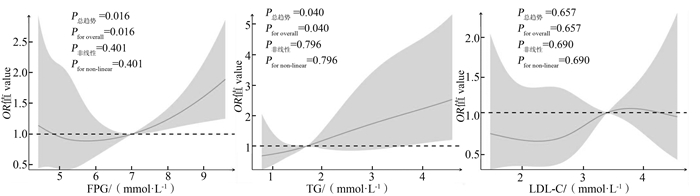
目的 基于队列人群研究心源性猝死(sudden cardiac death, SCD)的影响因素,为SCD的预防和病因学研究提供科学依据。 方法 采用巢式病例对照研究的方法,以金昌队列2011―2019年三次随访新发52例SCD者为病例组,按照年龄(±2岁)及同性别1∶4个体匹配的方法,以同期随访未发生SCD者的208例为对照组。用条件logistic回归分析模型分析金昌队列人群发生SCD的影响因素,并通过限制性立方样条(restricted cubic spline, RCS)模型拟合SCD发病风险的剂量-反应关系曲线。 结果 多因素条件logistic回归分析模型分析结果显示:三酰甘油(triglycerides, TG)(OR=2.94, 95% CI: 1.15~7.51)、低密度脂蛋白胆固醇(low density lipoprotein cholesterol, LDL-C)(OR=2.70, 95% CI: 1.18~6.22)、糖尿病(OR=5.59, 95% CI: 1.79~17.46)和心电图异常(OR=5.54, 95% CI: 2.11~14.56)是SCD的危险因素;文化程度在高中及以上(OR=0.33, 95% CI: 0.12~0.88)是SCD的保护因素。RCS结果显示:空腹血糖(fasting plasma glucose, FPG)、TG与SCD发病风险间呈正向线性剂量-反应关系(P总趋势<0.05,P非线性>0.05)。 结论 TG、LDL-C、糖尿病、心电图异常和文化程度与SCD的发生有关且FPG、TG与SCD的发生风险间存在线性剂量-反应关系。 Abstract:Objective To study the influencing factors of sudden cardiac death (SCD) based on the cohort population, and to provide basic data for the prevention and etiological research of SCD. Methods A nested case-control study was conducted, involving 52 newly diagnosed cases of SCD during three follow-up visits from 2011 to 2019 in Jinchang cohort. And 208 participants without SCD during the same period of follow-up were selected as the control group according to the matching method of age (±2 years) and 1∶4 individuals of the same sex. Conditional logistic regression model was used to analyze the influencing factors of SCD in Jinchang cohort, and the dose-response relationship of SCD risk was fitted by restricted cubic spline (RCS) models. Results Multivariate conditional logistic regression analysis showed that triglycerides (TG) (OR=2.94, 95% CI: 1.15-7.51), low density lipoprotein cholesterol (LDL-C) (OR=2.70, 95% CI: 1.18-6.22), diabetes (OR=5.59, 95% CI: 1.79-17.46) and abnormal electrocardiogram (OR=5.54, 95% CI: 2.11-14.56) were risk factors for SCD. Education level in high school and above (OR=0.33, 95% CI: 0.12-0.88) was a protective factor for SCD. RCS analysis showed that there was a positive linear dose-response relationship between fasting plasma glucose (FPG), TG and the risk of SCD (general trend P<0.05, non-linear P>0.05). Conclusions TG, LDL-C, diabetes, abnormal electrocardiogram and education level were related to the occurrence of SCD, and there was a dose-response relationship between FPG, TG and the risk of SCD. -
图 1 FPG、TG、LDL-C与SCD发病风险间的剂量-反应关系
1. FPG: 空腹血糖; TG: 三酰甘油; LDL-C: 低密度脂蛋白胆固醇; OR: 比值比; SCD: 心源性猝死。
2. FPG的参考点为7.00 mmoL/L,TG的参考点为1.70 mmoL/L,LDL-C的参考点为3.40 mmoL/L。调整了吸烟、冠心病、高血压、BMI、文化程度、职业、HDL-C、糖尿病(仅TG和LDL-C调整)、TG (仅FPG和LDL-C调整)、LDL-C (仅PFG和TG调整)和心电图。Figure 1. Dose-response relationship between FPG, TG, LDL-C and the risk of SCD
1. FPG: fasting plasma glucose; TG: triglycerides; LDL-C: low density lipoprotein cholesterol; OR: odds ratio; SCD: sudden cardiac death.
2. The reference point of FPG is 7.00 mmoL/L, the reference point of TG is 1.70 mmoL/L and the reference point of LDL-C is 3.40 mmoL/L. Adjusted for smoking, coronary heart disease, hypertension, BMI, education, occupation, HDL-C, diabetes (adjusted for TG and LDL-C only), TG (adjusted for FPG and LDL-C only), LDL-C (adjusted for PFG and TG only), and electrocardiogram.表 1 研究对象的基线特征
Table 1. Baseline characteristics of study subjects
基线特征
Baseline characteristics新发病例组①
New cases group ①
(n=52)对照组①
Control group ①
(n=208)合计①
Total ①
(n=260)t/χ2/Z值
valueP值
value年龄/岁 Age/years 55.92±15.37 55.87±14.61 55.88±14.73 -0.03 0.980 性别 Sex 0 1.000 男 Male 49(94.23) 196(94.23) 231(88.85) 女 Female 3(5.77) 12(5.77) 29(11.15) 职业 Occupation 3.12 0.413 工人 Worker 38(73.08) 125(60.10) 163(62.69) 干部 Administrator 9(17.31) 55(26.44) 64(24.62) 技术人员 Technical staff 3(5.77) 19(9.13) 22(8.46) 服务人员 Service staff 2(3.84) 9(4.33) 11(4.23) 文化程度 Educational level 10.12 0.038 小学及以下 Primary school and below 12(23.08) 31(14.90) 43(16.54) 初中 Junior school 18(34.61) 47(22.60) 65(25.00) 高中/中专 Senior school/Technical secondary school 9(17.31) 63(30.29) 72(27.69) 大专及以上 Junior college or above 13(25.00) 67(32.21) 80(30.77) 吸烟 Smoking 6.15 0.013 否 No 18(34.62) 112(53.85) 130(50.00) 是 Yes 34(65.38) 96(26.15) 130(50.00) 饮酒 Drinking 0.29 0.593 否 No 34(65.38) 144(69.23) 178(68.46) 是 Yes 18(34.62) 64(30.77) 82(31.54) 饮茶 Drinking tea 1.43 0.232 否 No 18(34.62) 91(43.75) 109(41.92) 是 Yes 34(65.38) 117(56.25) 151(58.08) 心电图 Electrocardiogram 10.49 0.001 正常 Normal 18(34.62) 124(59.62) 142(54.62) 异常 Abnormal 34(65.38) 84(40.38) 118(45.38) 高血压 Hypertension 2.01 0.157 否 No 32(61.54) 149(71.63) 181(69.62) 是 Yes 20(38.46) 59(28.37) 79(30.38) 糖尿病 Diabetes 9.32 0.002 否 No 41(78.85) 195(93.75) 236(90.77) 是 Yes 11(21.15) 13(6.25) 24(9.23) 冠心病 Coronary heart disease 3.26 0.071 否 No 46(88.46) 198(95.19) 244(93.85) 是 Yes 6(11.54) 10(4.81) 16(6.15) 高脂血症Hyperlipemia 0.17 0.682 否 No 42(80.77) 173(83.17) 215(82.69) 是 Yes 10(19.23) 35(16.83) 45(17.31) 高血压家族史 Family history of hypertension 0.17 0.595 否 No 37(71.15) 140(67.31) 177(68.08) 是 Yes 15(28.85) 68(32.69) 83(31.92) 糖尿病家族史 Family history of diabetes 0.93 0.335 否 No 49(94.23) 187(89.90) 236(90.77) 是 Yes 3(5.77) 21(10.10) 24(9.23) 收缩压/mmHg SBP/mmHg 137.83±24.13 131.60±21.76 132.85±22.35 -1.81 0.072 舒张压/mmHg DBP/mmHg 85.19±17.11 82.85±12.82 83.32±13.78 -0.92 0.359 BMI/(kg·m-2) 24.44±3.26 24.75±3.05 24.69±3.09 0.64 0.526 TC/(mmol·L-1) 4.70(4.03, 5.38) 4.60(4.10, 5.20) 4.60(4.10, 5.20) -0.97 0.331 TG/(mmol·L-1) 1.90(1.50, 3.10) 1.60(1.20, 2.20) 1.70(1.22, 2.30) -2.28 0.022 LDL-C/(mmol·L-1) 3.28(2.60, 3.65) 2.89(2.39, 3.51) 2.94(2.43, 3.59) -1.87 0.062 HDL-C/(mmol·L-1) 1.27(1.12, 1.46) 1.23(1.06, 1.41) 1.23(1.06, 1.42) -1.00 0.318 FPG/(mmol·L-1) 5.50(4.90, 6.90) 5.30(4.93, 6.00) 5.30(4.90, 6.18) -1.40 0.161 注:BMI, 体质指数;TC, 总胆固醇;TG, 三酰甘油;LDL-C, 低密度脂蛋白胆固醇;HDL-C, 高密度脂蛋白胆固醇;FPG, 空腹血糖。
①符合正态分布的资料用x±s表示; 不符合正态分布的资料用[M(P25, P75)]表示; 全部分类资料用[人数(构成比/%)]表示。
Note: BMI, body mass index; TC, total cholesterol; TG, triglycerides; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; FPG, fasting plasma glucose.
① Data conforming to the normal distribution is represented by x±s; data not conforming to the normal distribution is represented by [M(P25, P75)]; All categorical data are expressed as [Number of people (proportion/%)].表 2 心源性猝死的基线疾病及行为因素的单因素条件logistic回归分析
Table 2. Univariate conditional logistic regression analysis of baseline disease and behavioral factors of SCD
变量
Variable新发病例组①
New cases group ①
(n=52)对照组①
Control group ①
(n=208)Wald χ2值
valueOR值 value
(95% CI)P值
value文化程度 Educational level 初中及以下 Junior high school and below 30(57.69) 78(37.50) 1.00 高中及以上 High school and above 22(42.31) 130(62.50) 7.49 0.39(0.20~0.77) 0.006 职业 Occupation 工人 Worker 38(73.08) 125(60.10) 3.61 1.00 0.307 干部 Administrator 9(17.31) 55(26.44) 2.88 0.49(0.21~1.12) 0.090 技术人员 Technical staff 3(5.77) 19(9.13) 1.38 0.46(0.12~1.69) 0.240 服务人员 Service staff 2(3.84) 9(4.33) 0.07 0.81(0.16~4.01) 0.790 吸烟 Smoking 否 No 18(34.62) 112(53.85) 1.00 是 Yes 34(65.38) 96(26.15) 6.49 2.40(1.22~4.70) 0.011 饮酒 Drinking 否 No 34(65.38) 144(69.23) 1.00 是 Yes 18(34.62) 64(30.77) 0.29 1.19(0.62~2.27) 0.593 饮茶 Drinking tea 否 No 18(34.62) 91(43.75) 1.00 是 Yes 34(65.38) 117(56.25) 1.53 1.52(0.78~2.95) 0.216 高血压 Hypertension 否 No 32(61.54) 149(71.63) 1.00 是 Yes 20(38.46) 59(28.37) 2.13 1.64(0.85~3.16) 0.144 糖尿病 Diabetes 否 No 41(78.85) 195(93.75) 1.00 是 Yes 11(21.15) 13(6.25) 9.45 4.08(1.66~9.99) 0.002 冠心病 Coronary heart disease 否 No 46(88.46) 198(95.19) 1.00 是 Yes 6(11.54) 10(4.81) 3.36 2.99(0.93~9.66) 0.067 高脂血症 Hyperlipemia 否 No 42(80.77) 173(83.17) 1.00 是 Yes 10(19.23) 35(16.83) 0.17 1.18(0.54~2.59) 0.679 高血压家族史 Family history of hypertension 否 No 37(71.15) 140(67.31) 1.00 是 Yes 15(28.85) 68(32.69) 0.28 0.84(0.43~1.63) 0.597 糖尿病家族史 Family history of diabetes 否 No 49(94.23) 187(89.90) 1.00 是 Yes 3(5.77) 21(10.10) 0.88 0.55(0.16~1.91) 0.349 注:①采用[人数(构成比/%)]表示。
Note: ①[Number of people (proportion/%)].表 3 SCD基线生理生化指标的单因素条件logistic回归分析
Table 3. Univariate conditional logistic regression analysis of baseline physiological and biochemical indexes of SCD
变量 Variable 新发病例组①
New cases group ①
(n=52)对照组①
Control group ①
(n=208)Wald χ2值
valueOR值 value
(95% CI)P值
value收缩压/mmHg SBP/mmHg 正常 Normal 33(63.46) 151(72.60) 1.00 异常 Abnormal 19(36.54) 57(27.40) 1.86 1.61(0.81~3.21) 0.173 舒张压/mmHg DBP/mmHg 正常 Normal 34(65.38) 150(72.12) 1.00 异常 Abnormal 18(34.62) 58(27.88) 0.90 1.37(0.72~2.61) 0.342 心电图 Electrocardiogram 正常 Normal 18(34.62) 124(59.62) 1.00 异常 Abnormal 34(65.38) 84(40.38) 10.50 3.06(1.56~6.01) 0.001 TC/(mmol·L-1) 正常 Normal 37(71.15) 150(72.12) 1.00 异常 Abnormal 15(28.85) 58(27.88) 0.02 1.05(0.54~2.05) 0.890 TG/(mmol·L-1) 正常 Normal 17(32.69) 109(52.40) 1.00 异常 Abnormal 35(67.31) 99(47.60) 6.69 2.39(1.24~4.61) 0.010 LDL-C/(mmol·L-1) 正常 Normal 26(50.00) 144(69.23) 1.00 异常 Abnormal 26(50.00) 64(30.77) 6.42 2.21(1.20~4.08) 0.011 HDL-C/(mmol·L-1) 正常 Normal 43(82.69) 171(82.21) 1.00 异常 Abnormal 9(17.31) 37(17.79) 0.01 0.96(0.41~2.27) 0.931 BMI/(kg·m-2) <24.0 19(36.54) 85(40.86) 2.07 1.00 24.0~<28.0 27(51.92) 87(41.83) 1.01 1.41(0.72~2.75) 0.315 ≥28.0 6(11.54) 36(17.31) 0.33 0.75(0.28~2.02) 0.570 注:SCD, 心源性猝死;TC: 总胆固醇;TG: 三酰甘油;LDL-C: 低密度脂蛋白胆固醇;HDL-C: 高密度脂蛋白胆固醇;BMI: 体质指数。
①采用[例数(构成比/%)]表示。
Note: SCD, sudden cardiac death; TC, total cholesterol; TG, triglycerides; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; BMI: body mass index.
①[Number of people (proportion/%)].表 4 心源性猝死的多因素条件logistic回归分析
Table 4. Multivariate conditional logistic regression analysis of SCD
变量 Variable β sx Wald χ2值 value OR值 value
(95% CI)P值 value TG/(mmol·L-1) 正常 Normal 1.00 异常 Abnormal 1.08 0.48 5.11 2.94(1.15~7.51) 0.024 LDL-C/(mmol·L-1) 正常 Normal 1.00 异常 Abnormal 0.99 0.43 5.47 2.70(1.18~6.22) 0.019 HDL-C/(mmol·L-1) 正常 Normal 1.00 异常 Abnormal 0.44 0.61 0.51 1.55(0.47~5.15) 0.474 BMI/(kg·m-2) <24.0 4.92 1.00 0.085 24.0~<28.0 0.51 0.44 1.39 1.67(0.71~3.92) 0.238 ≥28.0 -0.83 0.62 1.78 0.43(0.13~1.48) 0.182 心电图 Electrocardiogram 正常 Normal 1.00 异常 Abnormal 1.71 0.49 12.07 5.54(2.11~14.56) 0.001 糖尿病 Diabetes 否 No 1.00 是 Yes 1.72 0.58 8.76 5.59(1.79~17.46) 0.003 冠心病 Coronary heart disease 否 No 1.00 是 Yes 1.22 0.85 2.07 3.39(0.64~17.86) 0.150 高血压 Hypertension 否 No 1.00 是 Yes -0.30 0.47 0.41 0.74(0.30~1.85) 0.523 吸烟 Smoking 否 No 1.00 是 Yes 0.50 0.44 1.32 1.65(0.70~3.87) 0.251 文化程度 Educational level 初中及以下 Junior high school and below 1.00 高中及以上 High school and above -0.11 0.50 4.90 0.33(0.12~0.88) 0.027 职业 Occupation 工人 Worker 0.70 1.00 0.873 干部 Administrator -0.40 0.60 0.43 0.67(0.21~2.19) 0.511 技术人员 Technical staff -0.66 0.89 0.55 0.52(0.09~2.94) 0.456 服务人员 Service staff 0.06 0.94 0 1.06(0.17~6.70) 0.951 注:SCD, 心源性猝死;TG, 三酰甘油;LDL-C, 低密度脂蛋白胆固醇;HDL-C, 高密度脂蛋白胆固醇;BMI: 体质指数。
Note: SCD, sudden cardiac death; TG, triglycerides; LDL-C, low Density Lipoprotein Cholesterol; HDL-C, high density lipoprotein cholesterol; BMI, body mass index. -
[1] 范国辉, 张林峰. 心源性猝死的流行病学研究进展[J]. 中华流行病学杂志, 2015, 36(1): 87-89. DOI: 10.3760/cma.j.issn.0254-6450.2015.01.020.Fan GH, Zhang LF. The epidemiological research progress of sudden cardiac death[J]. Chin J Epidemiol, 2015, 36(1): 87-89. DOI: 10.3760/cma.j.issn.0254-6450.2015.01.020. [2] 张道琴, 杨呈伟, 彭明亮, 等. 心源性猝死防治的最新研究进展[J]. 中国医药, 2020, 15(11): 1799-1803. DOI: 10.3760/j.issn.1673-4777.2020.11.034.Zhang DQ, Yang CW, Peng ML, et al. The latest research progress in the prevention and treatment of sudden cardiac death[J]. China Medicine, 2020, 15(11): 1799-1803. DOI: 10.3760/j.issn.1673-4777.2020.11.034. [3] Primorac D, Odak L, Perić V, et al. Sudden Cardiac Death-A New Insight Into Potentially Fatal Genetic Markers. [J]. Front Med (Lausanne), 2021, 8: 647412. DOI: 10.3389/fmed.2021.647412. [4] Shen CX, Ge JB. Epidemic of cardiovascular disease in China: Current perspective and prospects for the future[J]. Circulation, 2018, 138(4): 342-344. DOI: 10.1161/circulationaha.118.033484. [5] Wong CX, Brown A, Lau DH, et al. Epidemiology of sudden cardiac death: global and regional perspectives[J]. Heart Lung and Circu, 2019, 28(1): 6-14. DOI: 10.1016/j.hlc.2018.08.026. [6] Semsarian C, Ingles J, Wilde AAM. Sudden cardiac death in the young: the molecular autopsy and a practical approach to surviving relatives[J]. Eur Heart J, 2015, 36(21): 1290-1296. DOI: 10.1093/eurheartj/ehv063. [7] Albert CM, Chae CU, Grodstein F, et al. Prospective study of sudden cardiac death among women in the United States[J]. Circulation, 2003, 107(16): 2096-2101. DOI: 10.1161/01.CIR.0000065223.21530.11. [8] Bai YN, Yang AM, Pu HQ, et al. Cohort profile: the China metal-exposed workers cohort study (Jinchang cohort)[J]. Int J Epidemiol, 2017, 46(4): 1095-1096e. DOI: 10.1093/ije/dyw223. [9] 刘力生. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019, 24(1): 24-56. DOI: 10.3969/j.issn.1007-5410.2019.01.002.Liu LS. Chinese guidelines for the prevention and treatment of hypertension (2018 Revised Edition)[J]. Chin J Cardiovasc Med, 2019, 24(1): 24-56. DOI: 10.3969/j.issn.1007-5410.2019.01.002. [10] 诸骏仁, 高润霖, 赵水平, 等. 中国成人血脂异常防治指南(2016年修订版)[J]. 中华心血管病杂志, 2016, 31(10): 833-853. DOI: 10.3969/j.issn.1000-3614.2016.10.001.Zhu JR, Gao RL, Zhao SP, et al. Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (2016 revised edition)[J]. Chin J Cardiol, 2016, 31(10): 833-853. DOI: 10.3969/j.issn.1000-3614.2016.10.001. [11] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2017年版)[J]. 中国实用内科杂志, 2018, 38(4): 299-344. DOI: 10.19538/j.nk201804010.Chinese Diabetes Society. Guidelines for the prevention and control of type 2 diabetes in China (2017 Edition)[J]. Chinese Journal of Practical Internal Medicine, 2018, 38(4): 299-344. DOI: 10.19538/j.nk201804010. [12] 中国肥胖问题工作组. 中国成人超重和肥胖症预防与控制指南(节录)[J]. 营养学报, 2004, 26(1): 1-4. DOI: 10.13325/j.cnki.acta.nutr.sin.2004.01.001.Working Group on Obesity in China. Guidelines for the prevention and control of overweight and obesity in Chinese adults (excerpt)[J]. Acta Nutrim Sin, 2004, 26(1): 1-4. DOI: 10.13325/j.cnki.acta.nutr.sin.2004.01.001. [13] Lee S, Jeevaratnam K, Liu T, et al. Prediction of atrial fibrillation and sudden cardiac death in type 2 diabetic patients on insulin: a territory-wide observational cohort study[J]. Eur Heart J Acute CA, 2021, 10(Supplement_1): zuab020-019. DOI: 10.1093/EHJACC/ZUAB020.019. [14] Nakajima K, Nakajima Y, Takeichi S, et al. Plasma remnant-like lipoprotein particles or LDL-C as major pathologic factors in sudden cardiac death cases[J]. Atherosclerosis, 2008, 198(1): 237-246. DOI: 10.1016/j.atherosclerosis.2007.09.016. [15] Kunutsor SK, Zaccardi F, Karppi J, et al. Is high serum LDL/HDL cholesterol ratio an emerging risk factor for sudden cardiac death? findings from the KIHD study[J]. J Atheroscler Thromb, 2017, 24(6): 600-608. DOI: 10.5551/jat.37184. [16] Al-Aubaidy HA, Jelinek HF. Oxidative stress and triglycerides as predictors of subclinical atherosclerosis in prediabetes[J]. Redox Rep, 2014, 19(2): 87-91. DOI: 10.1179/1351000213Y.0000000080. [17] Eranti A, Kerola T, Aro AL, et al. Diabetes, glucose tolerance, and the risk of sudden cardiac death[J]. BMC cardiovas disord, 2016, 16(1): 1-8. DOI: 10.1186/s12872-016-0231-5. [18] Walker AM, Cubbon RM. Sudden cardiac death in patients with diabetes mellitus and chronic heart failure[J]. Diab Vasc Dis Res, 2015, 12(4): 228-233. DOI: 10.1177/1479164115573225. [19] Svane JS, Pedersen-Bjergaard U, Tfelt-Hansen J. Diabetes and the risk of sudden cardiac death[J]. Curr Cardiol Rep, 2020, 22(10): 1-10. DOI: 10.1007/s11886-020-01366-2. [20] Kenttä TV, Nearing BD, Porthan K, et al. Prediction of sudden cardiac death with automated high-throughput analysis of heterogeneity in standard resting 12-lead electrocardiograms[J]. Heart Rhythm, 2016, 13(3): 713-720. DOI: 10.1016/j.hrthm.2015.11.035. [21] Holkeri A, Eranti A, Haukilahti MAE, et al. Predicting sudden cardiac death in a general population using an electrocardiographic risk score[J]. Heart, 2020, 106(6): 427-433. DOI: 10.1136/heartjnl-2019-315437. -





 下载:
下载: