Preoperative albumin-globulin ratio and prognosis of patients with esophageal squamous cell carcinoma
-
摘要:
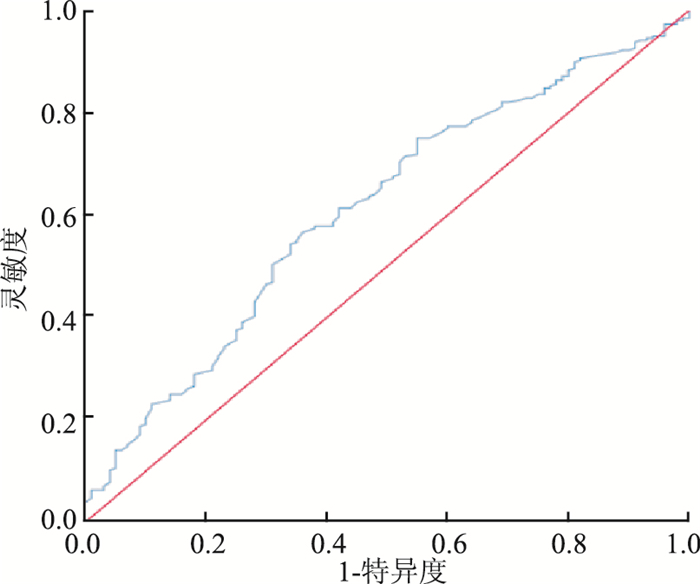
目的 探讨术前白球蛋白比(albumin/globulin ratio,AGR)与食管鳞癌(esophageal squamous cell carcinoma,ESCC)患者预后的关系,建立ESCC手术患者生存时间的预测列线图,为ESCC患者的预后预测提供参考依据。 方法 收集2014年2月-2017年9月在福建省肿瘤医院收治的390例接受过手术治疗的ESCC患者的临床资料。利用接受者操作特征曲线(receiver operating characteristic curves,ROC)确定术前AGR的最佳临界值,χ2检验分析AGR与一般临床特征间的相关性,Cox比例风险回归模型分析AGR与ESCC患者预后的关系,进而构建ESCC术后患者预后预测列线图模型。 结果 按术前AGR最佳临界值1.16将患者分为高AGR和低AGR两组,高AGR组1年和3年生存率均高于低AGR组(均有P < 0.05)。多因素分析结果显示:T分期、N分期、AGR是影响ESCC患者预后的因素(均有P < 0.05),其中T3-T4 vs T1-T2(HR=1.87,95% CI:1.04~3.35),N+ vs N0(HR=1.89,95% CI:1.13~3.17),高AGR组vs低AGR组(HR=0.57,95% CI:0.36~0.90)。预测ESCC术后患者预后的列线图一致性指数为0.68(95% CI:0.62~0.73,P < 0.001)。 结论 术前AGR水平是影响ESCC术后患者预后的因素,高AGR组ESCC患者的预后优于低AGR组,列线图有助于临床医生对ESCC术后患者的预后进行个体化预测。 Abstract:Objective To investigate the relationship between albumin/globulin ratio (AGR) and postoperative survival among patients with esophageal squamous cell carcinoma(ESCC) undergoing radical oesophagectomy, to establish an effective prognostic nomogram for ESCC and to provide a reference for prognosis prediction of ESCC. Methods From February 2014 to September 2017, 390 ESCC patients who underwent surgery were retrospectively enrolled from the tumor hospital in Fujian Province. The receiver operating characteristic curves(ROC) were applied to establish optimal cutoff points. Chi-square test was used to estimate the relationship between the AGR and the clinical features. Cox proportional hazards model was used to estimate the HR and 95% CI for the associations between AGR and Prognosis of ESCC patients. A nomogram model was established to predict the outcome of ESCC patients. Results The ROC demonstrated the best cutoff value for AGR was 1.16. A total of 356 patients were recruited in the final analysis, who were divided into the high AGR group (≥ 1.16) and the low AGR group (< 1.16) by the best cutoff value. Both 1-year and 3-year survival rates in the high AGR group were higher than those detected in the low AGR group(all P < 0.05). Multivariate analysis showed that the T stage, N stage, and AGR were independent prognostic factors of overall survival(all P < 0.05). The HR of T stage was 1.87 (T3-T4 vs T1-T2, 95% CI: 1.04-3.35); The HR of N stage was1.89 (N+ vs N0, 95% CI: 1.13-3.17); The HR of AGR was 0.57(the high AGR group vs the low AGR group, 95%CI: 0.36-0.90). The concordance index(C-index) of the nomogram to predict overall survival was 0.68 (95% CI: 0.62-0.73, P < 0. 001). Conclusions The AGR was an independent prognosis factor for operated ESCC patients. The prognosis of ESCC in the high AGR group was better than that in the low AGR group and the prognostic nomogram provides individualized risk estimate of survival in ESCC patients after surgery. -
表 1 术前AGR与ESCC患者一般特征的关系[n(%)]
Table 1. Relationship between preoperative AGR and baseline clinical features of ESCC patients[n(%)]
变量 合计 AGR χ2值 P值 < 1.16 ≥1.16 性别 4.597 0.032 女 94 37 (33.9) 57 (23.1) 男 262 72 (66.1) 190 (76.9) 年龄(岁) 12.768 < 0.001 ≥60 208 79 (72.5) 129 (52.2) < 60 148 30 (27.5) 118 (47.8) 肿瘤部位 4.233 0.237 胸上段 42 9 (8.3) 33 (13.4) 胸中段 172 56 (51.9) 116 (47.2) 胸下段 140 43 (39.8) 97 (39.4) T分期 8.260 0.004 T1~T2 121 25 (23.6) 96 (39.5) T3~T4 228 81 (76.4) 147 (60.5) N分期 3.100 0.078 N0 178 47 (43.5) 131 (53.7) N+ 174 61 (56.5) 113 (46.3) 分化程度 3.098 0.078 高分化 19 6 (5.6) 13 (5.3) 中分化 282 85 (79.4) 197 (81.1) 低分化/未分化 49 16 (15.0) 33 (13.6) 治疗方式 0.960 0.810 单纯手术 207 63 (57.8) 144 (58.3) 手术+放疗 5 1 (0.9) 4 (1.6) 手术+化疗 109 36 (33.3) 73 (29.6) 手术+放化疗 35 9 (8.3) 26 (10.5) 表 2 不同人群高、低AGR分组生存分析
Table 2. Survival analysis of high and low AGR groups in different populations
对象 1年生存率(95% CI) 3年生存率(95% CI) χ2值 P值 总人群 8.887 0.003 低AGR组 85.64%(78.68%~92.60%) 43.95%(30.92%~56.99%) 高AGR组 90.23%(86.26%~94.20%) 63.21%(53.93%~72.50%) T1-T2期人群 0.220 0.639 低AGR组 95.65%(95.57%~95.74%) 69.69%(69.46%~69.92%) 高AGR组 94.99%(94.94%~95.03%) 64.80%(64.61%~64.99%) T3-T4期人群 7.085 0.008 低AGR组 81.87%(81.78%~81.96%) 41.24%(41.10%~41.38%) 高AGR组 88.05%(87.99%~88.11%) 57.36%(57.23%~57.49%) N0期人群 2.425 0.119 低AGR组 89.80%(89.71%~89.90%) 63.37%(63.19%~63.55%) 高AGR组 94.91%(94.87%~94.95%) 72.15%(72.02%~72.29%) N+期人群 2.497 0.114 低AGR组 84.00%(83.90%~84.09%) 38.13%(37.97%~38.28%) 高AGR组 83.24%(83.16%~83.32%) 45.15%(45.00%~45.31%) 表 3 影响ESCC患者预后的单因素与多因素Cox回归分析
Table 3. Univariate and multivariate Cox regression analysis of prognosis in patients with ESCC
变量 单因素 多因素模型1 多因素模型2 多因素模型3 P值 HR(95% CI) 值 P值 HR(95% CI) 值 P值 HR(95% CI) 值 P值 HR(95% CI) 值 性别 0.288 0.145 0.292 0.281 女 1.00 1.00 1.00 1.00 男 1.30(0.80~2.12) 1.50(0.87~2.59) 1.34(0.78~2.29) 1.36(0.78~2.35) 年龄(岁) 0.300 0.605 0.506 0.464 ≥60 1.00 1.00 1.00 1.00 < 60 0.8(0.53~1.22) 0.89(0.56~1.41) 0.85(0.54~1.36) 0.84(0.53~1.34) 肿瘤部位 胸上段 1.00 1.00 1.00 1.00 胸中段 0.512 0.81(0.44~1.51) 0.257 0.69(0.37~1.31) 0.283 0.70(0.37~1.34) 0.311 0.72(0.38~1.36) 胸下段 0.561 0.83(0.44~1.57) 0.283 0.70(0.36~1.35) 0.322 0.71(0.37~1.39) 0.330 0.72(0.39~1.40) T分期 0.001 0.036 0.024 0.025 T1-T2 1.00 1.00 1.00 1.00 T3-T4 2.48(1.48~4.16) 1.87(1.04~3.35) 1.96(1.10~3.53) 1.96(1.09~3.54) N分期 <0.001 0.016 0.007 0.007 N0 1.00 1.00 1.00 1.00 N+ 2.53(1.63~3.92) 1.89(1.13~3.17) 2.03(1.21~3.42) 2.04(1.21~3.43) 分化程度 高分化 1.00 1.00 1.00 1.00 中分化 0.167 2.26(0.71~7.16) 0.322 1.85(0.55~6.20) 0.404 1.67(0.50~5.62) 0.397 1.69(0.55~5.65) 低分化/未分化 0.284 2.03(0.56~7.39) 0.761 1.24(0.31~5.04) 0.801 1.20(0.30~4.87) 0.798 1.20(0.30~4.87) 治疗方式 单纯手术 1.00 1.00 1.00 1.00 手术+放疗 0.421 1.79(0.43~7.40) 0.693 1.34(0.32~5.63) 0.867 1.13(0.27~4.73) 0.850 1.15(0.27~4.87) 手术+化疗 0.324 1.26(0.79~2.01) 0.353 0.77(0.45~1.33) 0.228 0.72(0.42~1.23) 0.244 0.72(0.42~1.25) 手术+放化疗 0.139 1.59(0.86~2.94) 0.535 1.23(0.64~2.39) 0.794 1.09(0.57~2.10) 0.769 1.10(0.57~2.12) AGR 0.003 0.017 < 1.16 1.00 1.00 ≥1.16 0.54(0.35~0.81) 0.57(0.36~0.90) 白蛋白(g/L) 0.252 0.609 < 41.5 1.00 1.00 ≥41.5 0.70(0.38~1.29) 0.84(0.44~1.63) 球蛋白(g/L) 0.552 0.923 < 31.5 1.00 1.00 ≥31.5 1.15(0.73~1.82) 1.03(0.61~1.73) -
[1] 左婷婷, 郑荣寿, 曾红梅, 等. 中国食管癌发病状况与趋势分析[J]. 中华肿瘤杂志, 2016, 38(9): 703-708. DOI: 10.3760/cma.j.issn.0253-3766.2016.09.013.Zuo TT, Zheng RS, Zeng HM, et al. Incidence and trend analysis of esophageal cancer in China[J]. Chin J Oncol, 2016, 38(9): 703-708. DOI: 10.3760/cma.j.issn.0253-3766.2016.09.013. [2] Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012[J]. CA Cancer J Clin, 2012, 65(6): 283-298. DOI: 10.3322/caac.21314. [3] Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008[J]. Int J Cancer, 2010, 127(12): 2893-2917. DOI: 10.1002/ijc.25516. [4] 王强强, 张玉虹, 刘阳晨. 血常规相关指标与食管癌患者治疗效果和预后的关系[J]. 现代肿瘤医学, 2016, 24(14): 2318-2322. DOI: 10.3969/j.issn.1672-4992.2016.14.044.Wang QQ, Zhang YH, Liu YC, et al. Relationship between some indicators in blood-RT and therapeutic efficacy as well as prognosis of patients with esophageal carcinoma[J]. Modern Oncology, 2016, 24(14): 2318-2322. DOI: 10.3969/j.issn.1672-4992.2016.14.044. [5] Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012[J]. Ca Cancer J Clin, 2015, 65(2): 69-90. DOI: 10.3322/caac.21262. [6] Takeshita N, Hoshino I, Mori M, et al. Serum microRNA expression profile: miR-1246 as a novel diagnostic and prognostic biomarker for oesophageal squamous cell carcinoma[J]. Br J Cancer, 2013, 108(3): 644-652. DOI: 10.1038/bjc.2013.8. [7] 张倩倩, 陈伟霖, 林征, 等. 外周血NLR和HWR水平对非手术食管鳞癌患者预后的影响[J]. 中华疾病控制杂志, 2017, 21(9): 930-934. DOI: 10.16462/j.cnki.zhjbkz.2017.09.017.Zhang QQ, Chen WL, Lin Z, et al. Prognostic values of neutrophil-to lymphocyte ratio and hemoglobin-to-white blood cell ratio on non operative esophageal squamous cell carcinoma patients[J]. Chin J Dis Control Prev, 2017, 21(9): 930-934. DOI: 10.16462/j.cnki.zhjbkz.2017.09.017. [8] Zhou T, He X, Fang W, et al. Pretreatment albumin/globulin ratio predicts the prognosis for small-cell lung cancer[J]. Medicine (Baltimore), 2016, 95(12): e3097. DOI: 10.1097/md.0000000000003097. [9] Deng Y, Pang Q, Miao RC, et al. Prognostic significance of pretreatment albumin/globulin ratio in patients with hepatocellular carcinoma[J]. Onco Targets Ther, 2016, 9: 5317-5328. DOI: 10.2147/OTT.S109736. [10] Liu J, Dai Y, Zhou F, et al. The prognostic role of preoperative serum albumin/globulin ratio in patients with bladder urothelial carcinoma undergoing radical cystectomy[J]. Urol Oncol, 2016, 34(11): 484. DOI: 10.1016/j.urolonc.2016.05.024. [11] 相智声, 林征, 刘双, 等. 术前血清CA19-9和NSE对食管鳞癌患者预后的影响[J]. 中华疾病控制杂志, 2019, 23(2): 134-139. DOI: 10.16462/j.cnki.zhjbkz.2019.02.003.Xiang ZS, Lin Z, Liu S, et al. Prognostic values of preoperative serum CA199 and NSE on esophageal squamous cell carcinoma patients[J]. Chin J Dis Control Prev, 2019, 23(2): 134-139. DOI: 10.16462/j.cnki.zhjbkz.2019.02.003. [12] Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature[J]. Nutr J, 2010, 9(1): 69-85. DOI: 10.1186/1475-2891-9-69. [13] Xing Y, Guo ZN, Yan S, et al. Increased globulin and its association with hemorrhagic transformation in patients receiving intra-arterial thrombolysis therapy[J]. Neurosci Bull, 2014, 30(3): 469-476. DOI: 10.1007/s12264-013-1440-x. [14] Park JH, Watt DG, Roxburgh CS, et al. Colorectal cancer, systemic inflammation, and outcome: staging the tumor and staging the host[J]. Ann Surg, 2015, 263(2): 326-336. DOI: 10.1097/SLA.0000000000001122. [15] Groot Kormelink T, Powe DG, Kuijpers SA, et al. Immunoglobulin free light chains are biomarkers of poor prognosis in basal-like breast cancer and are potential targets in tumor-associated inflammation[J]. Oncotarget, 2014, 5(10): 3159-3167. DOI: 10.18632/oncotarget.1868. [16] Guo HW, Yuan TZ, Chen JX, et al. Prognostic value of pretreatment albumin/globulin ratio in digestive system cancers: a meta-analysis[J]. PLoS One, 2018, 13(1): e0189839. DOI: 10.1371/journal.pone.0189839. [17] Suh B, Park S, Shin DW, et al. Low albumin-to-globulin ratio associated with cancer incidence and mortality in generally healthy adults[J]. Ann Oncol, 2014, 25(11): 2260-2266. DOI: 10.1093/annonc/mdu274. [18] Zhang F, Sun P, Wang ZQ, et al. Low preoperative albumin-globulin score predicts favorable survival in esophageal squamous cell carcinoma[J]. Oncotarget, 2016, 7(21): 30550-30560. DOI: 10.18632/oncotarget.8868. [19] Li XH, Gu WS, Wang XP, et al. Low preoperative albumin-to-globulin ratio predict poor survival and negatively correlated with fibrinogen in resectable esophageal squamous cell carcinoma[J]. J Cancer, 2017, 8(10): 1833-1842. DOI: 10.7150/jca.19062. [20] 杨连凯, 李丰科, 张文强, 等. 食管鳞癌患者淋巴结转移的特征、影响因素及其对生存的影响[J]. 肿瘤防治研究, 2017, 44(6): 413-417. DOI: 10.3971/j.issn.1000-8578.2017.16.1278.Yang LK, Li FK, Zhang WQ, et al. Characteristics and influence factors of lymph node metastasis and their effect on survival of esophageal squamous cell carcinoma patients[J]. Cancer Res Prev Treat, 2017, 44(6): 413-417. DOI: 10.3971/j.issn.1000-8578.2017.16.1278. -





 下载:
下载: