Carriage prevalence and drug resistance profile of MRSA and MSSA strains isolated from newborns
-
摘要:
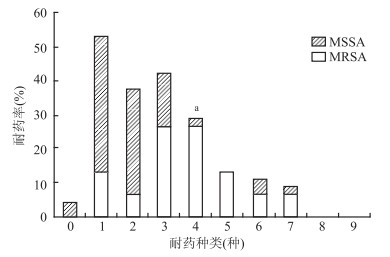
目的 了解新生儿耐甲氧西林金黄色葡萄球菌(methicillin-resistant staphylococcus aureus,MRSA)和甲氧西林敏感金黄色葡萄球菌(methicillin-sensitive staphylococcus aureus,MSSA)的携带现状及其耐药情况。 方法 采用横断面研究,于2015年8月-11月,对深圳市龙华区人民医院和观澜医院的1 834名新生儿进行棉拭子采样、菌株分离鉴定及药物敏感试验。 结果 新生儿金黄色葡萄球菌(staphylococcus aureus,SA)、MRSA、MSSA的携带率分别为3.27%(60/1 834)、0.82%(15/1 834)、2.45%(45/1 834)。MRSA与MSSA对青霉素、红霉素的耐药率较高,对利奈唑胺的耐药率均小于10%。MRSA对红霉素、莫西沙星、克林霉素的耐药率均高于MSSA(均有P < 0.05);MRSA的多重耐药率高达80.00%,风险是MSSA的12.36倍。 结论 该地区新生儿SA尤其是MRSA多重耐药率较高,且MRSA耐药情况比MSSA更严重。 Abstract:Objective To determine the carriage prevalence and antibiotics resistance profile of methicillin-resistant staphylococcus aureus(MRSA) and methicillin-sensitive staphylococcus aureus(MSSA) strains isolated from newborns. Methods A cross-sectional study was conducted in two hospitals in Shenzhen from August to November 2015. Cotton swab samples were collected from 1834 newborns. Staphylococcus aureus was identified by general laboratory tests, and antimicrobial-susceptibility profiles was tested. Results In total, 3.27% (60/1 834) Staphylococcus aureus (SA) strains were isolated, including 0.82% (15/1 834) MRSA and 2.45% (45/1 834) MSSA. Most MRSA and MSSA strains were resistant to penicillin and erythromycin but less than 10% strains resistant to linezolid. Drugs resistance rates of MRSA to erythromycin, moxifloxacin and clindamycin were all higher than that of MSSA (all P < 0.05). The multidrug-resistant risk of MRSA (80.00%) was 12.36 times higher than that of MSSA (24.44%). Conclusions Multidrug-resistant SA especially MRSA strains isolated from newborns had the higher prevalence, the drugs resistance rate of MRSA strains was more serious than that of MSSA. -
Key words:
- Newborns /
- MRSA /
- MSSA /
- Carriage prevalence /
- Antibiotics resistance profile
-
表 1 60名新生儿携带MRSA和MSSA的耐药情况
Table 1. Drugs resistance rates of MRSA and MSSA isolated from 60 newborns
抗生素 MRSA MSSA 合计 χ2值 Pa值 OR值(95% CI) n(例) % n(例) % n(例) % 克林霉素 10 66.67 7 15.56 17 28.33 - < 0.001 10.86(2.38~52.00) 红霉素 13 86.67 15 33.33 28 46.67 12.86 < 0.001 13.00(2.36~127.50) 庆大霉素 2 13.33 3 6.67 5 8.33 - 0.591 2.15(0.16~20.72) 莫西沙星 3 20.00 0 0.00 3 5.00 - 0.013 13.07(1.34~∞) 利奈唑胺 1 6.67 1 2.22 2 3.33 - 0.441 3.14(0.04~252.17) 利福平 3 20.00 2 4.44 5 8.33 - 0.094 5.38(0.53~68.7) 妥布霉素 2 13.33 9 20.00 11 18.33 - 0.714 0.62(0.06~3.61) 替考拉宁 4 26.67 8 17.78 12 20.00 - 0.472 1.68(0.31~7.81) 头孢西丁 12 80.00 0 0.00 12 20.00 - < 0.001 177.23(23.62~∞) 青霉素 13 86.67 43 95.56 56 93.33 - 0.258 0.30(0.02~4.66) 复方新诺明 4 26.67 4 8.89 8 13.33 - 0.098 3.73(0.58~23.01) MDR 12 80.00 11 24.44 23 38.33 14.69 < 0.001 12.36(2.56~76.77) 注:a表示采用Fisher确切概率法; MDR:多重耐药。 -
[1] Tsai MH, Chiu CY, Shih HJ, et al. Longitudinal investigation of nasopharyngeal methicillin-resistant staphylococcus aureus colonization in early infancy: The PATCH birth cohort study[J]. Clin Microbiol Infect, 2017, 23(2): 121-127. DOI: 10.1016/j.cmi.2016.10.020. [2] Jimenez-Truque N, Tedeschi S, Saye EJ, et al. Relationship between maternal and neonatal staphylococcus aureus colonization[J]. Pediatrics, 2012, 129(5): 1252-1259. DOI: 10.1542/peds.2011-2308. [3] 常林惠, 魏晓红, 杨锐. 儿科金黄色葡萄球菌感染的药敏分析[J]. 国际检验医学杂志, 2016, 37(12): 1709-1711. DOI: 10.3969/j.issn.1673-4130.2016.12.049.Chang LH, Wei XH, Yang R. Drug sensitivity analysis of pediatric staphylococcus aureus infection[J]. Int J Lab Med, 2016, 37(12): 1709-1711. DOI: 10.3969/j.issn.1673-4130.2016.12.049. [4] 李春辉, 吴安华. MDR、XDR、PDR多重耐药菌暂行标准定义——国际专家建议[J]. 中国感染控制杂志, 2014, 13(1): 62-64. DOI: 10.3969/j.issn.1671-9638.2014.01.018.Li CH, Wu AH. Interim standard definition of MDR, XDR and PDR multidrug-resistant bacteria-international expert recommendations[J]. Chin J Infec Contl, 2014, 13(1): 62-64. DOI: 10.3969/j.issn.1671-9638.2014.01.018. [5] Abernethy J, Sharland M, Johnson AP, et al. How do the epidemiology of paediatric methicillin-resistant staphylococcus aureus and methicillin-susceptible staphylococcus aureus bacteraemia differ?[J]. J Med Microbiol, 2017, 66(6): 737-743. DOI: 10.1099/jmm.0.000489. [6] Gutierrez K, Halpern MS, Sarnquist C, et al. Staphylococcal infections in children, California, USA, 1985-2009[J]. Emerg Infect Dis, 2013, 19(1): 10-20. DOI: 10.3201/eid1901.111740. [7] Shirai Y, Arai H, Tamaki K, et al. Neonatal methicillin-resistant staphylococcus aureus colonization and infection[J]. Journal of Neonatal-Perinatal Medicine, 2017, 10(4): 439-444. DOI: 10.3233/NPM-16166. [8] Kuo CY, Huang YC, Huang TN, et al. Prevalence and molecular characterization of staphylococcus aureus colonization among neonatal intensive care units in Taiwan[J]. Neonatology, 2014, 105(2): 142-148. DOI: 10.1159/000356733. [9] James L, Gorwitz RJ, Jones RC, et al. Methicillin-resistant staphylococcus aureus infections among healthy full-term newborns[J]. Arch Dis Child Fetal Neonatal Ed, 2008, 93(1): 40-44. DOI: 10.1136/adc.2006.104026. [10] 池嘉陵, 傅倩晰, 何磊, 等. 2014-2017年儿童金黄色葡萄球菌分离株耐药性分析[J]. 重庆医学, 2018, 47(32): 71-74. DOI: 10.3969/j.issn.1671-8348.2018.32.017.Chi JL, Fu QX, He L, et al. Analysis of staphylococcus aureus antimicrobial resistance in children from 2014 to 2017[J]. Chongqing Med, 2018, 47(32): 71-74. DOI: 10.3969/j.issn.1671-8348.2018.32.017. [11] 舒明. 医院MRSA感染危险因素研究[J]. 中国感染控制杂志, 2010, 9(3): 160-163. DOI: 10.3969/j.issn.1671-9638.2010.03.004.Shu M. Risk factors for nosocomial methicillin-resistant staphylococcus aureus infection[J]. Chin J Infec Contl, 2010, 9(3): 160-163. DOI: 10.3969/j.issn.1671-9638.2010.03.004. -





 下载:
下载: