Interaction between family history of diabetes and dyslipidemia on risk of diabetes
-
摘要:
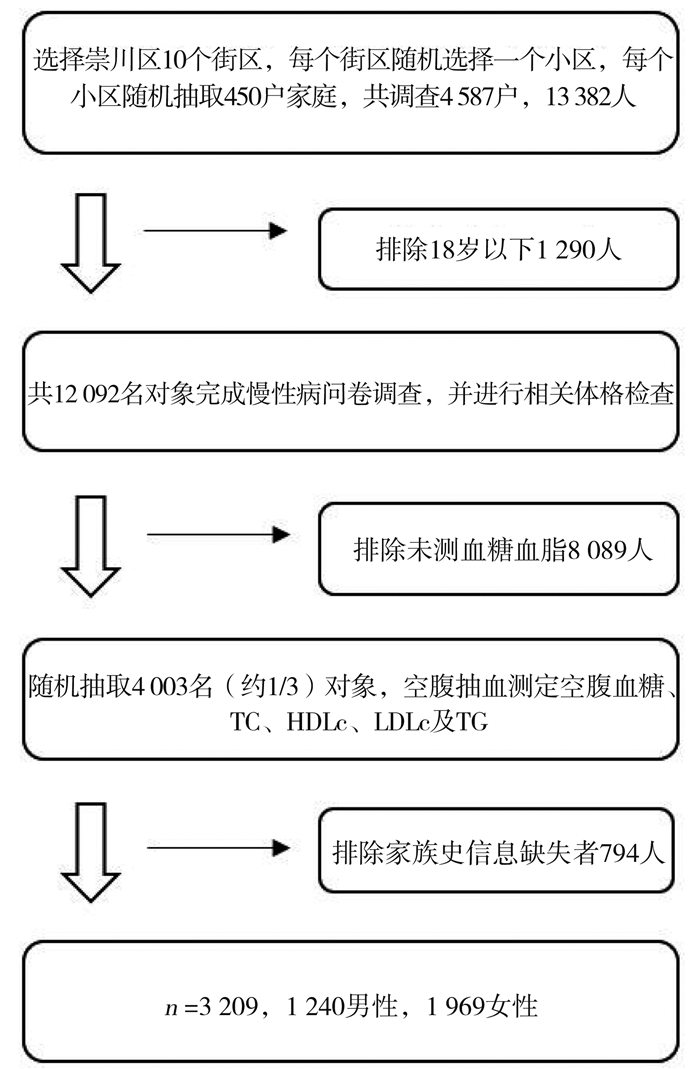
目的 探讨糖尿病家族史与血脂异常对糖尿病患病风险的交互作用。 方法 利用2018年江苏省南通市崇川区“国家慢性病综合防控示范区建设”项目调查的13 382名居民数据,其中血糖信息获得3 209份。Logistic回归模型分析糖尿病家族史、血脂异常与糖尿病患病的关系,使用相加模型评估二者交互作用对糖尿病患病风险的影响,并探讨二者交互作用的性别差异。 结果 本研究糖尿病患病率17.3%,标化患病率12.9%,糖尿病阳性家族史占8.8%,血脂异常者占7.6%。调整年龄、吸烟、饮酒及高脂饮食等混杂因素后,糖尿病家族史与血脂异常对糖尿病患病风险存在协同作用,家族史和血脂异常共同存在时,男、女性人群患病风险分别是二者均不存在者的15.24倍(95% CI:4.57~50.82)和9.84倍(95% CI:4.58~21.12)。男性相对超危险度比(the relative excess risk due to interaction, RERI)为6.59,归因交互作用(the attributable proportion due to interaction, AP)为43.2%,交互作用指数(the synergy index, S)为1.86,纯因子归因交互作用百分比AP%×(AB)为46.3%;女性RERI为4.22,AP%为42.9%,S为1.91,AP×(AB)%为47.7%。 结论 糖尿病家族史和血脂异常对糖尿病患病风险存在协同作用,且男性人群的交互作用可能大于女性。 Abstract:Objective To explore the interaction between family history of diabetes and dyslipidemia on the risk of diabetes. Methods Based on the data of 13 382 residents surveyed by the project "National Demonstration Zone for Comprehensive Prevention and Control of Chronic Diseases" in Chongchuan District, Nantong City, Jiangsu Province in 2018, 3 209 blood glucose information were obtained. Logistic regression analysis was utilized to analyze the correlation of family history and dyslipidemia on the risk of diabetes, and an additive model was conducted to evaluate the impact of their interaction effect on diabetes. The gender difference of their interaction was also explored. Results The prevalence of diabetes was 17.3%, the standardized prevalence was 12.9%. The proportion of individuals who had family history and dyslipidemia was 8.8% and 7.6% respectively. After adjusting confounding factors such as age, smoking, alcohol consumption and high fat diet, it showed that family history and dyslipidemia had synergistic effects on the risk of diabetes. When family history and dyslipidemia existed concurrently, the risk of diabetes for males and females was 15.24 times (95% CI: 4.57-50.82) and 9.84 times (95% CI: 4.58-21.12) higher than normal. In male, the RERI, AP%, S, AP×(AB)% was 6.59, 43.2%, 1.86 and 46.3% respectively; In female, the RERI, AP%, S, AP×(AB)% was 4.22, 42.9%, 1.91, and 47.7% respectively. Conclusions Family history of diabetes and dyslipidemia has synergistic impact on risk of diabetes, and the interaction effect among males may be stronger than females. -
Key words:
- Diabetes mellitus /
- Family history /
- Dyslipidemia /
- Interaction
-
表 1 研究人群基本特征[(x±s)或n(%)]
Table 1. Sociodemographic characteristics of the participants [(x±s) or n(%)]
变量 未患病(n=2 653) 患糖尿病(n=556) t/χ2值 P值 年龄(岁) 62.8±13.8 69.4±9.0 10.7 < 0.001 SBP (mm Hg) 132.3±14.1 138.9±15.4 9.9 < 0.001 DBP (mm Hg) 80.5±7.8 81.6±8.2 2.9 < 0.001 BMI (kg/m2) 消瘦/正常(<24) 1 383 (85.6) 232 (14.4) 32.8 < 0.001 超重(24~) 1 037 (81.4) 237 (18.6) 肥胖(≥28) 233 (72.8) 87 (27.2) 性别 11.3 < 0.001 男 990 (79.8) 250 (20.2) 女 1 663 (84.5) 306 (15.5) 文化程度 44.1 < 0.001 小学及以下 836 (77.6) 241 (22.4) 初中 881 (83.1) 179 (16.9) 高中/中专 556 (84.6) 101 (15.4) 大专及以上 380(91.6) 35 (8.4) 婚姻状况 14.6 < 0.001 未婚 50 (98.0) 1 (2.0) 已婚 2 349 (82.9) 485 (17.1) 离异/丧偶 254 (78.4) 70 (21.6) 职业 28.4 < 0.001 学生 6 (100.0) 0 (0.0) 私营业主 127 (94.8) 7 (5.2) 政府/事业单位人员 57 (87.7) 8 (12.3) 一般员工 859 (85.2) 149 (14.8) 离退休人员 1 604 (80.4) 392 (19.6) 吸烟 9.2 0.001 不吸烟 2 330 (83.0) 476 (17.0) 吸烟 270 (82.6) 57 (17.4) 已戒烟 53 (69.7) 23 (30.3) 饮酒 9.4 < 0.001 不饮酒 2 327 (82.4) 496 (17.6) 饮酒 291 (86.6) 45 (13.4) 已戒酒 35 (70.0) 15 (30.0) 高脂饮食 10.0 < 0.001 否 2 602 (83.0) 533(17.0) 是 51 (68.9) 23(31.1) 锻炼 0.3 0.598 否 1 304 (82.3) 280 (17.7) 是 1 349 (83.0) 276 (17.0) 表 2 研究对象糖尿病影响相关因素分析
Table 2. Analysis of diabetes-related factors of participants
变量 未患病(%) 患病(%) 不分性别OR (95% CI)值a 男性OR (95% CI)值b 女性OR (95% CI)值b 家族史 阴性 2 479 (84.7) 448 (15.3) 1.00 1.00 1.00 阳性 174 (61.7) 108 (38.3) 4.52(3.40~6.03)c 4.50 (2.78~7.30)c 4.80 (3.32~6.94)c 血脂异常 否 2 502 (84.4) 464 (15.6) 1.00 1.00 1.00 是 151 (62.1) 92 (37.9) 3.13 (2.32~4.22)c 4.93 (3.02~8.06)c 2.42 (1.63~3.60)c 注:a校正烟、酒、高脂饮食、锻炼、BMI、SBP、DBP、年龄、性别、文化程度、婚姻状况及职业;b校正烟、酒、高脂饮食、锻炼、BMI、SBP、DBP、年龄、文化程度、婚姻状况及职业;cP<0.001。 表 3 糖尿病家族史与血脂异常对糖尿病交互作用的定性分析
Table 3. Qualitative analysis of the interaction between family history and dyslipidemia
家族史/血脂异常 未患病(%) 患病(%) 不分性别OR (95% CI)值a 男性OR (95% CI)值b 女性OR (95% CI)值b 否/否 2 348 (86.0) 383 (14.0) 1.00 1.00 1.00 是/否 154 (65.5) 81 (34.5) 4.43 (3.22~6.10)c 4.62 (2.71~7.87)c 4.52 (3.00~6.79)c 否/是 131 (66.8) 65 (33.2) 2.98 (2.12~4.19)c 5.04 (2.93~8.67)c 2.10 (1.31~3.36)c 是/是 20 (42.6) 27 (57.4) 10.27 (5.52~19.11)c 15.24 (4.57~50.82)c 9.84 (4.58~21.12)c 注:a校正烟、酒、高脂饮食、锻炼、BMI、SBP、DBP、年龄、性别、文化程度、婚姻状况及职业;b校正烟、酒、高脂饮食、锻炼、BMI、SBP、DBP、年龄、文化程度、婚姻状况及职业;cP<0.001。 表 4 糖尿病家族史与血脂异常交互作用的定量分析
Table 4. Quantitative analysis of the interaction between family history and dyslipidemia
指标 不分性别a 男性b 女性b RERI 3.86 (0.26~7.45) 6.59 (~3.17~16.35) 4.22 (0.07~8.36) AP(%) 37.6 (16.1~59.0) 43.2 (12.1~74.4) 42.9 (19.4~66.3) S 1.71 (1.15~2.56) 1.86 (1.02~3.46) 1.91 (1.16~3.15) AP×(AB)% 41.6 46.3 47.7 注:a校正烟、酒、高脂饮食、锻炼、BMI、SBP、DBP、年龄、性别、文化程度、婚姻状况及职业;b校正烟、酒、高脂饮食、锻炼、BMI、SBP、DBP、年龄、文化程度、婚姻状况及职业。 -
[1] Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives[J]. Nat Rev Endocrinol, 2017(8): 228-236. DOI: 10.1038/nrendo.2011.183. [2] Bianco A. The relevant role of family history in predicting type 2 diabetes occurrence[J]. Pol Arch Intern Med, 2019, 129(7-8): 438-439. DOI: 10.20452/pamw.14951. [3] Moonesinghe R, Beckles GLA, Liu T, et al. The contribution of family history to the burden of diagnosed diabetes, undiagnosed diabetes, and prediabetes in the United States: analysis of the National Health and Nutrition Examination Survey, 2009-2014[J]. Genet Med, 2018, 20: 1159-1166. DOI: 10.1038/gim.2017.238. [4] 潘磊磊, 卢春明, 吴明, 等. 辽宁省35~75岁居民糖尿病患病率及影响因素[J]. 中华疾病控制杂志, 2020, 24(6): 670-675. DOI: 10.16462/j.cnki.zhjbkz.2020.06.010.Pan LL, Lu CM, WuM, et al. Prevalence and influencing factors of diabetes mellitus among residents aged 35 ~ 75 years in Liaoning Province[J]. The Chinese journal of disease control, 2020, 24(6): 670-675. DOI: 10.16462/j.cnki.zhjbkz.2020.06.010. [5] 路媛, 刘焕乐, 马韫韬, 等. 总胆固醇与2型糖尿病关联性的前瞻性队列研究[J]. 中华疾病控制杂志, 2020, 24(4): 380-383+479. DOI: 10.16462/j.cnki.zhjbkz.2020.04.002.Lu Y, Liu W L, MA W T, et al. A prospective cohort study on the association between total cholesterol and type 2 diabetes[J]. The Chinese journal of disease control, 2020, 24(4): 380-383+479. DOI: 10.16462/j.cnki.zhjbkz.2020.04.002. [6] Liu Lu, Guan Xiaoling, Yuan Zhongshang, et al. Different Contributions of Dyslipidemia and Obesity to the Natural History of Type 2 Diabetes: 3-Year Cohort Study in China[J]. J Diabetes Res, 2019, 2019: 4328975. DOI: 10.1155/2019/4328975. [7] 李荣成, 荣右明, 李亚丽, 等. 糖尿病家族史与腰高比异常对2型糖尿病患病风险的交互作用[J]. 中华糖尿病杂志, 2018, 10(9): 606-610. DOI: 10.3760/cma.j.issn.1674-5809.2018.09.008.Li RC, Rong RM, Li YL, et al. Interaction between family history of diabetes and abnormal waist height ratio on risk of type 2 diabetes[J]. Chinese Journal of Diabetes, 2018, 10(9): 606-610. DOI: 10.3760/cma.j.issn.1674-5809.2018.09.008. [8] 余成, 王敏珍, 靳亚飞, 等. 家族史和肥胖交互作用对糖尿病前期人群糖尿病发病的影响[J]. 中华疾病控制杂志, 2020, 24(9): 997-1002. DOI: 10.16462/j.cnki.zhjbkz.2020.09.002.Yu Cheng, WANG Minzhen, Jin Yafei, et al. The influence of family history and obesity interaction on the onset of diabetes in pre-diabetic population[J]. The Chinese journal of disease control, 2020, 24(9): 997-1002. DOI: 10.16462/j.cnki.zhjbkz.2020.09.002. [9] Wang L, Gao P, Zheng M, et al. Prevalence and Ethuic pattern of drabetes and prediabtes in China in 2013. JAMA. 2017 Jun 27: 317(24): 2515-2523. DOI: 10.1001/jana.2017.7596. [10] 张作记. 行为医学量表手册[M]. 北京: 中华医学电子音像出版社, 2005: 114-119.Zhang ZJ. Handbook of behavioral medicine scale[M]. Beijing: China Medical Electronic Audio & Video Press, 2005: 114-119. [11] 樊萌语, 吕筠, 何平平. 国际体力活动问卷中体力活动水平的计算方法[J]. 中华流行病学杂志, 2014, 35(8): 961-964. DOI: 10.3760/cma.j.issn.0254-6450.2014.08.019.Fan Mengyu, Lv Yun, HE Pingping. Calculation method of physical activity level in international Physical Activity Questionnaire[J]. Chinese Journal of Epidemiology, 2014, 35(8): 961-964. DOI: 10.3760/cma.j.issn.0254-6450.2014.08.019. [12] 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019, 24(1): 24-56. DOI: 10.3969/j.issn.1007-5410.2019.01.002.Chinese Guidelines for hypertension prevention and Treatment (2018 Revision)[J]. Chinese Journal of Cardiovascular Medicine, 2019, 24(1): 24-56. DOI: 10.3969/j.issn.1007-5410.2019.01.002. [13] 中国2型糖尿病防治指南(2017年版)[J]. 中华糖尿病杂志, 2018, 10(1): 4-67. DOI: 10.3760/cma.j.issn.1674-5809.2018.01.003.Chinese Guidelines for the Prevention and treatment of Type 2 Diabetes (2017 edition)[J]. Chinese Journal of Diabetes, 2018, 10(1): 4-67. DOI: 10.3760/cma.j.issn.1674-5809.2018.01.003. [14] 诸骏仁, 高润霖, 赵水平, 等. 中国成人血脂异常防治指南(2016年修订版)[J]. 中国循环杂志, 2016, 31(10): 937-953. DOI: 10.3969/j.issn.1000-3614.2016.10.001.Zhu JR, Gao RL, Zhao SP, et al. Chinese Guidelines for the Prevention and Treatment of dyslipidemia in Adults (2016 Revision)[J]. Chinese Journal of Circulation, 2016, 31(10): 937-953. DOI: 10.3969/j.issn.1000-3614.2016.10.001. [15] Andersson T, Alfredsson L, Källberg H, et al. Calculating measures of biological interaction[J]. Eur J Epidemiol, 2005, 20(7): 575-579. DOI: 10.1007/s10654-005-7835-x. [16] 谢玮, 张静娴, 朱谦让, 等. 2014年江苏省成年居民糖尿病流行状况[J]. 江苏预防医学, 2019, 30(5): 522-525. DOI: 10.13668/j.issn.1006-9070.2019.05.017.Xie W, Zhang JX, Zhu QR, et al. Prevalence of diabetes among adult residents in Jiangsu Province in 2014[J]. Jiangsu Preventive Medicine, 2019, 30(5): 522-525. DOI: 10.13668/j.issn.1006-9070.2019.05.017. [17] 周婷, 刘祥, 李晓松, 等. 中国人群2型糖尿病影响因素的Meta分析[J]. 中华流行病学杂志, 2016, 37(5): 730-736. DOI: 10.3760/cma.j.issn.0254-6450.2016.05.030.Zhou T, Liu X, Li XS, et al. Meta-analysis of influencing factors of type 2 diabetes in Chinese population[J]. Chinese Journal of Epidemiology, 2016, 37(5): 730-736. DOI: 10.3760/cma.j.issn.0254-6450.2016.05.030. [18] Relimpio F, Martinez-Brocca MA, Leal-Cerro A, et al. Variability in the presence of the metabolic syndrome in type 2 diabetic patients attending a diabetes clinic. Influences of age and gender[J]. Diabetes Res Clin Pract, 2004, 65: 135-142. DOI: 10.1016/j.diabres.2003.12.003. [19] Al-Zakwani I, Al-Mahruqi F, Al-Rasadi K, et al. Sex disparity in the management and outcomes of dyslipidemia of diabetic patients in the Arabian Gulf: findings from the CEPHEUS study[J]. Lipids Health Dis, 2018, 17(1): 25. DOI: 10.1186/s12944-018-0667-y. [20] Gǎman MA, Cozma MA, Dobric EC, et al. Dyslipidemia: A Trigger for Coronary Heart Disease in Romanian Patients with Diabetes[J]. Metabolites, 2020, 10(5): E195. DOI: 10.3390/metabo10050195. [21] 鲍春丹, 孙波, 兰莉, 等. 哈尔滨市血压正常居民糖尿病家族史和高血脂交互作用与糖尿病关系的研究[J]. 中华流行病学杂志, 2017, 38(5): 611-614. DOI: 10.3760/cma.j.issn.0254-6450.2017.05.010.Bao CD, Sun B, Lan L, et al. Impact of Interaction between family history of diabetes and hyperlipidemia on diabetes among residents with normal blood pressure in Harbin[J]. Chinese Journal of Epidemiology, 2017, 38(5): 611-614. DOI: 10.3760/cma.j.issn.0254-6450.2017.05.010. -





 下载:
下载: