A cohort study of the effect of sleep duration on possible sarcopenia in rural middle-aged and elderly people in China
-
摘要:
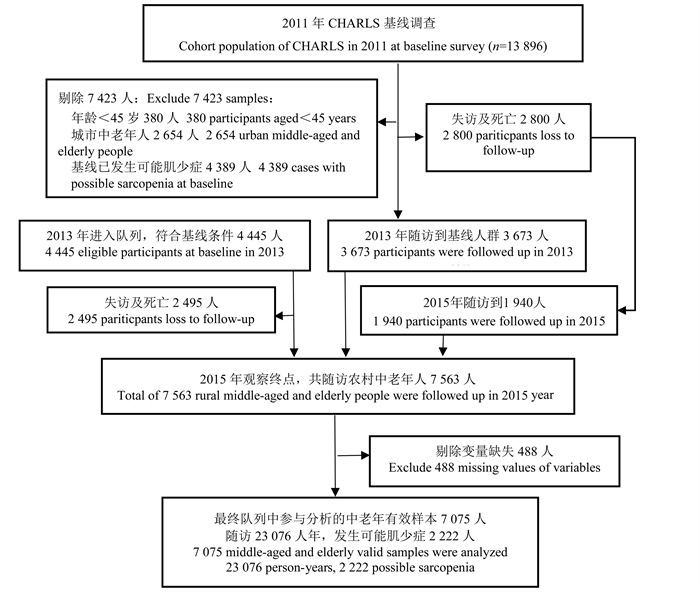
目的 探讨中国农村中老年人(≥45岁)睡眠时长对可能肌少症发生风险的影响,以便降低可能肌少症的发生率。 方法 采用队列研究方法,通过测量握力和重复5次起坐时间判断是否患可能肌少症,以“中国健康与养老追踪调查”2011年和2013年收集到的7 075名未发生可能肌少症的中老年人作为基线数据,随访该队列人群至2015年,构建动态队列数据库,采用Cox比例风险模型研究农村中老年人的睡眠时长与其可能肌少症发生风险的关联。 结果 与睡眠时长为8~ < 9 h的农村中老年人相比,睡眠时长 < 6 h、6~ < 7 h、7~ < 8 h和≥9 h的中老年人可能肌少症的发生风险分别增加22%(HR=1.22, 95% CI: 1.07~1.39, P=0.003)、17%(HR=1.17, 95% CI: 1.01~1.35, P=0.037)、18%(HR=1.18, 95% CI: 1.02~1.35, P=0.022)和16%(HR=1.16, 95% CI: 1.02~1.33, P=0.028)。趋势检验结果显示,随着睡眠时间的缩短(< 9 h)农村中老年人患可能肌少症的风险升高,存在剂量-反应关系(P < 0.001);对于45~<60岁中年人,相较8~ < 9 h睡眠时长,睡眠时长 < 6 h、6~ < 7 h和7~ < 8 h的中年人可能肌少症的发生风险分别增加21%(HR=1.21, 95% CI: 1.01~1.46, P=0.041)、23%(HR=1.23, 95% CI: 1.02~1.48, P=0.033)和30%(HR=1.30, 95% CI: 1.08~1.56, P=0.005);与8~ < 9 h睡眠时长相比,女性中老年人睡眠时长 < 6 h发生可能肌少症的风险增加了27%(HR=1.27, 95% CI: 1.06~1.52, P=0.010),男性中老年人睡眠时长≥9 h发生可能肌少症的风险增加了21%(HR=1.21, 95% CI: 1.01~1.46, P=0.045)。 结论 中国农村中老年人的睡眠时间过短和过长均会增加可能肌少症的发生风险,并且存在年龄差异,优化睡眠时长可以预防肌少症的发生发展。 Abstract:Objective To explore the effect of sleep duration on the risk of possible sarcopenia in rural middle-aged and elderly adults (≥45 years) in order to reduce the incidence of possible sarcopenia. Methods The cohort study was conducted base on the Chinese health and retirement longitudinal study (CHARLS). Possible sarcopenia was identified by measuring grip strength and five repetitions of sitting-up time. A total of 7 075 participants of middle-aged and elderly adults aged ≥45 years without possible sarcopenia in 2011 and 2013 were used as baseline data, and were followed up until 2015. Cox proportional risk model was used to explore the association between sleep duration and the risk of possible sarcopenia in rural middle-aged and elderly people. Results Compared to rural middle-aged and elderly adults with sleep duration of 8- < 9 hours, those with sleep duration less than 6 hours, 6- < 7 hours, 7- < 8 hours and more than 9 hours had an increased risk of possible sarcopenia by 22% (HR=1.22, 95% CI: 1.07-1.39, P=0.003), 17% (HR=1.17, 95% CI: 1.01-1.35, P=0.037), 18% (HR=1.18, 95% CI: 1.02-1.35, P=0.022) and 16% (HR=1.16, 95% CI: 1.02-1.33, P=0.028) respectively. Trend test showed that the risk of possible sarcopenia increased with the shortening of sleep time (< 9 h), and there was a dose-response relationship (P < 0.001). Among participants aged 45- < 60 years, compared with sleep duration of 8- < 9 hours, the risk of possible sarcopenia with sleep duration less than 6 hours, 6- < 7 hours and 7- < 8 hours was increased by 21% (HR=1.21, 95% CI: 1.01-1.46, P=0.041), 23% (HR=1.23, 95% CI: 1.02-1.48, P=0.033) and 30% (HR=1.30, 95% CI: 1.08-1.56, P=0.005), respectively. Compared with sleep duration of 8- < 9 hours, short sleep duration (< 6 h) was associated with a 27% increased risk of possible sarcopenia in females (HR=1.27, 95% CI: 1.06-1.52, P=0.010), and long sleep duration (≥9 h) was associated with a 21% increased risk of possible sarcopenia in males (HR=1.21, 95% CI: 1.01-1.46, P=0.045). Conclusions The shorter and longer sleep duration among rural middle-aged and elderly were associated with an increased risk of possible sarcopenia, and there existed age differences. Optimizing sleep duration may prevent the occurrence and development of sarcopenia. -
Key words:
- Possible sarcopenia /
- Sleep duration /
- Cohort study /
- Middle-aged and elderly adults /
- Rural
-
表 1 农村中老年人基线暴露因素与睡眠时长分布
Table 1. Distribution of baseline exposure factors and sleep duration in rural middle-aged and elderly people
变量Variables 例数
Cases
(n=7 075)< 6 h ①
(n=1 583)6~ < 7 h ①
(n=1 203)7~ < 8 h ①
(n=1 357)8~ < 9 h ①
(n=1 422)≥9 h ①
(n=1 510)性别Gender 男Male 3 517 639(40.37) 587(48.79) 708(52.17) 770(54.15) 813(53.84) 女Female 3 558 944(59.63) 616(51.21) 649(47.83) 652(45.85) 697(46.16) 年龄组/岁Age group/years 45~<60 4 471 891(56.29) 803(66.75) 890(65.59) 973(68.42) 914(60.53) ≥60 2 604 692(43.71) 400(33.25) 467(34.41) 449(31.58) 596(39.47) 婚姻状况Marital status 在婚Married 6 432 1 384(87.43) 1 110(92.27) 1 244(91.67) 1 328(93.39) 1 366(90.46) 不在婚Single 643 199(12.57) 93(7.73) 113(8.33) 94(6.61) 144(9.54) 受教育程度Education level 文盲Illiterate 1 875 549(34.68) 317(26.35) 287(21.15) 324(22.78) 398(26.36) 小学及以下Elementary school or below 3 194 740(46.75) 537(44.64) 621(45.76) 649(45.64) 647(42.85) 初中及以上Middle school or above 2 006 294(18.57) 349(29.01) 449(33.09) 449(31.58) 465(30.79) 工作状况Job status 未工作No work 1 035 287(18.13) 181(15.04) 165(12.16) 173(12.17) 229(15.17) 从事农业工作Agricultural work 5 468 1 214(76.69) 914(75.98) 1 059(78.04) 1 114(78.34) 1 167(77.28) 从事非农工作Non-agricultural work 572 82(5.18) 108(8.98) 133(9.80) 135(9.49) 114(7.55) 过去1个月参与社交活动Participated in social activities last month 否No 780 209(13.20) 124(10.31) 1 47(10.83) 144(10.13) 156(10.33) 是Yes 6 295 1 374(86.80) 1 079(89.69) 1 210(89.17) 1 278(89.87) 1 354(89.67) 家庭人均收入Household income per capita 偏上High 1 857 398(25.14) 223(18.54) 280(20.63) 269(18.92) 332(21.99) 中上Middle-high 1 858 460(29.06) 306(25.44) 332(24.47) 356(25.04) 404(26.75) 中下Middle-low 1 858 385(24.32) 328(27.27) 355(26.16) 396(27.84) 394(26.09) 偏下Low 1 502 340(21.48) 346(28.75) 390(28.74) 401(28.20) 380(25.17) 吸烟Smoking 否No 4 115 1 011(63.87) 710(59.02) 752(55.42) 797(56.05) 845(55.96) 是Yes 2 960 572(36.13) 493(40.98) 605(44.58) 625(43.95) 665(44.04) 饮酒Drinking 否No 4 523 1 089(68.79) 746(62.01) 825(60.80) 906(63.71) 957(63.38) 是Yes 2 552 494(31.21) 457(37.99) 532(39.20) 516(36.29) 553(36.62) BMI/(kg·m-2) 体重过低Underweight (< 18.5) 394 141(8.91) 64(5.32) 63(4.64) 64(4.50) 62(4.11) 标准Standard (18.5~23.9) 3 935 932(58.88) 672(55.86) 732(53.94) 792(55.70) 807(53.44) 超重Overweight (24.0~27.9) 2 032 389(24.57) 356(29.59) 422(31.10) 416(29.25) 449(29.73) 肥胖Obesity (≥28.0) 714 121(7.64) 111(9.23) 140(10.32) 150(10.55) 192(12.72) 慢性病Chronic disease 无No 2 849 524(33.10) 480(39.90) 560(41.27) 627(44.09) 658(43.58) 有Yes 4 226 1 059(66.90) 723(60.10) 797(58.73) 795(55.91) 852(56.42) 日常生活活动能力Activity of daily living 完好Well 6 399 1 348(85.15) 1 108(92.10) 1 247(91.89) 1 321(92.90) 1 375(91.06) 受损Impaired 676 235(14.85) 95(7.90) 110(8.11) 101(7.10) 135(8.94) 注:①以人数(占比/%)表示。
Note: ① Number of people(proportion/%).表 2 农村中老年人按基线暴露因素分层的可能肌少症发生率
Table 2. Incidence of possible sarcopenia stratified by baseline exposure in rural middle-aged and elderly people
变量Variables 例数
Cases
(n=7 075)可能肌少症
人数(占比/%)
Number of possible
sarcopenia
(proportion/%)生存时间/人年
Survival time/person-years,
x±sχ2值
valueP值
value性别Gender 17.60 < 0.001 男Male 3 517 1 044(29.68) 3.33±0.94 女Female 3 558 1 178(33.11) 3.20±0.98 年龄组/岁Age group/years 187.66 < 0.001 45~<60 4 471 1 174(26.26) 3.35±0.94 ≥60 2 604 1 048(40.25) 3.12±0.99 婚姻状况Marital status 40.01 < 0.001 在婚Married 6 432 1 962(30.50) 3.28±0.96 不在婚Single 643 260(40.44) 3.05±1.00 受教育程度Education level 180.92 < 0.001 文盲Illiterate 1 875 743(39.63) 3.10±1.00 小学及以下Elementary school or below 3 194 1 037(32.47) 3.26±0.97 初中及以上Middle school or above 2 006 442(22.03) 3.42±0.91 工作状况Job status 81.37 < 0.001 未工作No work 1 035 418(40.39) 3.12±1.00 从事农业工作Agricultural work 5 468 1 680(30.72) 3.27±0.96 从事非农工作Non-agricultural work 572 124(21.68) 3.44±0.90 过去1个月参与社交活动Participated in social activities last month 7.12 0.008 否No 780 154(19.74) 2.01±0.12 是Yes 6 295 2 068(32.85) 3.42±0.91 家庭人均收入Household income per capita 41.90 < 0.001 偏上High 1 857 511(27.52) 3.34±0.94 中上Middle-high 1 858 555(29.87) 3.31±0.95 中下Middle-low 1 858 628(33.80) 3.20±0.98 偏下Low 1 502 528(35.15) 3.18±0.98 吸烟Smoking 6.92 0.009 否No 4 115 1 331(32.35) 3.23±0.97 是Yes 2 960 891(30.10) 3.31±0.95 饮酒Drinking 10.76 0.001 否No 4 523 1 473(32.57) 3.24±0.97 是Yes 2 552 749(29.35) 3.31±0.95 BMI/(kg·m-2) 40.90 < 0.001 过低Underweight (< 18.5) 394 179(45.43) 3.23±0.97 标准Standard (18.5~23.9) 3 935 1 260(32.02) 3.28±0.96 超重Overweight (24.0~27.9) 2 032 579(28.49) 3.23±0.97 肥胖Obesity (≥28.0) 714 204(28.57) 3.28±0.96 慢性病Chronic disease 17.73 < 0.001 无No 2 849 763(26.78) 3.13±0.99 有Yes 4 226 1 459(34.52) 3.35±0.94 日常生活活动能力Activity of daily living 59.84 < 0.001 完好Well 6 399 1 934(30.22) 3.28±0.96 受损Impaired 676 288(42.60) 3.05±1.00 睡眠时长/h Sleep duration/h 41.77 < 0.001 < 6 1 583 574(36.26) 3.17±0.99 6~<7 1 203 372(30.92) 3.26±0.97 7~<8 1 357 417(30.73) 3.25±0.97 8~<9 1 422 373(26.23) 3.31±0.95 ≥9 1 510 486(32.19) 3.32±0.95 表 3 农村中老年人睡眠时长与可能肌少症发生风险关联的Cox回归模型分析
Table 3. Association of sleep duration and risk of possible sarcopenia in rural middle-aged and elderly people by Cox regression model analysis
睡眠时长/h
Sleep duration/h45~<60岁/years (n=4 471) ≥60岁/years (n=2 604) 合计Total (n=7 075) HR值 ② value ②
(95% CI)P值
valueHR值 ② value ②
(95% CI)P值
valueHR值 ② value ②
(95% CI)P值
value< 6 1.21(1.01~1.46) 0.041 1.20(0.99~1.46) 0.063 1.22(1.07~1.39) 0.003 6~<7 1.23(1.02~1.48) 0.033 1.07(0.86~1.34) 0.535 1.17(1.01~1.35) 0.037 7~<8 1.30(1.08~1.56) 0.005 1.03(0.83~1.28) 0.757 1.18(1.02~1.35) 0.022 8~<9 1.00 1.00 1.00 ≥9 1.17(0.97~1.41) 0.098 1.15(0.94~1.41) 0.163 1.16(1.02~1.33) 0.028 P值 ① value ① < 0.001 注:①为检验睡眠时长和年龄组交互作用在2个年龄组之间差别的P值;②调整了性别、婚姻状况、受教育程度、工作状况、社交活动参与、家庭人均年收入、吸烟、饮酒、BMI、慢性病和日常生活活动能力的混杂影响后的风险比值。
Note: ① P value to examine the difference in sleep duration and age interaction between the two age groups; ② The hazard ration adjusted for the confounding effects of age, marital status, education, job status, social activities, household income per capita, smoke, drink, BMI, chronic disease and activity of daily living.表 4 农村中老年人不同性别睡眠时长与可能肌少症发生风险关联的Cox回归模型分析
Table 4. Association of sleep duration and risk of possible sarcopenia in rural middle-aged and elderly with different genders by Cox regression model analysis
睡眠时长/h
Sleep duration/h男性Male (n=3 517) 女性Female (n=3 558) HR值 ② value ②
(95% CI)P值
valueHR值 ② value ②
(95% CI)P值
value< 6 1.13(0.92~1.38) 0.236 1.27(1.06~1.52) 0.010 6~7 1.20(0.98~1.47) 0.083 1.14(0.93~1.39) 0.209 7~8 1.20(0.98~1.45) 0.076 1.17(0.96~1.43) 0.121 8~9 1.00 1.00 ≥9 1.21(1.01~1.46) 0.045 1.13(0.93~1.37) 0.222 P值 ① value ① 0.332 注:①为检验睡眠时长和性别交互作用在2个性别组之间差别的P值;②调整了年龄、婚姻状况、受教育程度、工作状况、社交活动参与、家庭人均年收入、吸烟、饮酒、BMI、慢性病和日常生活活动能力的混杂影响后的风险比值。
Note: ① P value to examine the difference in sleep duration and gender interaction between the two gender groups; ② The hazard ration adjusted for the confounding effects of age, marital status, education, job status, social activities, household income per capita, smoke, drink, BMI, chronic disease and activity of daily living. -
[1] 崔王殊, 魏玥, 梁博, 等. 中国中老年人慢性共患病对肌少症发生风险的影响[J]. 中华骨质疏松和骨矿盐疾病杂志, 2022, 15(6): 629-637. DOI: 10.3969/j.issn.1674-2591.2022.06.003.Cui WS, Wei Y, Liang B, et al. Effects of chronic disease comorbidity on the risk of possible sarcopenia among Chinese middle-aged and older adults[J]. Chin J Osteoporos Bone Miner Res, 2022, 15(6): 629-637. DOI: 10.3969/j.issn.1674-2591.2022.06.003. [2] Pourmotabbed A, Ghaedi E, Babaei A, et al. Sleep duration and sarcopenia risk: a systematic review and dose-response meta-analysis[J]. Sleep Breath, 2020, 24(4): 1267-1278. DOI: 10.1007/s11325-019-01965-6. [3] Han PP, Hou L, Liang ZW, et al. Both short and long sleep durations are risk factors for sarcopenia in suburban-dwelling older Chinese individuals: a 3-year longitudinal study[J]. Nat Sci Sleep, 2022, 14: 1089-1096. DOI: 10.2147/NSS.S361925. [4] Shibuki T, Iida M, Harada S, et al. The association between sleep parameters and sarcopenia in Japanese community-dwelling older adults[J]. Arch Gerontol Geriatr, 2023, 109: 104948. DOI: 10.1016/j.archger.2023.104948. [5] Hu XY, Jiang JJ, Wang HZ, et al. Association between sleep duration and sarcopenia among community-dwelling older adults: a cross-sectional study[J]. Medicine(Baltimore), 2017, 96(10): e6268. DOI: 10.1097/MD.0000000000006268. [6] Smith L, Shin JI, Veronese N, et al. Sleep duration and sarcopenia in adults aged ≥65 years from low and middle-income countries[J]. Aging Clin Exp Res, 2022, 34(7): 1573-1581. DOI: 10.1007/s40520-022-02074-3. [7] Nakakubo S, DoiT, Tsutsumimoto K, et al. Sleep duration and progression to sarcopenia in Japanese community-dwelling older adults: a 4 year longitudinal study[J]. J Cachexia Sarcopenia Muscle, 2021, 12(4): 1034-1041. DOI: 10.1002/jcsm.12735. [8] Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment[J]. J Am Med Dir Assoc, 2020, 21(3): 300-307. e2. DOI: 10.1016/j.jamda.2019.12.012. [9] Zhao YH, Hu YS, Smith JP, et al. Cohort profile: the China health and retirement longitudinal study (CHARLS)[J]. Int J Epidemiol, 2014, 43(1): 61-68. DOI: 10.1093/ije/dys203. [10] Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary[J]. Sleep Health, 2015, 1(1): 40-43. DOI: 10.1016/j.sleh.2014.12.010. [11] Kwon YJ, Jang SY, Park EC, et al. Long sleep duration is associated with sarcopenia in Korean adults based on data from the 2008-2011 KNHANES[J]. J Clin Sleep Med, 2017, 13(9): 1097-1104. DOI: 10.5664/jcsm.6732. [12] Huang WC, Lin CY, Togo F, et al. Nonlinear associations between sleep patterns and sarcopenia risks in older adults[J]. J Clin Sleep Med, 2022, 18(3): 731-738. DOI: 10.5664/jcsm.9698. [13] Lee H, Kim S, Kim BS, et al. Sexual difference in effect of long sleep duration on incident Sarcopenia after two years in community-dwelling older adults[J]. Ann Geriatric Med Res, 2022, 26(3): 264-274. DOI: 10.4235/agmr.22.0093. [14] 刘洲, 汪海伟, 张晓丹. 老年女性肌少症与睡眠质量的关联性[J]. 中华骨质疏松和骨矿盐疾病杂志, 2020, 13(5): 432-439. DOI: 10.3969/j.issn.1674-2591.2020.05.006.Liu Z, Wang HW, Zhang XD. Relationship between sarcopenia and sleep quality in elderly women[J]. Chin J Osteoporos Bone Miner Res, 2020, 13(5): 432-439. DOI: 10.3969/j.issn.1674-2591.2020.05.006. [15] Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty[J]. Nat Rev Cardiol, 2018, 15(9): 505-522. DOI: 10.1038/s41569-018-0064-2. [16] Piovezan RD, Abucham J, Dos Santos RVT, et al. The impact of sleep on age-related sarcopenia: possible connections and clinical implications[J]. Ageing Res Rev, 2015, 23(Pt B): 210-220. DOI: 10.1016/j.arr.2015.07.003. [17] Pyykkönen AJ, Isomaa B, Pesonen AK, et al. Sleep duration and insulin resistance in individuals without type 2 diabetes: the PPP-Botnia study[J]. Ann Med, 2014, 46(5): 324-329. DOI: 10.3109/07853890.2014.902226. [18] Anderson LJ, Liu HM, Garcia JM. Sex differences in muscle wasting[J]. Adv Exp Med Biol, 2017, 1043: 153-197. DOI: 10.1007/978-3-319-70178-3_9. [19] Gheller BJF, Riddle ES, Lem MR, et al. Understanding age-related changes in skeletal muscle metabolism: differences between females and males[J]. Annu Rev Nutr, 2016, 36: 129-156. DOI: 10.1146/annurev-nutr-071715-050901. [20] Lauderdale DS, Knutson KL, Yan LL, et al. Self-reported and measured sleep duration: how similar are they?[J]. Epidemiology, 2008, 19(6): 838-845. DOI: 10.1097/EDE.0b013e318187a7b0. -





 下载:
下载: