Association and dose-response relationship of physical activity and sedentary behavior with risk of premature rupture of membranes
-
摘要:
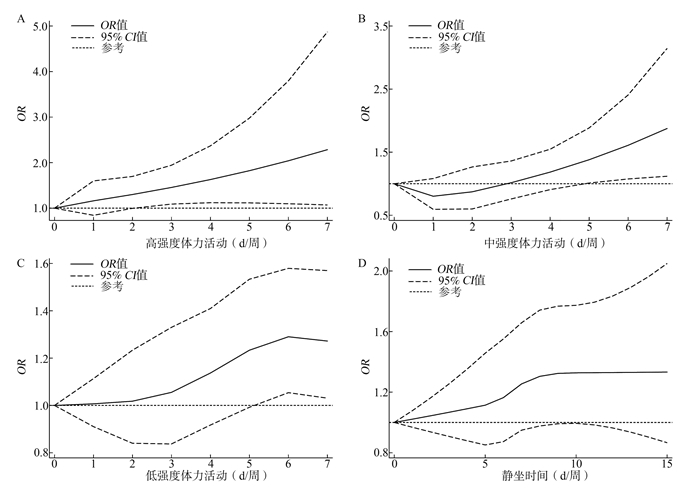
目的 探究孕期妇女体力活动(physical activity, PA)、久坐行为与胎膜早破(premature rupture of membranes, PROM)发生风险的相关性及剂量反应关系。 方法 采用国际体力活动短问卷收集中国孕产妇队列研究·协和项目中孕妇的体力活动状况和静坐时间(sedentary time, ST),并随访收集研究对象PROM的诊断情况,采用Logistic回归分析模型和限制性立方样条模型进行数据分析,计算OR及95% CI值。 结果 共纳入研究对象6 848例。孕妇PROM的发生率为13.79%。在中/低强度PA方面,与低频组相比,高频组PROM的发生风险更高(中强度OR=1.50, 95% CI: 1.01~2.23;低强度OR=1.19, 95% CI: 1.04~1.73);高强度PA频次每增加1 d/week,PROM发生风险增加13%(OR=1.13, 95% CI: 1.03~1.24);ST每增加1 h/d,PROM发生风险增加2%(OR=1.02, 95% CI: 1.01~1.04)。剂量反应关系显示,高强度PA超过2 d/周,中强度超过5 d/周或低强度超过5 d/周均可增加PROM的发生风险(OR及95% CI均>1)。 结论 孕期高频体力活动和久坐行为是胎膜早破发生的危险因素,应鼓励孕妇进行适宜和中低强度体力活动的同时,减少静坐时间,以降低胎膜早破的发生风险。 Abstract:Objective To investigate the association and dose-response relationship of physical activity (PA) and sedentary behavior with premature rupture of membranes (PROM). Methods Data were collected from the Chinese Pregnant Women Cohort Study. The International Physical Activity Questionnaire-Short Form was used to assess the frequency of PA and sedentary time (ST), and diagnosis of PROM was collected in the follow-up period. Logistic regression analysis model and restricted cubic spline (RCS) model were used for data analyses. The odds ratio (OR) with its 95% confidence interval (CI) was calculated. Results A total of 6 848 participants were included in this study. The incidence of PROM was 13.79% among pregnant women. Compared with low frequency group, women with high frequencies of moderate-intensity PA (OR=1.50, 95% CI: 1.01-2.23) and light-intensity PA (OR=1.19, 95% CI: 1.04-1.37) had higher risks of PROM respectively. The risk of PROM increased 13% (OR=1.13, 95% CI: 1.03-1.24) per 1 d/week increase of vigorous-intensity PA, while the risk increased 2% (OR=1.02, 95% CI: 1.01-1.04) per 1 h/d increase of ST. The RCS model showed that the risk for PROM was significant with frequencies of over 2 d/week of vigorous-intensity PA, over 5 d/week of moderate-intensity PA or over 5 d/week of light-intensity PA (all ORs with corresponding 95% CIs>1). Conclusions High frequency of physical activity and sedentary behavior are risk factors for PROM. Pregnant women are supposed to conduct physical activity with proper frequency and moderate intensity as well as decreasing sedentary time, so as to prevent the risk of PROM during pregnancy. -
表 1 6 848名研究对象的基本特征[n(%)]
Table 1. Demographic characteristics of 6 848 participants [n(%)]
基线特征 总例数 胎膜早破 χ2值 P值 Ptrend值 是(n=944) 否(n=5 904) 年龄组(岁) 14.85 0.002 0.395 <25 1 003(14.65) 104(11.02) 899(15.23) 25~ 3 360(49.07) 506(53.60) 2 854(48.34) 30~ 1 815(26.50) 247(26.16) 1 568(26.56) ≥35 670(9.78) 87(9.22) 583(9.97) 孕前BMI(kg/m2) 4.72 0.194 0.093 <18.5 902(13.17) 128(13.56) 774(13.11) 18.5~ 4 372(63.84) 616(65.25) 3 756(63.62) 24.0~ 1 242(18.14) 167(17.69) 1 075(18.21) ≥28.0 332(4.85) 33(3.50) 299(5.06) 民族 0.79 0.373 汉族 6 457(94.29) 896(94.92) 5 561(94.19) 少数民族 391(5.71) 48(5.08) 343(5.81) 户口类型 20.85 <0.001 城镇 3 192(46.61) 505(53.50) 2 687(45.51) 农村 3 656(53.39) 439(46.50) 3 217(54.49) SES 30.13 <0.001 <0.001 低 2 048(29.91) 219(23.20) 1 829(30.98) 中 2 342(34.20) 323(34.22) 2 019(34.20) 高 2 458(35.89) 402(42.58) 2 056(34.82) 地区划分1 1.79 0.181 北方 3 736(54.56) 534(56.57) 3 202(54.23) 南方 3 112(45.44) 410(43.43) 2 702(45.77) 地区划分2 26.76 <0.001 0.208 东部 2 599(37.95) 377(39.94) 2 222(37.64) 中部 2 388(34.87) 263(27.86) 2 125(35.99) 西部 1 861(27.18) 304(32.20) 1 557(26.37) 表 2 体力活动与胎膜早破发生风险的相关性[n(%)]
Table 2. Association between physical activities and risk of premature rupture of membranes [n(%)]
体力活动类型 总例数 胎膜早破 例数 粗OR(95% CI)值 调整OR(95% CI)值 高强度 低频组 6 784(99.07) 932(98.73) 1.00 1.00 高频组 64(0.93) 12(1.27) 1.45(0.77~2.73) 1.57(0.83~2.97) 中强度 低频组 6 688(97.66) 913(96.72) 1.00 1.00 高频组 160(2.34) 31(3.28) 1.52(1.02~2.26) 1.50(1.01~2.23) 低强度 低频组 3 800(55.49) 483(51.17) 1.00 1.00 高频组 3 048(44.51) 461(48.83) 1.22(1.07~1.40) 1.19(1.04~1.37) 久坐组 否 5 094(74.39) 676(71.61) 1.00 1.00 是 1 754(25.61) 268(28.39) 1.18(1.01~1.37) 1.12(0.96~1.31) -
[1] Committee on Practice Bulletins-Obstetrics. Acog practice bulletin no. 188: prelabor rupture of membranes[J]. Obstet Gynecol, 2018, 131(1):e1-e14. DOI: 10.1097/AOG.0000000000002455. [2] Ramsauer B, Vidaeff AC, Hosli I, et al. The diagnosis of rupture of fetal membranes (rom): a meta-analysis[J]. J Perinat Med, 2013, 41(3):233-240. DOI: 10.1515/jpm-2012-0247. [3] Ananth CV, Oyelese Y, Srinivas N, et al. Preterm premature rupture of membranes, intrauterine infection, and oligohydramnios: risk factors for placental abruption[J]. Obstet Gynecol, 2004, 104(1):71-77. DOI: 10.1097/01.AOG.0000128172.71408.a0. [4] Goldenberg RL, Culhane JF, Iams JD, et al. Epidemiology and causes of preterm birth[J]. Lancet, 2008, 371(9606):75-84. DOI: 10.1016/S0140-6736(08)60074-4. [5] Locatelli A, Ghidini A, Paterlini G, et al. Gestational age at preterm premature rupture of membranes: a risk factor for neonatal white matter damage[J]. Am J Obstet Gynecol, 2005, 193(3 Pt 2):947-951. DOI: 10.1016/j.ajog.2005.06.039. [6] Sharp GC, Stock SJ, Norman JE. Fetal assessment methods for improving neonatal and maternal outcomes in preterm prelabour rupture of membranes[J]. Cochrane Database Syst Rev, 2014, (10):CD010209. DOI: 10.1002/14651858.CD010209.pub2. [7] Assefa NE, Berhe H, Girma F, et al. Risk factors of premature rupture of membranes in public hospitals at mekele city, tigray, a case control study[J]. BMC Pregnancy Childbirth, 2018, 18(1):386. DOI: 10.1186/s12884-018-2016-6. [8] Hassanzadeh A, Paknahad Z, Khoigani MG. The relationship between macro- and micro-nutrients intake and risk of preterm premature rupture of membranes in pregnant women of isfahan[J]. Adv Biomed Res, 2016, 5:155. DOI: 10.4103/2277-9175.188949. [9] Acog committee opinion no. 650: physical activity and exercise during pregnancy and the postpartum period[J]. Obstet Gynecol, 2015, 126(6):e135-e142. DOI: 10.1097/AOG.0000000000001214. [10] Wang YW, Ma HH, Feng YH, et al. Association among pre-pregnancy body mass index, gestational weight gain and neonatal birth weight: a prospective cohort study in china[J]. BMC Pregnancy Childbirth, 2020, 20(1):690. DOI: 10.1186/s12884-020-03323-x. [11] Zhan YL, Ma HH, Feng YH, et al. Dietary patterns in relation to gestational depression and sleep disturbance in chinese pregnant women[J]. J Obstet Gynaecol Res, 2020, 46(12):2618-2628. DOI: 10.1111/jog.14508. [12] 岳和欣, 冯雅慧, 湛永乐, 等.孕期环境暴露对早产和低出生体重影响的队列研究[J].中华疾病控制杂志, 2020, 24(11):1246-1251. DOI: 10.16462/j.cnki.zhjbkz.2020.11.002.Yue HX, Feng YH, Zhan YL, et al. Effects of environmental exposure during pregnancy on preterm birth and low birth weight: a cohort study[J]. Chin J Dis Control Prev, 2020, 24(11):1246-1251. DOI: 10.16462/j.cnki.zhjbkz.2020.11.002. [13] Deng HB, Macfarlane DJ, Thomas GN, et al. Reliability and validity of the ipaq-chinese: the Guangzhou biobank cohort study[J]. Med Sci Sports Exerc, 2008, 40(2):303-307. DOI: 10.1249/mss.0b013e31815b0db5. [14] 屈宁宁, 李可基.国际体力活动问卷中文版的信度和效度研究[J].中华流行病学杂志, 2004, 25(3):265-268.Qu NN, Li KJ. Study on the reliability and validity of international physical activity questionnaire (Chinese Vision, IPAQ)[J]. Chin J Epidemiol, 2004, 25(3):265-268. [15] 冯雅慧, 吕嬿, 马帅, 等.孕早期妇女体力活动现状及影响因素分析[J].中华护理杂志, 2019, 54(8):1200-1204. DOI: 10.3761/j.issn.0254-1769.2019.Feng YH, Lyu Y, Ma S, et al. The status and influencing factors of physical activity among early pregnancy women[J]. Chin J Nurs, 2019, 54(8):1200-1204. DOI: 10.3761/j.issn.0254-1769.2019. [16] 中华人民共和国国家卫生和计划生育委员会. WS/T 428-2013成人体重判定[S].北京: 中国标准出版社, 2013National Health and Family Planning Commission of the People's Republic of China. Health industry standard: Criteria of weight for adults[S]. Beijing: Chinese Standards Press, 2013. [17] Green LW. Manual for scoring socioeconomic status for research on health behavior[J]. Public Health Rep, 1970, 85(9):815-827. DOI: 10.2307/4593972. [18] 湛永乐, 石英杰, 陈云利, 等.孕育史对孕期抑郁影响的前瞻性队列研究[J].中华疾病控制杂志, 2020, 24 (3):324-329. DOI: 10.16462/j.cnki.zhjbkz.2020.03.015.Zhan YL, Shi YJ, Chen YL, et al. Influence of reproduction history on depression during pregnancy: a prospective cohort study[J]. Chin J Dis Control Prev, 2020, 24(3):324-329. DOI: 10.16462/j.cnki.zhjbkz.2020.03.015. [19] Lederman RP. Relationship of anxiety, stress, and psychosocial development to reproductive health[J]. Behav Med, 1995, 21(3):101-112. DOI: 10.1080/08964289.1995.9933748. [20] Mozurkewich EL, Luke B, Avni M, et al. Working conditions and adverse pregnancy outcome: a meta-analysis[J]. Obstet Gynecol, 2000, 95(4):623-635. DOI: 10.1016/s0029-7844(99)00598-0. [21] Takami M, Tsuchida A, Takamori A, et al. Effects of physical activity during pregnancy on preterm delivery and mode of delivery: the japan environment and children's study, birth cohort study[J]. PLoS One, 2018, 13(10):e0206160. DOI: 10.1371/journal.pone.0206160. [22] 冯雅慧, 湛永乐, 吕嬿, 等.孕早期体力活动与妊娠期糖尿病关系的队列研究[J].中华流行病学杂志, 2020, 41(6):829-833. DOI: 10.3760/cma.j.cn112338-20190914-00671.Feng YH, Zhan YL, Lyu Y, et al. Associations of physical activity in gestational diabetes mellitus in the first trimester of pregnancy[J]. Chin J Epidemiol, 2020, 41(6):829-833. DOI: 10.3760/cma.j.cn112338-20190914-00671. [23] 冯雅慧, 石英杰, 王雅文, 等.孕中期身体活动与剖宫产关系的队列研究[J].中华疾病控制杂志, 2020, 24 (3):319-323, 329. DOI:10.16462 /j.cnki.zhjbkz.2020.03.014.Feng YH, Shi YJ, Wang YW, et al. Association of physical activity and cesarean section in second trimester of pregnancy: a cohort study[J]. Chin J Dis Control Prev, 2020, 24(3):319-323. DOI:10.16462 /j.cnki.zhjbkz.2020.03.014. [24] 岳和欣, 冯雅慧, 吴散散, 等.孕期妇女体力活动变化对抑郁影响的队列研究[J].中华流行病学杂志, 2020, 41(6):834-838. DOI:103760/cma.j.cn112338-20200118-00043.Yue HY, Feng YH, Wu SS, et al. Effects of changes in physical activities on depressive symptoms during pregnancy: a cohort study[J]. Chin J Epidemiol, 2020, 41(6):834-838. DOI:103760/cma.j.cn112338-20200118-00043. [25] Catov JM, Parker CB, Gibbs BB, et al. Patterns of leisure-time physical activity across pregnancy and adverse pregnancy outcomes[J]. Int J Behav Nutr Phys Act, 2018, 15(1):68. DOI: 10.1186/s12966-018-0701-5. [26] Aune D, Schlesinger S, Henriksen T, et al. Physical activity and the risk of preterm birth: a systematic review and meta-analysis of epidemiological studies[J]. BJOG, 2017, 124(12):1816-1826. DOI: 10.1111/1471-0528.14672. [27] Fazzi C, Saunders DH, Linton K, et al. Sedentary behaviours during pregnancy: a systematic review[J]. Int J Behav Nutr Phys Act, 2017, 14(1):32. DOI: 10.1186/s12966-017-0485-z. [28] de Rezende LF, Rodrigues Lopes M, Rey-Lopez JP, et al. Sedentary behavior and health outcomes: an overview of systematic reviews[J]. PLoS One, 2014, 9(8):e105620. DOI: 10.1371/journal.pone.0105620. -





 下载:
下载: