Influential factors of mild cognitive impairment in type 2 diabetes mellitus based on machine learning and logistic regression
-
摘要:
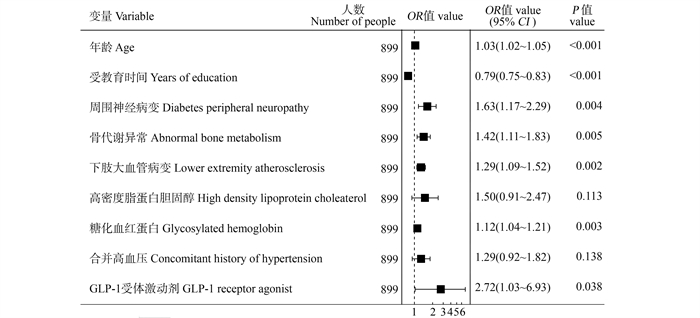
目的 应用机器学习和logistic回归分析模型分析2型糖尿病(type 2 diabetes mellitus, T2DM)轻度认知功能障碍的影响因素,为相关干预措施提供依据。 方法 收集南京鼓楼医院内分泌科1 284例T2DM患者的资料,将数据分为训练集(70%)和测试集(30%),分别采用logistic回归分析、随机森林、XGBoost模型对数据建模并进行可解释性分析。 结果 随机森林模型的预测性能最高,训练集的AUC值为1.0,测试集的AUC值为0.783(95% CI:0.660~0.894),模型筛选出T2DM患者发生轻度认知功能障碍的19个重要变量,如受教育时间、年龄、胰岛素敏感指数、周围神经病变、糖化血红蛋白、骨代谢异常等。 结论 随机森林模型的预测性能最佳,可以协助医务人员准确识别T2DM患者发生轻度认知功能障碍的危险因素,有助于医务人员对患者进行早期预防。 Abstract:Objective To analyze the risk factors of mild cognitive impairment in type 2 diabetes mellitus(T2DM) by using machine learning and Logistic regression, and to provide basis for relevant intervention. Methods The data of 1 284 T2DM patients in the Department of Endocrinology of Nanjing Gulou Hospital were collected. The data were divided into the training set (70%) and the testing set (30%). Logistic regression model, Random Forest and XGBoost were used to construct the models, and the results were explained by the model interpretability. Results The random forest model had the highest predictive performance, the AUC value of the training set was 1.0 while the testing one was 0.783 (95% CI: 0.660-0.894), the model screened 19 important variables for MCI in patients with T2DM, such as education time, age, insulin sensitivity index, peripheral neuropathy, glycosylated hemoglobin, abnormal bone metabolism. Conclusions The prediction performance of random forest model is the best, which can help medical staff accurately identify the risk factors of MCI in patients with T2DM, and help medical staff to apply early intervention. -
表 1 两组患者疾病资料的比较
Table 1. Comparison of disease data between two groups of patients
变量variable 正常对照组 ②
Control group②
(n=865)MCI组 ②
group ②
(n= 419)t/Z/χ2
值valueP值
value病程/年Course of disease /years 9.56±8.01 10.81±8.28 -2.56 0.010 年龄/年Age/years 55.34±11.70 61.91±8.60 -11.36 < 0.001 性别Gender 16.60 < 0.001 男Male 605(69.94) 245(58.47) 女Female 260(30.06) 174(41.53) 受教育时间/年Years of education/years 12.97±3.24 10.41±3.35 13.15 < 0.001 糖尿病家族史Family history of diabetes 467(53.99) 191(45.58) 7.65 0.006 合并高血压Concomitant history of hypertension 407(47.05) 244(58.23) 14.12 < 0.001 合并高血脂Concomitant history of hyperlipidemia 357(41.27) 147(35.08) 4.28 0.039 体质指数/(kg·m-2) Body mass index/(kg·m-2) 24.84(23.03, 27.12) 24.14(22.23, 26.46) -3.54 < 0.001 周围神经病变Diabetes peripheral neuropathy 235(27.17) 180(42.96) 31.46 < 0.001 颈动脉斑块Complications of carotid artery plaques 471(54.45) 296(70.64) 30.11 < 0.001 糖尿病肾病Complications of diabetic nephropathy 83(9.59) 58(13.84) 4.78 0.029 骨代谢异常Abnormal bone metabolism 303(35.03) 217(51.79) -20.94 < 0.001 下肢大血管病变Lower extremity atherosclerosis 408(47.17) 260(62.05) 24.46 < 0.001 脑血管病史History of cerebrovascular diseases 83(9.60) 74(17.66) 16.37 < 0.001 心血管病史History of cardiovascular 107(12.37) 85(20.29) 13.30 < 0.001 使用GLP-1药物 ① Using GLP-1 medication ① 23(2.66) 13(3.10) 0.65 0.786 三酰甘油/(mmol·L-1) Triglyceride/(mmol·L-1) 1.35(0.95, 2.06) 1.30(0.90, 1.83) -1.78 0.075 胆固醇/(mmol·L-1) Cholesterol/(mmol·L-1) 4.53(3.79, 5.34) 4.45(3.70, 5.27) -1.21 0.225 低密度脂蛋白胆固醇/(mmol·L-1) Low density lipoprotein cholesterol/(mmol·L-1) 2.64(2.00, 3.30) 2.99(2.32, 3.66) -5.52 < 0.001 肾小球滤过率/(mL·min·1.73 m-2) Glomeruar filtration rate/(mL·min·1.73 m-2) 117.65(106.20, 135.60) 117.65(98.00, 134.05) -1.68 0.094 尿酸/(μmol·L-1) Uric acid/(μmol·L-1) 326.00(275.00, 378.00) 305.00(253.00, 363.00) 3.57 < 0.001 血清骨钙素/(μg·L-1) Serum osteocalcin/(μg·L-1) 12.26(9.87, 15.85) 12.13(9.45, 15.75) 0.57 0.163 糖化血红蛋白/% Glycosylated hemoglobin/% 8.40(7.00, 10.00) 9.10(7.40, 10.90) -3.99 < 0.001 空腹血糖/(mmol·L-1) Fasting plasma glucose/(mmol·L-1) 7.76(6.39, 9.85) 8.10(6.78, 10.27) -2.85 0.004 餐后2 h血糖/(mmol·L-1) 2-hour postprandial blood glucose/(mmol·L-1) 15.50(12.90, 18.40) 16.30(13.15, 19.65) -2.79 0.005 空腹胰岛素/(μIU·mL-1) Fasting insulin/(μIU·mL-1) 6.69(4.90, 9.91) 6.69(3.66, 8.34) -4.16 < 0.001 餐后2 h胰岛素/(μIU·mL-1) 2-hour post meal insulin/(μIU·mL-1) 26.22(15.00, 47.20) 24.10(12.05, 40.70) -2.02 < 0.001 胰岛素抵抗指数Homeostasis model assessment insulin resistance 2.51(1.60, 3.86) 2.21(1.34, 3.52) -2.59 0.010 胰岛素敏感指数Homeostasis model assessment insulin sensitivity 32.35(18.16, 58.85) 25.00(13.10, 45.35) -4.62 < 0.001 C-反应蛋白/(mg·L-1) C-reactive protein/(mg·L-1) 2.50(1.70, 3.50) 2.50(1.70, 3.60) -0.27 0.784 注:GLP-1,胰高糖素样肽-1; MCI, 轻度认知功能障碍。
①使用GLP-1药物指使用利拉鲁肽注射液、度拉糖肽注射液; ②以M(P25,P75)或人数(占比/%)或x±s表示。
Note: GLP-1, glucagon-like peptide-1; MCI, mild cognitive impairment.
① The use of GLP-1 drug refers to the use of liraglutide injection and dulaglutide injection; ② M(P25,P75) or number of people (proportion/%) or x±s. -
[1] Li YZ, Teng D, Shi XG, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study[J]. BMJ, 2020, 369: m997. DOI: 10.1136/bmj.m997. [2] Meyhöfer S, Schmid SM. Diabetes complications - diabetes and the nervous system[J]. Dtsch Med Wochenschr, 2020, 145(22): 1599-1605. DOI: 10.1055/a-1038-0102. [3] Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission[J]. Lancet, 2020, 396(10248): 413-446. DOI: 10.1016/S0140-6736(20)30367-6. [4] You Y, Liu ZZ, Chen YN, et al. The prevalence of mild cognitive impairment in type 2 diabetes mellitus patients: a systematic review and meta-analysis[J]. Acta Diabetol, 2021, 58(6): 671-685. DOI: 10.1007/s00592-020-01648-9. [5] 黄倩, 杜蕾, 昌菁, 等. 中青年2型糖尿病患者并发轻度认知功能障碍相关影响因素研究[J]. 现代生物医学进展, 2021, 21(22): 4256-4261. DOI: 10.13241/j.cnki.pmb.2021.22.011.Huang Q, Du L, Chang J, et al. Related factors of mild cognitive impairment in young and middle-aged patients with type 2 diabetes mellitus[J]. Prog Mod Biomed, 2021, 21(22): 4256-4261. DOI: 10.13241/j.cnki.pmb.2021.22.011. [6] 陈新宇, 周军良, 李婷婷, 等. 基于随机森林算法和Logistic回归分析的老年肌肉衰减症影响因素[J]. 中华疾病控制杂志, 2022, 26(3): 357-361. DOI: 10.16462/j.cnki.zhjbkz.2022.03.020.Chen XY, Zhou JL, Li TT, et al. Influential factors of sarcopenia in older adults based on random forest and Logistic regression[J]. Chin J Dis Control Prev, 2022, 26(3): 357-361. DOI: 10.16462/j.cnki.zhjbkz.2022.03.020. [7] 张玮畅, 田晶, 杨弘, 等. 冠心病合并慢性心力衰竭患者5年全因死亡生存分析与可解释性研究[J]. 中华疾病控制杂志, 2023, 27(4): 373-378, 391. DOI: 10.16462/j.cnki.zhjbkz.2023.04.001.Zhang WC, Tian J, Yang H, et al. 5-year all-cause mortality survival analysis and interpretable study in patients with coronary artery disease combined with chronic heart failure[J]. Chin J Dis Control Prev, 2023, 27(4): 373-378, 391. DOI: 10.16462/j.cnki.zhjbkz.2023.04.001. [8] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)(上)[J]. 中国实用内科杂志, 2021, 41(8): 668-695. DOI: 10.19538/j.nk2021080106.Chinese Diabetes Society. Guidelines for prevention and treatment of type 2 diabetes in China (2020 edition) (Ⅰ)[J]. Chin J Pract Intern Med, 2021, 41(8): 668-695. DOI: 10.19538/j.nk2021080106. [9] 李岚. 常用认知障碍评估工具的特点与适用性[J]. 上海护理, 2022, 22(3): 73-75. DOI: 10.3969/j.issn.1009-8399.2022.03.017.Li L. Characteristics and suitability of common cognitive impairment assessment tools[J]. Shanghai Nurs, 2022, 22(3): 73-75. DOI: 10.3969/j.issn.1009-8399.2022.03.017. [10] Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment[J]. J Am Geriatr Soc, 2005, 53(4): 695-699. DOI: 10.1111/j.1532-5415.2005.53221.x. [11] Pinto TCC, Machado L, Bulgacov TM, et al. Is the montreal cognitive assessment (MoCA) screening superior to the mini-mental state examination (MMSE) in the detection of mild cognitive impairment (MCI) and Alzheimer's Disease (AD) in the elderly?[J]. Int Psychogeriatr, 2019, 31(4): 491-504. DOI: 10.1017/S1041610218001370. [12] Li J, Zhang WY, Wang X, et al. Functional magnetic resonance imaging reveals differences in brain activation in response to thermal stimuli in diabetic patients with and without diabetic peripheral neuropathy[J]. PLoS One, 2018, 13(1): e0190699. DOI: 10.1371/journal.pone.0190699. [13] 徐爱红, 李海平, 苏婷婷, 等. 老年骨质疏松症患者的认知功能特点及相关性[J]. 临床与病理杂志, 2022, 42(5): 1130-1135. DOI: 10.3978/j.issn.2095-6959.2022.05.018.Xu AH, Li HP, Su TT, et al. Characteristics and correlation of cognitive function in elderly patients with osteoporosis[J]. Int J Pathol Clin Med, 2022, 42(5): 1130-1135. DOI: 10.3978/j.issn.2095-6959.2022.05.018. [14] 薛承浩, 郭海健, 李明码, 等. 2型糖尿病患者轻度认知功能障碍影响因素的Meta分析[J]. 中国循证医学杂志, 2022, 22(5): 568-574. DOI: 10.7507/1672-2531.202111062.Xue CH, Guo HJ, Li MM, et al. Influencing factors of mild cognitive impairment in patients with type 2 diabetes: a meta-analysis[J]. Chin J Evid Based Med, 2022, 22(5): 568-574. DOI: 10.7507/1672-2531.202111062. [15] 李晶, 袁金环, 王猛, 等. 动脉硬化程度对糖尿病患者认知功能的影响研究[J]. 中国全科医学, 2020, 23(19): 2417-2422. DOI: 10.12114/j.issn.1007-9572.2019.00.688.Li J, Yuan JH, Wang M, et al. Impact of arterial stiffness level on cognitive function among diabetic patients[J]. Chin Gen Pract, 2020, 23(19): 2417-2422. DOI: 10.12114/j.issn.1007-9572.2019.00.688. [16] 姚瑶, 褚敏. 糖尿病肾病患者认知功能障碍与血清β淀粉样蛋白的关系[J]. 临床荟萃, 2022, 37(9): 813-816. DOI: 10.3969/j.issn.1004-583X.2022.09.009.Yao Y, Chu M. Relationship between serum amyloid β-protein and cognitive dysfunction in patients with diabetic kidney disease[J]. Clin Focus, 2022, 37(9): 813-816. DOI: 10.3969/j.issn.1004-583X.2022.09.009. [17] 刘晶晶, 李楠楠. 高龄老人体位性低血压对轻度认知功能障碍的影响[J]. 中国实用内科杂志, 2021, 41(4): 315-320. DOI: 10.19538/j.nk2021040111.Liu JJ, Li NN. Effect of postural hypotension on mild cognitive impairment in the elderly[J]. Chin J Pract Intern Med, 2021, 41(4): 315-320. DOI: 10.19538/j.nk2021040111. [18] Ehtewish H, Arredouani A, El-Agnaf O. Diagnostic, prognostic, and mechanistic biomarkers of diabetes mellitus-associated cognitive decline[J]. Int J Mol Sci, 2022, 23(11): 6144. DOI: 10.3390/ijms23116144. [19] 冯莓婷, 刘佳昊, 王晓丽. 血清25-羟维生素D、同型半胱氨酸、尿酸水平与老年高血压患者发生轻度认知功能障碍的相关性[J]. 江苏大学学报(医学版), 2023, 33(3): 252-257, 264. DOI: 10.13312/j.issn.1671-7783.y220276.Feng MT, Liu JH, Wang XL. Relationship between serum 25-hydroxyvitamin D, homocysteine, uric acid and mild cognitive impairment in elderly patients with hypertension[J]. J Jiangsu Univ (Med Ed), 2023, 33(3): 252-257, 264. DOI: 10.13312/j.issn.1671-7783.y220276. -





 下载:
下载: