A case-control study on risk factors for atrial fibrillation among people over 50 years old in a community in Nanjing
-
摘要:
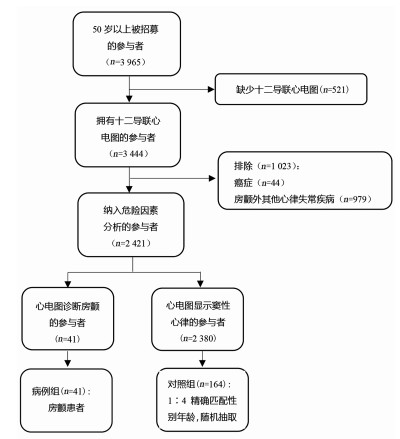
目的 探讨江苏南京某社区≥50岁人群发生心房颤动的危险因素。 方法 2019年3月1日至4月30日,对南京市栖霞区某社区医院进行健康检查的社区老年人群开展流行病学现况调查,经12导联心电图诊断后的房颤患者为病例组,按照年龄、性别进行1:4频数匹配后的非房颤人群作为对照组。采用单因素和多因素条件Logisitc回归分析模型分析心房颤动可能的危险因素。 结果 共调查3 444名社区老人,男女性别比为1:2,房颤检出率为1.19%。单因素条件Logistic回归分析模型分析结果提示:血尿酸(OR=1.01, 95% CI: 1.00~1.01)、红细胞比容(OR=1.11, 95% CI: 1.01~1.23)、红细胞分布宽度(OR=1.50, 95% CI: 1.05~2.14)可能是房颤的危险因素。多因素条件Logistic回归分析模型分析结果显示:红细胞比容每升高1%,个体发生房颤的风险增加13%(OR=1.13, 95% CI: 1.01~1.27);红细胞分布宽度每升高1%,个体发生房颤的风险可能增加61%(OR=1.61, 95% CI: 1.00~2.59)。 结论 红细胞比容、红细胞分布宽度增加可能是南京社区老年人群房颤发生的可疑危险因素。本研究的结论需要进一步扩大样本验证。 Abstract:Objective To explore the risk factors of atrial fibrillation (AF) in people aged 50 years and above in Nanjing, Jiangsu Province. Methods An epidemiological survey was conducted among the elderly in a community healthcare center in Qixia District from March 1, 2019 to April 30, 2019. The case group was defined as patients with AF diagnosed by 12-lead electrocardiogram (ECG), and the controls were a non-AF population matched by age and sex, with a matching ratio of 1:4. Univariate and multivariate conditional Logistic regression analysis model were used to analyse possible influencing factors. Results A total of 3 444 cases were investigated. The ratio of male to female is 1:2, and the detection rate of AF was 1.19%. The univariate Logistic regression analysis indicated that serum uric acid (OR=1.01, 95% CI: 1.00-1.01), hematocrit (HCT, OR=1.11, 95% CI: 1.01-1.23) and red blood cell distribution width (RDW, OR=1.50, 95% CI: 1.05-2.14) might be risk factors for AF. The multivariate Logistic regression analysis model results showed that each increase of 1% in HCT and RDW was associated with a 13% (OR=1.13, 95% CI: 1.01-1.27) and 61% (OR=1.61, 95% CI: 1.00-2.59) increased risk of AF respectively. Conclusions HCT and RDW may be independent risk factors for atrial fibrillation in the elderly in Nanjing community. In addition, the results of this study need to be further verified due to the limited sample size. -
Key words:
- Atrial fibrillation /
- Risk factors /
- Older-people /
- Case-control study
-
表 1 南京市栖霞区2019年房颤组与对照组计量指标比较(x ±s)
Table 1. Comparison between the atrial fibrillation group and the control group of measurement indicators in Qixia District, Nanjing in 2019 (x ±s)
变量 房颤组(n=41) 对照组(n=164) OR(95% CI)值 P值 BMI (kg/m2) 25.0±2.8 25.0±3.2 1.00(0.91~1.11) 0.965 SBP (mm Hg) 137.4±15.7 141.6±14.2 0.98(0.96~1.01) 0.143 DBP (mm Hg) 85.0±11.4 85.7±8.4 0.99(0.95~1.03) 0.664 LDL-C (mmol/L) 2.2±0.8 2.6±0.7 0.51(0.32~0.82) 0.005 HDL-C (mmol/L) 1.2±0.3 1.3±0.3 0.32(0.10~1.08) 0.066 TC (mmol/L) 4.5±1.2 5.1±1.0 0.62(0.45~0.86) 0.004 总胆红素(μmol/L) 16.5±4.7 14.7±5.7 1.06(0.99~1.12) 0.064 血尿酸(μmol/L) 353.3±92.2 320.1±76.9 1.01(1.00~1.01) 0.020 血尿素氮(mmol/L) 6.5±4.0 5.8±1.8 1.12(0.97~1.29) 0.113 红细胞比容(%) 43.9±5.6 42.6±4.0 1.11(1.01~1.23) 0.039 红细胞分布宽度(%) 11.7±1.1 11.3±0.9 1.50(1.05~2.14) 0.026 表 2 2019年南京市栖霞区房颤组组与对照组有关健康状态的比较[n(%)]
Table 2. Comparison of health status between atrial fibrillation group and control group in Qixia District, Nanjing in 2019 [n(%)]
变量 房颤组(n=41) 对照组(n=164) OR(95% CI)值 P值 中心性肥胖 无 11(26.8) 65(39.6) 1.00 有 30(73.2) 99(60.4) 1.47(0.70~3.11) 0.310 高血压 无 12(29.3) 54(32.9) 1.00 有 29(70.7) 110(67.1) 0.79(0.36~1.74) 0.560 糖尿病 无 31(75.6) 121(73.8) 1.00 有 10(24.4) 43(26.2) 1.15(0.51~2.57) 0.737 高尿酸血症 无 30(73.2) 143(87.2) 1.00 有 11(26.8) 21(12.8) 2.14(0.92~4.98) 0.107 高脂肪酸血症 无 27(65.9) 108(65.9) 1.00 有 14(34.1) 56(34.1) 1.00(0.49~2.06) 1.000 表 3 2019年南京市栖霞区房颤危险因素的多因素Logistic回归分析模型分析
Table 3. Multivariate Logistic regression analysis model analysis of the risk factors for atrial fibrillation in Qixia District, Nanjing in 2019
变量 β值 sx Wald χ2值 AOR(95% CI)值 P值 HDL-C (mmol/L) -1.08 0.69 1.84 0.34(0.09~1.32) 0.119 LDL-C (mmol/L) -0.73 0.46 3.21 0.48(0.20~1.15) 0.100 TC (mmol/L) 0.04 0.32 0.02 1.04(0.57~1.91) 0.890 总胆红素(μmol/L) 0.04 0.03 0.73 1.04(0.97~1.11) 0.325 血尿酸(μmol/L) 0.00 0.003 0.06 1.00(0.99~1.01) 0.711 红细胞比容(%) 0.12 0.05 3.20 1.13(1.01~1.27) 0.032 红细胞分布宽度(%) 0.48 0.23 5.08 1.61(1.00~2.59) 0.048 -
[1] Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study[J]. Lancet, 2015, 386(9989):154-162. DOI: 10.1016/S0140-6736(14)61774-8. [2] Wang Z, Chen Z, Wang X, et al. The disease burden of atrial fibrillation in China from a national cross-sectional survey[J]. Am J Cardiol, 2018, 122(5):793-798. DOI: 10.1016/j.amjcard.2018.05.015. [3] Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: A global burden of disease 2010 study[J]. Circulation, 2014, 129(8):837-847. DOI: 10.1161/CIRCULATIONAHA.113.005119. [4] January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart rhythm society[J]. J Am Coll Cardiol, 2019, 74(1):104-132. DOI: 10.1016/j.jacc.2019.01.011. [5] 黄从新, 张澍, 黄德嘉, 等.心房颤动:目前的认识和治疗建议-2018[J].中国心脏起搏与心电生理, 2018, 32(4):315-368. DOI: 10.13333/j.cnki.cjcpe.2018.04.001.Huang CX, Zhang S, Huang DJ, et al. Current knowledge and management recommendations of atrial fibrillation-2018[J]. Chinese Journal of Cardiac Pacing and Electrophysiology, 2018, 32(4):315-368. DOI: 10.13333/j.cnki.cjcpe.2018.04.001. [6] Turakhia MP, Shafrin J, Bognar K, et al. Estimated prevalence of undiagnosed atrial fibrillation in the United States[J]. PLoS ONE, 2018, 13(4):e0195088. DOI: 10.1371/journal.pone.0195088. [7] Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomized controlled trials, and Mendelian randomization studies[J]. BMJ, 2017, 358: j3799. DOI: 10.1136/bmj.j3799. [8] Hong M, Park JW, Yang PS, et al. A mendelian randomization analysis: The causal association between serum uric acid and atrial fibrillation[J]. Eur J Clin Invest, 2020, 50(10):e13300. DOI: 10.1111/eci.13300. [9] Bae JC, Rhee EJ, Lee WY, et al. Combined effect of nonalcoholic fatty liver disease and impaired fasting glucose on the development of type 2 diabetes: a 4-year retrospective longitudinal study[J]. Diabetes Care, 2011, 34(3):727-729. DOI: 10.2337/dc10-1991. [10] Shibata M, Kihara Y, Taguchi M, et al. Nonalcoholic fatty liver disease is a risk factor for type 2 diabetes in middle-aged Japanese men[J]. Diabetes Care, 2007, 30(11):2940-2944. DOI: 10.2337/dc07-0792. [11] Fan JG, Li F, Cai XB, et al. Effects of nonalcoholic fatty liver disease on the development of metabolic disorders[J]. J Gastroenterol Hepatol, 2007, 22(7):1086-1091. DOI: 10.1111/j.1440-1746.2006.04781.x. [12] Watanabe H, Tanabe N, Yagihara N, et al. Association between lipid profile and risk of atrial fibrillation[J]. Circ J, 2011, 75(12):2767-2774. DOI: 10.1253/circj.cj-11-0780. [13] 刘洪梅, 邵清淼, 缪帅, 等.非瓣膜性心房颤动患者红细胞分布宽度与CHADS2、CHA2DS2-VASc评分的关系[J].临床心血管病杂志, 2014, 3(30):207-210. DOI: 10.13201/j.issn.1001-1439.2014.03.009.Liu HM, Shao QM, Miao S, et al. The relationship of red blood cell distribution width and CHADS2/CHA2DS2-VASc score in non-valvular atrial fibrillation parents[J]. J Clin Cardiol (China), 2014, 3(30):207-210. DOI: 10.13201/j.issn.1001-1439.2014.03.009. [14] Kurt M, Tanboga IH, Buyukkaya E, et al. Relation of red cell distribution width with CHA2DS2-VASc score in patients with nonvalvular atrial fibrillation[J]. Clin Appl Thromb Hemost, 2013, 20(7):687-692. DOI: 10.1177/1076029613478157. [15] 梁荻, 于胜波, 赵庆彦, 等.慢性心力衰竭患者红细胞压积与心房颤动类型的相关性研究[J].微循环学杂志, 2011, 21(2):50-52. DOI: 10.3969/j.issn.1005-1740.2011.02.019.Liang D, Yu SB, Zhao QY, et al. Correlation between hematocrit and the pattern of atrial fibrillation in patients with chronic heart failure[J]. Chin J Microcirc, 2011, 21(2):50-52. DOI: 10.3969/j.issn.1005-1740.2011.02.019. [16] 朱增民.红细胞压积对全血黏度关系的影响研究[J].当代医学, 2011, 17(29):20-21. DOI: 10.3969/j.issn.1009-4393.2011.29.011.Zhu ZM. Study on the influence of hematocrit on the relationship of whole blood viscosity[J]. Contemporary Medicine, 2011, 17(29):20-21. DOI: 10.3969/j.issn.1009-4393.2011.29.011. [17] Li H, Gu Y, Liu M, et al. The relationship between red blood cell distribution width and atrial fibrillation in Asian population: A cross-sectional study[J]. Pacing Clin Electrophysio, 2019, 42(9):1197-1203. DOI: 10.1111/pace.13776. [18] Shao QM, Korantzopoulos P, Letsas KP, et al. Red blood cell distribution width as a predictor of atrial fibrillation[J]. J Clin Lab Anal, 2018, 32(5):1-8. DOI: 10.1002/jcla.22378. [19] Hu YF, Chen YJ, Lin YJ, et al. Inflammation and the pathogenesis of atrial fibrillation[J]. Nat Rev Cardiol, 2015, 12(4):230. DOI: 10.1038/nrcardio. [20] Montagnana M, Cervellin G, Meschi T, et al. The role of red blood cell distribution width in cardiovascular and thrombotic disorders[J]. Clin Chem Lab Med, 2012, 50(4):635-641. DOI: 10.1515/cclm.2011.831. [21] 李苏宁, 陈柞, 王增武, 等.我国老年人高血压现状分析[J].中华高血压杂志, 2019, 27(2):140-150. DOI: 10.16439/j.cnki.1673-7245.2019.02.002.Li SN, Chen Z, Wang ZW, et al. The hypertension status of the elder population in China[J]. Chin J Hypertens, 2019, 27(2):140-150. DOI: 10.16439/j.cnki.1673-7245.2019.02.002. [22] 中华医学会糖尿病学分会.中国2型糖尿病防治指南(2017年版)[J].中国实用内科杂志, 2018, 38(4):292-344. DOI: 10.19538/j.nk2018040108.Chinese Diabetes Society. Guidelines for the prevention and control of type 2 diabetes in China (2017 Edition)[J]. Chin J Pract Intern Med, 2018, 38(4):292-344. DOI: 10.19538/j.nk2018040108. -





 下载:
下载: