-
摘要:
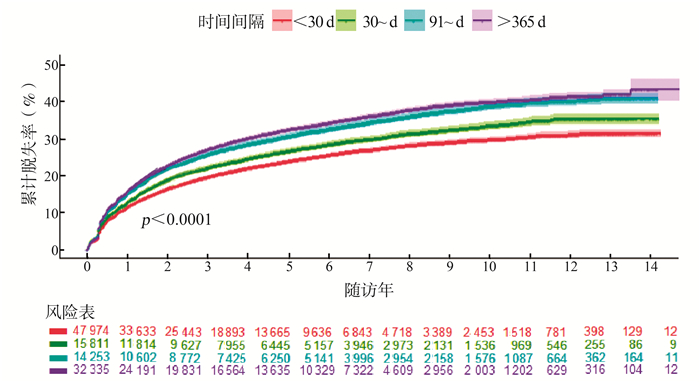
目的 分析从人类免疫缺陷病毒(human immunodeficiency virus, HIV)确诊到启动治疗时间间隔对艾滋病抗病毒治疗中患者脱失的影响,为指导动员治疗咨询提供参考。 方法 对云南省15年艾滋病抗病毒治疗(antiretroviral therapy, ART)数据回顾性分析,用COX回归评估不同时间间隔组患者首次发生脱失的风险。 结果 2004年-2018年在云南省接受ART的110 373例HIV感染者纳入分析,从HIV确诊到启动ART时间中位数47(11,550) d,中位随访2.63(0.88,5.28)年。其中47 974例(43.5%)患者在确诊HIV后30 d内启动ART,15 811例(14.3%)间隔时间在31~90 d,14 253(12.9%)例间隔时间在91~365 d,32 335例(29.3%)间隔时间超过365 d。总脱失率为6.77/100人年(95% CI:6.69~6.85)。以 < 30 d组为参照,30~ d组、91~ d组、>365 d组发生脱失的风险分别提高了10%、22%和14%。 < 30 d组、30~ d组、91~ d组、>365 d组患者治疗1年累计脱失率分别为11.4%、12.7%、15.0%和15.7%。 结论 通过真实世界数据证实:缩短从HIV确诊到启动ART时间间隔(30 d内)可以减少治疗中脱失。研究结果支持“艾滋病检测与治疗一站式服务”作为防治措施实施,并为云南省指导动员治疗咨询提供建议。 Abstract:Objective To analyze the effect of time interval from diagnosis of human immunodeficiency virus (HIV) to initiation of antiretroviral therapy (ART) on the dropout during treatment, and to provide reference for counseling on mobilization of ART. Methods COX regression was used to assess the risk of first dropout in patients with different time intervals. The data of 15- years ART in Yunnan Province were analyzed retrospectively. Results 110 373 cases of ART among people living with HIV in Yunnan from 2004 to 2018 were included in the analysis. the median time from the diagnosis of HIV to the start of ART was 47 (11 550) days, and the median follow-up was 2.63 (0.88, 5.28) years. Out of the total cases, 47 974 (43.5%) patients started ART within 30 days post-HIV-diagnosis, 15 811 (14.3%) patients had an interval of 31-90 days, 14 253 (12.9%) patients had an interval of 91-365 days, and 32 335 (29.3%) patients had an interval above 365 days. The total dropout rate was 6.77/100 person-years (95% CI:6.69-6.85). With the < 30 day group as the reference, the dropout risk in the 30-90 day group, the 91-365 day group and the >365 day group increased by 10%, 22% and 14%, respectively. In the groups of < 30- day, the 30-90 day, the 91-365 day and the >365 day, the cumulative dropout rates were respectively 11.4%, 12.7%, 15.0% and 15.7%. Conclusions Real-world data confirmed that shortening the time interval from HIV diagnosis to ART initiation (preferably within 30 days) can reduce treatment dropout. The results support the implementation of "one-stop AIDS testing and treatment service" as a prevention and treatment measure. This study provides powerful suggestions for Yunnan Province to guide the mobilization of treatment counseling. -
Key words:
- HIV/AIDS /
- Antiretroviral therapy /
- Treatment dropout
-
表 1 云南省不同HIV确诊到启动ART时间间隔病例人口学特征和相关变量情况[n(%)]
Table 1. The demographic characteristics and related variables of different groups at the time interval from HIV diagnosis to ART initiation in Yunnan Province [n(%)]
变量 从HIV确诊到启动ART时间间隔(d) χ2/H值 P值 < 30 30~ 91~ >365 性别 8.2 0.041 男 29 954(62.4) 9 937(62.8) 8 740(61.3) 20 154(62.3) 女 18 020(37.6) 5 874(37.2) 5 513(38.7) 12 181(37.7) 婚姻 71 749.0 < 0.001 未婚 8 539(17.8) 3 115(19.8) 2 920(20.5) 7 249(22.4) 已婚或同居 31 916(66.5) 10 422(65.9) 9 251(64.9) 19 748(61.1) 离异或分居 4 425(9.2) 1 380(8.7) 1 309(9.2) 3 528(10.9) 丧偶 2 986(6.2) 844(5.3) 713(5.0) 1 526(4.7) 不详 108(0.2) 50(0.3) 60(0.4) 284(0.9) 传播途径 11 279.0 < 0.001 同性性传播 2 463(5.1) 635(4.0) 413(2.9) 495(1.5) 异性性传播 39 594(82.6) 1 2056(76.3) 9 899(69.6) 19 309(59.9) 静脉吸毒 3 039(6.3) 2 028(12.8) 2 936(20.6) 1 1052(34.3) 其他 2 828(5.9) 1 077(6.8) 982(6.9) 1 392(4.3) HIV确诊年龄[岁, M(P25,P75)] 39.86(31.25, 50.38) 37.87(30.44, 47.32) 35.46(28.82, 44.01) 31.10(25.86, 37.54) 9 896.1 < 0.001 HIV确诊年龄(岁) 7 983.7 < 0.001 15~ 10 328(21.5) 3 720 (23.5) 4 211(29.5) 14 478(44.8) 31~ 25 295(52.7) 8 850(56.0) 7 877(55.3) 15 743(48.7) >50 12 351(25.7) 3 241 (20.5) 2 164(15.2) 2 114(6.5) ART启动时间(年) 6 488.6 < 0.001 < 2008 2 871(6.0) 1 892(12.0) 2 236(15.7) 2 744(8.5) 2008-2012 8 297(17.3) 4 588(29.0) 4 488(31.5) 10 546(32.6) 2013-2016 22 680(47.3) 6 488 (41.0) 5 459(38.3) 14 483(44.8) >2016 14 126(29.4) 2 843(18.0) 2 070(14.5) 4 562(14.1) 开始ART时CD4计数[个/mm3, M(P25,P75)] 237(122, 357) 222(108, 334) 256(158, 361) 275(173, 386) 1 524.5 < 0.001 开始ART时CD4计数(个/mm3) 1 375.6 < 0.001 0~ 19 728(41.9) 7 011(45.2) 4 914(35.4) 9 832(31.2) 200~ 15 078(32.0) 5 068 (32.6) 5 278(38.0) 12 179(38.7) 350~ 7 351(15.6) 2 034(13.1) 2 092(15.1) 5 450(17.3) >500 4 904(10.4) 1 413(9.1) 1 601(11.5) 4 035(12.8) 随访年[ M(P25,P75)] 2.21(0.75, 4.39) 3.03(0.99, 5.99) 3.22(0.98, 6.41) 3.13(0.99, 5.67) 1 646.3 < 0.001 HIV确诊到启动ART时间间隔[d, M(P25,P75)] 10(5, 17) 48(38, 65) 182(126, 26) 1 260(724, 2 099) 97 988.0 < 0.001 表 2 从HIV确诊到启动ART时间间隔不同组脱失发生率
Table 2. Incidence of dropout in different groups at the time interval from HIV diagnosis to ART initiation
从HIV诊断到启动ART时间间隔(d) 病例数(n) 随访人年 脱失人数 脱失率(人/100人年)(95% CI)值 < 30 47 974 143 342.0 8 667 6.05(5.92~6.17) 30~ 15 811 60 644.8 3 688 6.08(5.89~6.27) 91~ 14 253 57 666.8 4 015 6.96(6.76~7.17) >365 32 335 118 559.0 9 372 7.90(7.75~8.06) 表 3 从HIV确诊到启动ART时间间隔与治疗中脱失的COX回归分析
Table 3. COX regression analysis of the time interval from HIV diagnosis to ART initiation and loss in treatment
变量 单因素HR(95% CI)值 P值 多因素调整HR(95% CI)值 P值 从HIV诊断到启动ART时间间隔(d) < 30 1.00 1.00 30~ 1.14(1.10~1.19) < 0.001 1.10(1.06~1.14) < 0.001 91~ 1.35(1.30~1.40) < 0.001 1.22(1.18~1.27) < 0.001 >365 1.43(1.39~1.47) < 0.001 1.14(1.10~1.18) < 0.001 性别 男 1.00 1.00 女 0.80(0.78~0.83) < 0.001 0.87(0.85~0.90) < 0.001 婚姻 未婚 1.00 1.00 已婚或同居 0.72(0.70~0.74) < 0.001 0.78(0.76~0.81) < 0.001 离异或分居 0.96(0.92~1.00) 0.067 1.00(0.95~1.05) 0.998 丧偶 0.79(0.75~0.84) < 0.001 0.94(0.88~1.00) 0.044 不详 0.92(0.77~1.11) 0.405 0.90(0.74~1.09) 0.293 HIV确诊年龄(岁) 15~ 1.00 1.00 31~ 0.88(0.86~0.91) < 0.001 0.87(0.84~0.89) < 0.001 >50 0.85(0.82~0.88) < 0.001 1.00(0.96~1.05) 0.800 ART启动时间(年) < 2008 1.00 1.00 2008-2012 1.13(1.08~1.18) < 0.001 1.21(1.16~1.27) < 0.001 2013-2016 1.12(1.07~1.16) < 0.001 1.23(1.18~1.29) < 0.001 >2016 0.79(0.75~0.84) < 0.001 0.92(0.86~0.98) 0.008 传播途径 同性性传播 1.00 1.00 异性性传播 1.61(1.47~1.76) < 0.001 2.04(1.85~2.24) < 0.001 静脉吸毒 2.88(2.63~3.16) < 0.001 3.36(3.05~3.70) < 0.001 其他 1.56(1.40~1.73) < 0.001 2.02(1.80~2.25) < 0.001 入组时CD4计数(个/mm3) < 200 1.00 1.00 200~ 1.18(1.15~1.22) < 0.001 1.17(1.13~1.20) < 0.001 351~ 1.14(1.10~1.19) < 0.001 1.17(1.12~1.21) < 0.001 >500 1.26(1.20~1.31) < 0.001 1.29(1.23~1.35) < 0.001 注:11 0373例病例纳入分析,有25 742例发生脱失,观察结局为病例首次发生脱失(定义为《成人随访及用药情况表》随访状态首次由“在治”转为“失访”或“停药”),病例发生死亡或到2018年12月31日前最近1次随访时,该病例以右删失处理。 -
[1] Phanuphak N, Seekaew P, Phanuphak P. Optimising treatment in the test-and-treat strategy: what are we waiting for?[J]. Lancet HIV, 6(10): e715-e722. DOI: 10.1016/s2352-3018(19)30236-x. [2] Sellers CJ, Wohl DA. Antiretroviral Therapy:when to start[J]. Infect Dis Clin North Am, 2014, 28(3):403-420. DOI: 10.1016/j.idc.2014.05.004. [3] Vella S, Schwartländer B, Sow SP, et al. The history of antiretroviral therapy and of its implementation in resource-limited areas of the world[J]. AIDS, 2012, 26(10):1231-1241. DOI: 10.1097/qad.0b013e32835521a3. [4] Department of Health and Human Services. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV[EB/OL]. (2020-08-26)[2020-09-21]. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/AdultandAdolescentGL.pdf [5] World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV[EB/OL]. (2016-06-01)[2019-12-18]. https://apps.who.int/iris/bitstream/handle/10665/208825/9789241549684_eng.pdf;jsessionid=C0113D15A5A7D410E0082E34D7D4D49E?sequence=1. [6] European AIDS Clincal Society. European Guidelines for treatment of HIV infected adults in Europe. Version 9.1[EB/OL]. (2018-10)[2020-01-05]. http://www.eacsociety.org/files/2018_guidelines-9.1-english.pdf. [7] Zhao Y, Wu Z, McGoogan JM, et al. Nationwide cohort study of antiretroviral therapy timing: treatment dropout and virological failure in China, 2011-2015[J]. Clin Infect Dis, 2019, 68(1):43-50. DOI: 10.1093/cid/ciy400. [8] Wu Z, Zhao Y, Ge X, et al. Simplified HIV testing and treatment in China: analysis of mortality rates before and after a structural intervention[J]. PLoS Med, 2015, 12(9):e1001874. DOI: 10.1371/journal.pmed.1001874. [9] Wu Z, Tang Z, Mao Y, et al. Testing and linkage to HIV care in China: a cluster-randomised trial[J]. Lancet HIV, 2017, 4(12):e555-e565. DOI: 10.1016/S2352-3018(17)30131-5. [10] Zhao Y, Wu Z, McGoogan JM, et al. Immediate antiretroviral therapy decreases mortality among patients with high CD4 counts in China: A nationwide, retrospective cohort study[J]. Clin Infect Dis, 2018, 66(5):727-734. DOI: 10.1093/cid/cix878. [11] 蔡英, 李世福, 董文斌, 等.玉溪市红塔区开展艾滋病防治"一站式服务"效果评价[J].中国皮肤性病学杂志, 2018, 32(12):1432-1437. DOI: 10.13735/j.cjdv.1001-7089.201705107.Cai Y, Li SF, Dong WB, et al. The effect evaluation of "one-stop service" for AIDS prevention and treatment in HongTa District, Yuxi[J]. Chin J Dermatovenereol, 2018, 32(12):1432-1437. DOI: 10.13735/j.cjdv.1001-7089.201705107. [12] 夏小亮.艾滋病检测与治疗"一站式服务"工作模式可推广性与可持续性研究[D].北京: 中国疾病预防控制中心, 2017.Xia XL. Replicability and sustainability of HIV/AIDS testing and treatment "one-stop service" model abstract[D]. Beijing: Chinese Center for Disease Control and Prevention, 2017. [13] 杨吟, 白劲松, 冯玲, 等.昆明市官渡区艾滋病检测治疗一站式服务项目效果评估[J].皮肤病与性病, 2017, 39(2):111-113. DOI: 10.3969/j.issn.1002-1310.2017.02.015.Yang Y, Bai JS, Feng L, et al. AIDS testing and treatment one-stop service project effect evaluation in Guan Du District, Kunming[J]. J Dermatol Venereol, 2017, 39(2):111-113. DOI: 10.3969/j.issn.1002-1310.2017.02.015. [14] 姬尔高, 王学敏, 刘礼荣, 等.新疆伊宁市艾滋病抗病毒治疗"一站式"工作模式效果分析[J].中国艾滋病性病, 2016, 22(2):95-98. DOI: 10.13419/j.cnki.aids.2016.02.10.Ji EG, Wang XL, Liu LR, et al. Effect analysis of HIV/AIDS treatment after practice of "one-stop service" in Yining, Xinjiang[J]. Chin J AIDS STD, 2016, 22(2):95-98. DOI: 10.13419/j.cnki.aids.2016.02.10. [15] 国务院办公厅.中国遏制与防治艾滋病"十三五"行动计划[EB/OL]. (2017-02-05)[2020-01-05]. http://www.gov.cn/zhengce/content/2017-02/05/content_5165514.htm.General Office of the State Council. China's 13th five-year action plan for the prevention and treatment of AIDS[EB/OL]. (2017-02-05)[2020-01-05]. http://www.gov.cn/zhengce/content/2017-02/05/content_5165514.htm. [16] Rosen S, Maskew M, Fox MP, et al. Initiating antiretroviral therapy for hiv at a patient's first clinic visit: The RapIT randomized controlled trial[J]. PLoS Med, 2016, 13(5):e1002015. DOI: 10.1371/journal.pmed.1002015. [17] Rosen S, Maskew M, Larson BA, et al. Simplified clinical algorithm for identifying patients eligible for same-day HIV treatment initiation (SLATE): Results from an individually randomized trial in South Africa and Kenya[J]. PLoS Med, 2019, 16(9):e1002912. DOI: 10.1371/journal.pmed.1002912. [18] Ford N, Migone C, Calmy A, et al. Benefits and risks of rapid initiation of antiretroviral therapy:a systematic review and meta-analysis[J]. AIDS, 2018, 32(1):17-23. DOI: 10.1097/QAD.0000000000001671. [19] Koenig SP, Dorvil N, Dévieux JG, et al. Same-day HIV testing with initiation of antiretroviral therapy versus standard care for persons living with HIV: A randomized unblinded trial[J]. PLoS Med, 2017, 14(7):e1002357. DOI: 10.1371/journal.pmed.1002357. [20] 中国疾病预防控制中心性病艾滋病预防控制中心.国家免费艾滋病抗病毒药物治疗手册[M].北京:人民卫生出版社, 2016.The Chinese center for disease control and prevention sexually transmitted disease of AIDS prevention and control center. National handbook of free antiviral therapy for AIDS[M]. Beijing: People's Medical Publishing House, 2016. [21] 安靓, 劳云飞, 楼金成, 等. 2016年云南省艾滋病抗病毒治疗人力现状及需要量分析[J].中国艾滋病性病, 2018, 24(10):1043-1046. DOI: 10.13419/j.cnki.aids.2018.10.22.An J, Lao YF, Lou JC, et al. Status of human resource and demand for HIV antiretroviral therapy program in Yunnan Province[J]. Chin J AIDS STD, 2018, 24(10):1043-1046. DOI: 10.13419/j.cnki.aids.2018.10.22. [22] 劳云飞.云南省艾滋病抗病毒治疗质量控制手册[M].云南:云南科技出版社, 2018.Lao YF. Yunnan Province manual of Quality Control of antiretroviral therapy for AIDS[M]. Yunnan:Yunnan Science and Technology Press, 2018. -





 下载:
下载: