Study on the association between prenatal examinations of Tibetan pregnant women and low birth weight infants
-
摘要:
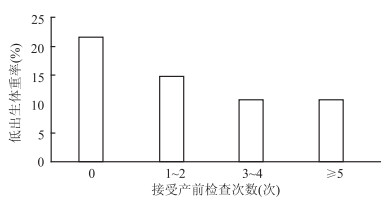
目的 了解西藏藏族孕产妇产前检查次数与低出生体重儿的关联,为提高产前保健质量、减少低出生体重儿的发生提供参考。 方法 选取2012年1月-2018年12月在西藏拉萨市某医院分娩的藏族产妇及新生儿为研究对象,收集所有单胎活产分娩孕产妇的基础资料、分娩资料及新生儿出生资料。采用Logistic回归模型对孕产妇产前检查次数与其分娩的新生儿出生体重进行关联性分析。 结果 5 563例孕产妇,规范产前检查率为10.48%。孕产妇所分娩新生儿中,低出生体重儿占11.32%。随着孕产妇产检次数的增加,新生儿低出生体重率呈现下降趋势(χ2=14.57,P=0.002)。多因素Logistic回归模型显示,在控制了孕产妇年龄、胎儿性别、分娩方式、胎儿窒息等因素后,未接受产前检查和接受1~2次产前检查的孕产妇分娩的低出生体重儿发生率分别是接受规范产前检查孕产妇的1.41倍(95% CI:1.00~1.98)和2.34倍(95% CI:1.09~5.02)。 结论 西藏藏族孕产妇接受规范的产前检查的比例较低,存在较高的低出生体重儿的发生风险。建议加强少数民族地区的妇幼保健工作质量,保障母婴安全。 Abstract:Objective To understand the relationship between the number of prenatal examination during pregnancy in Tibetan mothers and low birth weight infants, and to provide reference for improving the quality of antenatal care and reducing the incidence of low birth weight infants. Methods Tibetan women and newborns who gave birth in a hospital in Lhasa, Tibet from January 2012 to December 2018 were selected as research objects. The basic data, delivery materials and newborn data of all single births were collected. Logistic regression models were used to analyze the relationship between the number of maternal prenatal examinations and the birth weight of the newborn. Results In 5 563 pregnant women, the prenatal check-up rate was 10.48%. Among the newborns, low birth weight accounted for 11.32%. With the increase in the number of maternal births, the neonatal low birth weight rate showed a downward trend (χ2=14.57, P=0.002). Multivariate Logistic regression model showed that after controlling for maternal age, fetal gender, mode of delivery, fetal asphyxia and other confounding factors, the number of low prenatal examinations was still related to the occurrence of low birth weight infants. The incidence of low birth weight infants who gave birth to antenatal check-ups and 1-2 prenatal visits was 1.41 times (95% CI: 1.00-1.98) and 2.34 times (95% CI: 1.09-5.02) higher than those who received standardized prenatal checkups. Conclusions Tibetan pregnant women receive a lower proportion of standardized prenatal examination and there is a higher risk of low birth weight infants. It is recommended to strengthen the quality of maternal and child health care work in minority areas to ensure maternal and child safety. -
Key words:
- Low birth weight infants /
- Antenatal care /
- Prenatal checkup
-
表 1 研究对象基本特征
Table 1. Basic characteristics of the research object
研究对象基本特征 例数(n) 占比(%) 孕产妇 年龄(岁)a ≤20 365 6.57 21~ 1 741 31.32 26~ 1 956 35.19 31~ 1 001 18.01 >35 495 8.91 职业 无业 4 804 86.36 农民 382 6.87 牧民 71 1.28 职工 306 5.50 新生儿 性别 男 2 890 51.95 女 2 673 48.05 窒息程度 无窒息 5 418 97.39 轻度窒息 88 1.58 重度窒息 57 1.02 出生体重(g) < 2 500 630 11.32 2 500~ 4 838 86.97 ≥4 000 95 1.71 注:a数据缺失5例(0.09%) 表 2 不同特征孕产妇的产前检查情况[n(%)]
Table 2. Prenatal examination of pregnant women with different characteristics[n(%)]
孕产妇 例数 未接受产前检查(%) 接受产前检查(%) 接受规范产前检查(%) 合计 5 563 46(0.83) 5 517(99.17) 583(10.48) 年龄(岁)a ≤20 365 6 (1.64) 359(98.36) 23(6.30) 21~ 1 741 16(0.92) 1 725(99.08) 183(10.51) 26~ 1 956 12(0.61) 1 944(99.39) 237(12.12) 31~ 1 001 5(0.50) 996(99.50) 98(9.79) >35 495 7(1.41) 488(98.59) 41(8.28) 职业 无业 4 804 45(0.94) 4 813(99.06) 415(8.64) 农民 382 0(0.00) 388(100.00) 97(25.00) 牧民 71 1(1.41) 70(98.59) 6(8.45) 职工 306 0(0.00) 306(100.00) 65(21.24) 孕次(次) 1 2 178 19(0.87) 2 159(99.13) 268(12.30) >1 3 385 27(0.80) 3 358(99.20) 315(9.31) 产次(次) 1 2 266 19(0.84) 2 247(99.16) 280(12.36) >1 3 297 27(0.82) 3 270(99.18) 303(9.19) 分娩方式 顺产 4 639 45(0.97) 4 594(99.03) 449(9.68) 剖宫产 924 1(0.11) 923(99.89) 134(14.50) 注:a数据缺失5例(0.09%)。 表 3 孕产妇产前检查次数与低出生体重儿发生率的关联性分析
Table 3. Correlation analysis between the number of maternal prenatal examinations and the incidence of low birth weight infants
产前检查 活产数 低出生体重儿(%) 单因素模型 多因素模型 OR(95% CI)值 P值 OR(95% CI)值 P值 未接受产前检查a 46(0.83) 10 (21.74) 2.29(1.09~4.84) 0.030 2.34(1.09~5.02) 0.030 1~2次a 646(11.61) 96 (14.86) 1.44(1.03~2.02) 0.035 1.41(1.00~1.98) 0.050 3~4次 4 288(77.08) 461(10.75) 0.99(0.75~1.31) 0.968 1.01(0.76~1.33) 0.972 接受规范产前检查 583(10.48) 63 (10.81) 1.00 1.00 合计 5 563(100.00) 630(11.32) 注:aP < 0.05,多因素模型控制了孕产妇年龄、胎儿性别、胎儿窒息程度、分娩方式等因素 -
[1] Greenberg RS. The impact of prenatal care in different social groups[J]. Am J Obstet Gynecol, 1983, 145(7): 797-801. DOI: 10.1016/0002-9378(83)90681-6. [2] Eisner V, Brazie JV, Pratt MW, et al. The risk of low birthweight[J]. Am J Public Health, 1979, 69(9): 887-893. DOI: 10.2105/AJPH.69.9.887. [3] Hong R, Ruiz-Beltran M. Low birth weight as a risk factor for infant mortality in Egypt[J]. East Mediterr Health J, 2008, 14(5): 992-1002. http://www.ncbi.nlm.nih.gov/pubmed/19161070 [4] World Health Organization. The world health report 2005: make every mother and child count[EB/OL]. (2005-04-02)[2019-9-19]. https://www.who.int/whr/2005/whr2005_en.pdf?ua=1. [5] Leveno KJ, Cunningham FG, Roark ML, et al. Prenatal care and the low birth weight infant[J]. Obstet Gynecol, 1985, 66(5): 599-605. DOI: 10.1016/0378-5122(85)90061-1. [6] 中华人民共和国卫生部. 母婴健康素养——基本知识与技能(试行)[EB/OL]. (2014-05-16)[2019-06-10]. http://www.nhc.gov.cn/jnr/mrwyzzsxx/201405/0065ee2071204f0c9b52f7cdcbb392f2.shtml.Ministry of Health of the People's Republic of China. Maternal and child health literacy——basic knowledge and skills (trial)[EB/OL]. (2014-05-16)[2019-06-10]. http://www.nhc.gov.cn/jnr/mrwyzzsxx/201405/0065ee2071204f0c9b52f7cdcbb392f2.shtml. [7] 赵凤敏, 郭素芳, 张彤, 等. 不同时期育龄妇女产前保健及影响因素分析[J]. 中国公共卫生, 2006, (1): 9-11. DOI: 10.11847/zgggws2006-22-01-05.Zhao FM, Guo SF, Zhang T, et al. Analysis on influence factors of antenatal care in reproductive aged women of various period[J]. Chin J Public Health, 2006, 22(1): 9-11. DOI: 10.11847/zgggws2006-22-01-05 [8] 唐梦莎, 王德斌, 李洪飞, 等. 中国妇女孕产期保健服务利用地区差异分析[J]. 中国妇幼保健, 2010, 25(24): 3381-3384. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201024000.htmTang MS, Wang DB, Li HF, et al. Analysis on regional differences of services utilization of maternal health care in China[J]. Maternal and Child Health Care of China, 2010, 25(24): 3381-3384. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201024000.htm [9] 陈音汁, 许红, 唐晓君, 等. 中国西部部分少数民族地区产前检查现状及影响因素分析[J]. 华中科技大学学报(医学版), 2013, 42(3): 346-350. DOI: 10.3870/j.issn.1672-0741.2013.03.025.Chen YZ, Xu H, Tang XJ, et al. Current state of prenatal examination and associated influence factors in some western minority-inhabited areas[J]. Acta Med Uni Sci Technol Huazhong, 2013, 42(3): 346-350. DOI: 10.3870/j.issn.1672-0741.2013.03.025 [10] 王泽华. 妇产科学[M]. 第5版. 北京: 人民卫生出版社, 2004.Wang ZH. Obstetrics and gynecology[M]. 5 rd ed. Beijing: People's Medical Publishing House, 2004. [11] 程华, 刘芳, 巴拉卓玛. 高原地区与平原地区孕产妇产前保健及妊娠结局对比分析[J]. 中国妇幼健康研究, 2017, 28(3): 256-258, 269. DOI: 10.3969/j.issn.1673-5293.2017.03.012.Cheng H, Liu F, Bala ZM. Prenatal care and pregnancy outcomes of women from plateau region and plain region[J]. Chinese Journal of Woman and Child Health Research, 2017, 28(3): 256-258, 269. DOI: 10.3969/j.issn.1673-5293.2017.03.012. [12] 鲜恩英, 陈瑞华, 董海. 拉萨市林周县农牧民孕产妇产前保健现状及影响因素分析[J]. 卫生职业教育, 2013, 31(4): 126-127. DOI: 10.3969/j.issn.1671-1246.2013.04.071Xian EY, Chen RH, Dong H. Lhasa linzhou county farmers and herdsmen maternal prenatal care status and influence factors analysis[J]. Health Vocational Education, 2013, 31(4): 126-127. DOI: 10.3969/j.issn.1671-1246.2013.04.071 [13] World Health Organization. Global nutrition targets 2025: low birth weight policy brief[EB/OL]. (2014-10-08)[2019-09-19]. https://apps.who.int/iris/bitstream/handle/10665/149020/WHO_NMH_NHD_14.5_eng.pdf?ua=1. [14] 陈奕, 李光辉, 邹丽颖, 等. 我国低出生体重儿的影响因素[J]. 中华围产医学杂志, 2015, 18(10): 755-760. DOI: 10.3760/cma.j.issn.1007-9408.2015.10.008.Chen Y, Li GH, Zou LY, et al. Influencing factors of low birth weight infants in China[J]. Chin J Perinat Med, 2015, 18(10): 755-760. DOI: 10.3760/cma.j.issn.1007-9408.2015.10.008. [15] 边巴卓玛, 普布卓玛, 康轶君. 拉萨市藏族新生儿出生体重及其影响因素[J]. 中华围产医学杂志, 2014, 17(6): 418-420. DOI: 10.3760/cma.j.issn.1007-9408.2014.06.017Bianba ZM, Pubu ZM, Kang YJ. Birth weight of Tibetan newborns in Lhasa and its influencing factors[J]. Chin J Perinat Med, 2014, 17(6): 418-420. DOI: 10.3760/cma.j.issn.1007-9408.2014.06.017 [16] 徐小红, 普布卓玛, 格央, 等. 高海拔地区低出生体重儿发生规律及相关因素分析[J]. 中国实用妇科与产科杂志, 2018, 34(3): 293-297. DOI: 10.19538/j.fk2018030115.Xu XH, Pubu ZM, Ge Y, et al. Occurrence and related factors of low birth weight infants in high altitude areas[J]. Chin J Pract Gynecol Obstetr, 2018, 34(3): 293-297. DOI: 10.19538/j.fk2018030115. [17] 胡美娜, 赵银珠, 邹晓璇, 等. 低出生体重发生率及影响因素[J]. 中国生育健康杂志, 2019, 30(2): 127-130. https://www.cnki.com.cn/Article/CJFDTOTAL-SYJK201902006.htmHu MN, Zhao YZ, Zou XX, et al. Analysis on incidence and risk factors of low birth weight[J]. Chin J Reprod Heal, 2019, 30(2): 127-130. https://www.cnki.com.cn/Article/CJFDTOTAL-SYJK201902006.htm [18] 甘伟红, 李翠苑. 孕妇在产前门诊中规律接受产前保健对妊娠结局影响分析[J]. 现代诊断与治疗, 2017, 28(23): 4475-4476. doi: 10.3969/j.issn.1001-8174.2017.23.100Gan WH, Li CY. Analysis on the influence of regular prenatal care on pregnancy outcome of pregnant women in prenatal clinic[J]. Modern Diagn Treat, 2017, 28(23): 4475-4476. doi: 10.3969/j.issn.1001-8174.2017.23.100 [19] 黄渊清. 低出生体重儿发生的危险因素及干预研究[D]. 福州: 福建医科大学, 2008.Huang YQ. Study on the risk factors and intervention of low birth weight infants[D]. Fuzhou: Fujian Medical University, 2008. [20] 胡成文. 妊娠相关因素对新生儿出生体重及身长的影响研究[D]. 合肥: 安徽医科大学, 2008.Hu CW. Study on factors related to pregnancy and neonatal birth size[D]. Hefei: Anhui Medical University, 2008. -





 下载:
下载: