Development and validation of a risk prediction model for venous thromboembolism in stroke patients
-
摘要:
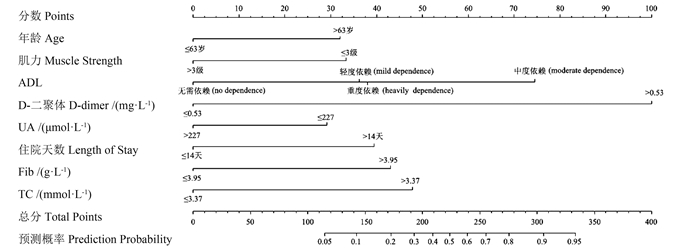
目的 构建并验证脑卒中患者发生静脉血栓栓塞症(venous thromboembolism, VTE)的风险预测模型,为脑卒中患者VTE的预防控制提供科学依据。 方法 研究对象为河南省脑卒中队列的675例脑卒中患者,按7∶3随机划分为训练集(473例)和测试集(202例)。使用随机森林算法筛选变量、logistic回归模型分析方法构建模型,并绘制列线图。通过受试者工作特征曲线下面积(area under curve, AUC)、Hosmer-Lemeshow检验等评价模型的预测效能,使用决策曲线分析(decision curve analysis, DCA)评估模型的临床使用价值;并采用五折交叉验证对模型进行内部验证。 结果 最终纳入模型的预测因子为年龄、住院天数、日常生活活动能力(activity of daily living, ADL)、肌力、尿酸(uric acid, UA)、D-二聚体、纤维蛋白原(fibrinogen, Fib)和总胆固醇(total cholesterol, TC)。模型在训练集中的Hosmer-Lemeshow检验P=0.872,AUC=0.924(95% CI: 0.898~0.950);测试集Hosmer-Lemeshow检验P=0.597,AUC=0.902(95% CI: 0.852~0.951)。DCA曲线表明,模型在训练集和测试集中均具有较高的临床净获益。五折交叉内部验证结果显示,模型在训练集和测试集中的平均AUC分别为0.913和0.929。 结论 该研究构建的脑卒中患者VTE风险预测模型能有效预测VTE的发生,可为高风险患者早期识别和预防性治疗提供参考。 Abstract:Objective To develop and validate the risk prediction model of venous thromboembolism (VTE) in stroke patients, so as to provide a scientific basis for the prevention and control of VTE. Methods A total of 675 stroke patients were enrolled from our stroke cohort of Henan Province. The data were randomly divided into a training (473 patients) and a testing dataset (202 patients) by a ratio of 7∶3. Then, we used a random forest algorithm for variable selection and logistic regression analysis to construct the model, and a nomogram was drawn. The prediction efficiency of the model was evaluated by the area under the receiver operating characteristic curve and Hosmer-Lemeshow test. Decision curve analysis (DCA) was used to evaluate the clinical application value of the model and the five-fold cross-validation was utilized to verify the model internally. Results The predictors that ultimately entered the prediction model were age, hospital stays, ADL, myodynamia, uric acid, D-dimer, fibrinogen, and total cholesterol. In the training dataset, the Hosmer-Lemeshow test yielded P=0.872 and the AUC was 0.924 (95% CI: 0.898-0.950). The testing dataset showed that the Hosmer-Lemeshow test yielded P=0.597 and the AUC was 0.902 (95% CI: 0.852-0.951). DCA curves indicated that the model had high clinical net benefits in both datasets. Internal verification presented that the average AUCs of the model in the training and testing datasets were 0.913 and 0.929, respectively. Conclusions The risk prediction model developed in this study can effectively predict VTE occurrence in stroke patients, offering a valuable tool for identifying high-risk individuals and implementing early preventive measures. -
Key words:
- Stroke /
- Venous thromboembolism /
- Prediction model /
- Random forest /
- Nomogram
-
表 1 训练集与测试集病例的基线特征
Table 1. Baseline characteristics of patients in training and testing datasets
变量 Variable 训练集 Training datasets (n=473) 测试集 Testing datasets (n=202) VTE组①
VTE group ①
(n=121, 25.6%)非VTE组①
Non-VTE group ①
(n=352, 74.4%)Z/χ2值
valueP值
valueVTE组①
VTE group ①
(n=43, 21.3%)非VTE组①
Non-VTE group ①
(n=159, 78.7%)Z/χ2值
valueP值
value性别 Gender 8.476 0.004 2.709 0.100 男性 Man 61(21.0) 230(79.0) 24(17.9) 110(82.1) 女性 Woman 60(33.0) 122(67.0) 19(27.9) 49(72.1) 年龄/岁 Age/years 68(57, 74) 58(50, 68) -5.033 < 0.001 67(57, 75) 58(48, 68) -3.596 < 0.001 住院天数/d Length of stay/d 17(10, 25) 10(8, 15) -6.805 < 0.001 15(10, 21) 10(7, 13) -4.207 < 0.001 BMI/(kg·m-2) 3.875 0.268 2.256 0.500 <18.5 4(50.0) 4(50.0) 1(33.3) 2(66.7) 18.5~<24.0 52(27.1) 140(72.9) 19(25.7) 55(74.3) 24.0~<28.0 56(24.9) 169(75.1) 18(19.4) 75(80.6) ≥28.0 9(18.8) 39(81.2) 5(15.6) 27(84.4) ADL 71.515 < 0.001 20.336 < 0.001 无须依赖 No dependence 2(2.2) 87(97.8) 3(6.5) 43(93.5) 轻度依赖 Mild dependence 26(15.4) 143(84.6) 9(13.2) 59(86.8) 中度依赖 Moderate dependence 35(38.9) 55(61.1) 9(28.1) 23(71.9) 重度依赖 Heavily dependence 58(46.4) 67(53.6) 22(39.3) 34(60.7) 卒中类型 Stroke subtypes 10.582 0.004 14.255 < 0.001 缺血性 Ischemic 93(23.1) 310(76.9) 31(17.5) 146(82.5) 出血性 Hemorrhagic 23(37.1) 39(62.9) 9(40.9) 13(59.1) 混合型 Mixed 5(62.5) 3(37.5) 3(100.0) 0(0.0) 吸烟史 Smoking history 4.543 0.103 0.850 0.714 从不吸烟 Never smoking 95(28.3) 241(71.7) 31(22.5) 107(77.5) 曾经吸烟 Ever smoking 9(20.9) 34(79.1) 5(23.8) 16(76.2) 现在吸烟 Current smoking 17(18.1) 77(81.9) 7(16.3) 36(83.7) 饮酒史 Drinking history 6.072 0.048 1.406 0.504 从不饮酒 Never drinking 99(28.4) 249(71.6) 34(23.4) 111(76.6) 曾经饮酒 Ever drinking 6(22.2) 21(77.8) 1(9.1) 10(90.9) 现在饮酒 Current drinking 16(16.3) 82(83.7) 8(17.4) 38(82.6) 输血史 Transfusion history 17(41.5) 24(58.5) 5.948 0.015 9(45.0) 11(55.0) 5.961 0.015 卒中史 Stroke history 34(26.4) 95(73.6) 0.056 0.813 25(34.2) 48(65.8) 11.458 0.001 并发症 Complications 糖尿病 Diabetes 36(23.7) 116(76.3) 0.423 0.515 16(23.9) 51(76.1) 0.402 0.526 高血压 Hypertension 93(26.8) 254(73.2) 1.018 0.313 30(21.7) 108(78.3) 0.053 0.818 高脂血症 Hyperlipidaemia 14(26.4) 39(73.6) 0.022 0.883 3(15.0) 17(85.0) 0.190 0.663 房颤 Atrial fibrillation 17(60.7) 11(39.3) 19.297 < 0.001 6(75.0) 2(25.0) 11.199 0.001 感染 Infection 65(51.6) 61(48.4) 61.016 < 0.001 21(48.8) 22(51.2) 24.746 < 0.001 恶性肿瘤 Malignant tumor 8(80.0) 2(20.0) 13.106 < 0.001 4(100.0) 0(0.0) 10.677 < 0.001 脱水类药物 Hyperosmotic drugs 56(48.3) 60(51.7) 41.580 < 0.001 17(39.5) 26(60.5) 10.856 0.001 抗血小板药物 Antiplatelet drugs 85(23.1) 283(76.9) 5.371 0.020 29(17.9) 133(82.1) 5.597 0.018 激素类药物 Hormone drugs 6(50.0) 6(50.0) 2.653 0.103 3(42.9) 4(57.1) 0.901 0.343 溶栓 Thrombolysis 17(51.5) 16(48.5) 12.533 < 0.001 4(25.0) 12(75.0) 0.004 0.952 深静脉置管 Deep vein catheterization 31.648 < 0.001 14.289 < 0.001 无 No 96(22.2) 337(77.8) 33(17.8) 152(82.2) 中心静脉 Central venous 22(61.1) 14(38.9) 9(64.3) 5(35.7) 股静脉 Femoral vein 3(75.0) 1(25.0) 1(33.3) 2(66.7) PT/s 10.9(10.2~12.0) 10.5(9.9~11.1) -3.961 < 0.001 11.1(10.4~12.2) 10.6(10.0~11.0) -2.747 0.006 PTA/% 102.0(91.7~113.5) 108.0(99.3~116.8) -3.746 < 0.001 100.0(87.0~112.0) 106.0(99.0~116.0) -2.516 0.012 APTT/s 27.6(24.7~29.7) 28.7(26.3~31.1) -2.988 0.003 27.6(24.5~32.1) 28.9(26.7~31.4) -1.179 0.238 Fib/(g·L-1) 3.67(2.95~4.61) 2.93(2.55~3.44) -6.623 < 0.001 3.83(2.78~4.53) 2.88(2.45~3.39) -3.898 < 0.001 TT/s 15.3(14.0~16.8) 15.3(14.3~16.9) -0.780 0.435 15.1(13.7~16.7) 15.7(14.4~17.1) -1.775 0.076 D-二聚体/(mg·L-1) D-dimer/(mg·L-1) 1.02(0.37~3.06) 0.15(0.08~0.27) -11.546 < 0.001 0.83(0.29~2.11) 0.16(0.08~0.24) -6.685 < 0.001 CRP/(mg·L-1) 17.25(2.98~69.12) 2.42(1.01~7.71) -7.203 < 0.001 20.28(5.01~102.95) 2.94(1.29~7.48) -5.458 < 0.001 血红蛋白/(g·L-1) Hemoglobin/(g·L-1) 128.8(115.9~139.7) 137.0(125.8~147.0) -4.347 < 0.001 125.0(117.2~144.0) 140.3(126.9~149.0) -2.592 0.010 PLT/(109·L-1) 223.0(180.5~272.5) 215.5(179.3~258.8) -0.947 0.344 223.0(169.0~273.0) 217.0(186.0~251.0) -0.109 0.913 UA/(μmol·L-1) 222(182~288) 273(222~335) -4.992 < 0.001 252(208~328) 274(227~336) -0.953 0.913 TC/(mmol·L-1) 3.88(3.23~4.64) 3.71(3.06~4.47) -2.084 0.037 3.81(3.09~4.57) 3.83(3.25~4.76) -0.260 0.795 TG/(mmol·L-1) 1.26(0.93~1.95) 1.21(0.87~1.62) -1.407 0.159 1.32(0.95~1.61) 1.31(0.99~1.84) -0.838 0.402 LDL/HDL 2.26(1.73~2.77) 2.09(1.51~2.73) -1.421 0.155 2.38(1.76~3.29) 2.28(1.72~2.95) -0.644 0.520 Hcy/(μmol·L-1) 13.57(10.87~17.64) 14.11(11.11~17.92) -0.684 0.494 13.22(10.35~16.57) 14.38(12.61~19.61) -2.145 0.032 GCS 15(9~15) 15(15~15) -7.608 < 0.001 15(9~15) 15(15~15) -4.559 < 0.001 肌力/级 Muscle strength/grade 3(2~4) 5(4~5) -8.527 < 0.001 3.8(2~5) 5(4~5) -3.232 0.001 NIHSS评分 NIHSS score 5(3~8) 3(2~6) -4.937 < 0.001 4(2~10) 3(1~5) -2.978 0.003 mRs评分 mRs score 0(0~2) 0(0~1) -2.370 0.018 1(0~2) 0(0~1) -1.233 0.217 吞咽功能/级 Swallowing function/grade 1(1~2) 1(1~1) -4.282 < 0.001 1(1~2) 1(1~1) -2.651 0.008 注:PT, 凝血酶原时间; PTA, 凝血酶原时间活动度; APTT, 活化部分凝血酶原时间; TT, 凝血酶时间; CRP, C-反应蛋白; PLT, 血小板计数; UA, 尿酸; TC, 总胆固醇; TG, 甘油三酯; LDL/HDL, 低密度脂蛋白/高密度脂蛋白; Hcy, 同型半胱氨酸; NIHSS, 美国国立卫生院神经功能缺损。
①以[人数(占比/%)]或[M(P25, P75)]表示。
Note: PT, prothrombin time; PTA, prothrombin time activity; APTT, activated partial thromboplastin time; TT, thrombin time; CRP, C-reactive protein; PLT, blood platelet count; UA, uric acid; TC, total cholesterol; TG, triglyceride; LDL/HDL, low density lipoprotein/high-density lipoprotein; Hcy, homocysteine; NIHSS, national institution of health stroke scale.
① [Number of people (proportion/%)] or [M(P25, P75)].表 2 脑卒中患者VTE的多因素logistic回归模型分析
Table 2. Multivariate logistic regression model analysis of the risk of VTE in stroke patients
变量 Variable β s Wald值
valueOR值 value
(95% CI)P值
value常量 Constant -3.730 1.077 -3.463 0.024(0.002~0.174) 0.001 年龄>63岁 Age >63 years 0.858 0.336 2.554 2.359(1.227~4.609) 0.011 ADL(参照:无须依赖) ADL(reference: no dependence) 轻度依赖 Mild dependence 0.907 0.822 1.103 2.476(0.591~17.234) 0.270 中度依赖 Moderate dependence 1.909 0.837 2.281 6.745(1.559~47.997) 0.023 重度依赖 Heavily dependence 0.321 0.915 0.351 1.378(0.260~10.854) 0.726 住院天数>14 d length of stay >14 days 1.015 0.336 3.019 2.761(1.432~5.383) 0.003 肌力>3级 Muscle strength >3 grades -0.890 0.370 -2.403 0.411(0.197~0.846) 0.016 D-二聚体>0.53/(mg·L-1) D-dimer >0.53/(mg·L-1) 2.521 0.363 6.945 12.435(6.208~25.896) <0.001 Fib>3.95/(g·L-1) 1.054 0.402 2.620 2.869(1.305~6.355) 0.009 UA>227/(μmol·L-1) -0.811 0.329 -2.463 0.445(0.231~0.845) 0.014 TC>3.37/(mmol·L-1) 1.333 0.385 3.460 3.793(1.831~8.344) 0.001 注:VTE, 静脉血栓栓塞症; ADL, 日常行为活动能力; Fib, 纤维蛋白原; UA, 尿酸; TC, 总胆固醇。
Note: VTE, venous thromboembolism; ADL, activity of daily living; Fib, fibrinogen; UA, uric acid; TC, total cholesterol. -
[1] 王深明. 静脉血栓栓塞症诊治现状与展望[J]. 中国实用外科杂志, 2010, 30(12): 992-994. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK201012004.htmWang SM. The present situation and forecast of venous thromboembolism[J]. Chin J Pract Surg, 2010, 30(12): 992-994. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK201012004.htm [2] Liu XC, Chen XW, Li ZL, et al. Anatomical distribution of lower-extremity deep venous thrombosis in patients with acute stroke[J]. J Stroke Cerebrovasc Dis, 2020, 29(7): 104866. DOI: 10.1016/j.jstrokecerebrovasdis.2020.104866. [3] Khan F, Tritschler T, Kahn SR, et al. Venous thromboembolism[J]. Lancet, 2021, 398(10294): 64-77. DOI: 10.1016/S0140-6736(20)32658-1. [4] Ding DL, Sekar P, Moomaw CJ, et al. Venous thromboembolism in patients with spontaneous intracerebral hemorrhage: a multicenter study[J]. Neurosurgery, 2018, 84(6): E304-E310. DOI: 10.1093/neuros/nyy333. [5] Kahn SR, Morrison DR, Diendere G, et al. Interventions for implementation of thromboprophylaxis in hospitalized patients at risk for venous thromboembolism[J]. Cochrane Database Syst Rev, 2018, 4(4): D8201. DOI: 10.1002/14651858.CD008201.pub3. [6] 谢长清. 脑卒中急性期并发深静脉血栓形成不同风险评估工具的比较研究[D]. 苏州: 苏州大学, 2020.Xie CQ. A comparative study of different risk assessment tools for acute stroke complicated with deep vein thrombosis[D]. Suzhou: Suzhou university, 2020. [7] Yang YQ, Wang X, Huang Y, et al. Ontology-based venous thromboembolism risk assessment model developing from medical records[J]. BMC Med Inform Decis Mak, 2019, 19(Suppl 4): 151. DOI: 10.1186/s12911-019-0856-2. [8] Pan X, Wang Z, Chen QM, et al. Development and validation of a nomogram for lower extremity deep venous thrombosis in patients after acute stroke[J]. J Stroke Cerebrovasc Dis, 2021, 30(5): 105683. DOI: 10.1016/j.jstrokecerebrovasdis.2021.105683. [9] 陈新宇, 周军良, 李婷婷, 等. 基于随机森林算法和Logistic回归分析的老年肌肉衰减症影响因素[J]. 中华疾病控制杂志, 2022, 26(3): 357-361. DOI: 10.16462/j.cnki.zhjbkz.2022.03.020.Chen XY, Zhou JL, Li TT, et al. Influential factors of sarcopenia in older adults based on random forest and Logistic regression[J]. Chin J Dis Control Prev, 2022, 26(3): 357-361. DOI: 10.16462/j.cnki.zhjbkz.2022.03.020. [10] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国各类主要脑血管病诊断要点2019[J]. 中华神经科杂志, 2019, 52(9): 710-715. DOI: 10.3760/cma.j.issn.1006-7876.2019.09.003.Chinese Society of Neurology; Chinese Stroke Society. Main diagnostic points of cerebro-vascular diseases in China 2019[J]. Chin J Neurol, 2019, 52(9): 710-715. DOI: 10.3760/cma.j.issn.1006-7876.2019.09.003. [11] Wang Y, Shi Y, Dong Y, et al. Clinical risk factors of asymptomatic deep venous thrombosis in patients with acute stroke[J]. Clin Appl Thromb Hemost, 2019, 25: 1076029619868534. DOI: 10.1177/1076029619868534. [12] Cheng HR, Huang GQ, Wu ZQ, et al. Individualized predictions of early isolated distal deep vein thrombosis in patients with acute ischemic stroke: a retrospective study[J]. BMC Geriatr, 2021, 21(1): 140. DOI: 10.1186/s12877-021-02088-y. [13] Riley RD, Ensor J, Snell KIE, et al. Calculating the sample size required for developing a clinical prediction model[J]. BMJ, 2020, 368: m441. DOI: 10.1136/bmj.m441. [14] 张丹丹, 丁唱, 欧阳朝威, 等. 重型创伤性脑损伤患者发生静脉血栓栓塞的危险因素分析[J]. 中华创伤杂志, 2022, 38(4): 346-353. DOI: 10.3760/cma.j.cn501098-20211202-00631.Zhang DD, Ding C, Ou Yang CW, et al. Risk factors of venous thromboembolism in patients with severe traumatic brain injury[J]. Chin J Trauma, 2022, 38(4): 346-353. DOI: 10.3760/cma.j.cn501098-20211202-00631. [15] Spasić I, Ubavić M, Sumarac Z, et al. Influence of lipid metabolism disorders on venous thrombosis risk[J]. J Med Biochem, 2021, 40(3): 245-251. DOI: 10.5937/jomb0-27106. [16] Ren WW, Huang QQ, Fan KL, et al. Uric acid played a role in the association between gender and deep vein thrombosis in patients with stroke[J]. Nutr Metab Cardiovasc Dis, 2021, 31(9): 2700-2706. DOI: 10.1016/j.numecd.2021.05.032. [17] Vila E, Sole M, Masip N, et al. Uric acid treatment after stroke modulates the Kruppel-like factor 2-VEGF-A axis to protect brain endothelial cell functions: Impact of hypertension[J]. Biochem Pharmacol, 2019, 164: 115-128. DOI: 10.1016/j.bcp.2019.04.002. -





 下载:
下载: