A systematic review and Meta-analysis on the carcinogenic risk difference of HBV subtypes
-
摘要:
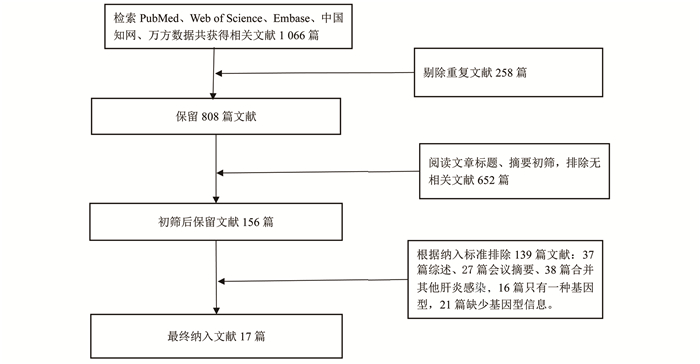
目的 探究不同基因型的HBV引发肝细胞癌(简称“肝癌”)风险差异及其潜在机制。 方法 通过检索数据库PubMed、Web of Science、Embase、中国知网(China national knowledge infrastructure, CNKI)及万方数据获取相关数据,利用Meta分析的方法进行数据整合。从National Center for Biotechnology Information(NCBI)Genbank数据库获取HBV的DNA序列,并分析不同基因型的HBV危险突变发生频率。 结果 共检出相关文献1 066篇,经筛检纳入符合要求文献17篇。总调查人数为16 288例,其中肝癌患者3 613例。Meta分析结果显示,感染HBV C基因型患者罹患肝癌风险较A、B及D基因型高,而感染A、B及D基因型的患者发生肝癌风险差异无统计学意义(均有P>0.05)。HBV DNA突变频率分析结果显示,C基因型中危险突变发生频率高于其他基因型。 结论 HBV C基因型与其他主要基因型相比,发生肝癌的风险更高,这可能归因于C基因型发生危险突变的频率更高。 Abstract:Objective To explore the risk difference and potential mechanisms on the hepatocellular carcinogenesis of different HBV genotypes. Methods Literatures were retrieved from PubMed, Web of Science, Embase databases Wanfang data and CNKI. Data were synthesized by meta-analysis methods. HBV sequences were obtained from NCBI-GenBank and the mutation frequency of different HBV genotypes were calculated. Results A total of 1 066 studies were retrieved via literature search. Finally, 17 studies were included in the Meta-analysis after eligibility screening. The total number of study subjects was 16 288, including 3 613 liver cancer patients. Patients with HBV C genotype had a higher risk of liver cancer than genotypes A, B, and D. While no significant difference in the risk of liver cancer across genotypes A, B and D was observed. The frequency of mutations indicated that most mutations were more frequently occurred in genotype C compared with other genotypes. Conclusions HBV genotype C is associated with a higher risk of hepatocellular carcinoma than other genotypes, which might due to more risk mutations genotype C HBV possessed. -
Key words:
- HBV /
- Genotype /
- Liver cancer /
- Meta-analysis
-
表 1 纳入文献基本情况
Table 1. Characteristic of included studies
作者及年份 地区 研究人数 肝癌人数 研究的基因型 研究设计 质量评分 杨家红2013[9] 中国大陆 1 152 112 B、C 横断面研究 A-6 郑丹2015[10] 中国大陆 123 53 B、C 病例对照研究 N-6 Chen 2012[11] 中国大陆 466 156 B、C 病例对照研究 N-6 Kao 2000[12] 中国台湾 270 80 A、B、C、D、 横断面研究 A-7 Fujie 2001[13] 日本 109 58 B、C 病例对照研究 N-5 陈岳明2009[14] 中国大陆 175 86 B、C 横断面研究 A-5 Asim 2010[15] 印度 189 88 A、D 病例对照研究 N-7 Chen 2014[16] 中国大陆 328 97 B、C 病例对照研究 N-7 Sumi 2003[7] 日本 585 74 A、B、C 横断面研究 A-8 Sung 2008[17] 中国香港 200 100 B、C 病例对照研究 N-6 Toan 2006[18] 越南 375 84 A、B、C、D 横断面研究 A-8 Wen 2015[19] 中国大陆 3 067 1 507 B、C、D 病例对照研究 N-7 Yang 2008[6] 中国台湾 2 762 153 B、C 横断面研究 A-9 Yin 2008[20] 中国大陆 1 121 462 A、B、C、D 横断面研究 A-7 Yu 2005[21] 中国台湾 470 154 A、B、C 病例对照研究 N-7 Yuen 2004[22] 中国香港 270 90 B、C 病例对照研究 N-6 Li 2010[23] 中国大陆 4 300 203 B、C、D 病例对照研究 N-5 注:A:AHRQ,横断面文献质量评价工具;N:NOS,病例对照文献质量评价工具。 表 2 亚组分析
Table 2. Subgroup analysis
分组 研究数量 样本量 OR(95% CI)值 I2值(%) P值 研究类型 横断面研究 7 6 013 2.18(1.34~3.52) 84 0.002 病例对照研究 9 8 656 3.22(1.78~5.83) 92 < 0.001 地区 中国大陆 8 10 071 3.24(1.76~5.97) 94 < 0.001 其他 8 4 598 2.19(1.34~3.58) 82 0.002 -
[1] Schweitzer A, Horn J, Mikolajczyk RT, et al. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013[J]. Lancet, 2015, 386(10003): 1546-1555. DOI: 10.1016/S0140-6736(15)61412-X. [2] Hutin Y, Nasrullah M, Easterbrook P, et al. Access to treatment for hepatitis B virus infection-worldwide, 2016[J]. MMWR Morb Mortal Wkly Rep, 2018, 67(28): 773-777. DOI: 10.15585/mmwr.mm6728a2. [3] Lai CL, Yuen MF. Prevention of hepatitis B virus-related hepatocellular carcinoma with antiviral therapy[J]. Hepatology, 2013, 57(1): 399-408. DOI: 10.1002/hep.25937. [4] El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma[J]. Gastroenterology, 2012, 142(6): 1264-1273. e1. DOI: 10.1053/j.gastro.2011.12.061. [5] Lu SN, Su WW, Yang SS, et al. Secular trends and geographic variations of hepatitis B virus and hepatitis C virus-associated hepatocellular carcinoma in Taiwan[J]. Int J of Cancer, 2006, 119(8): 1946-1952. DOI: 10.1002/ijc.22045. [6] Yang HI, Yeh SH, Chen PJ, et al. Associations between hepatitis B virus genotype and mutants and the risk of hepatocellular carcinoma[J]. J Natl Cancer Inst, 2008, 100(16): 1134-1143. DOI: 10.1093/jnci/djn243. [7] Sumi H, Yokosuka O, Seki N, et al. Influence of hepatitis B virus genotypes on the progression of chronic type B liver disease[J]. Hepatology, 2003, 37(1): 19-26. DOI: 10.1053/jhep.2003.50036. [8] 曾宪涛, 刘慧, 陈曦, 等. Meta分析系列之四: 观察性研究的质量评价工具[J]. 中国循证心血管医学杂志, 2012, 4(4): 297-299. doi: 10.3969/j.1674-4055.2012.04.004Zeng XT, Liu H, Chen X, et al. Meta analysis series Ⅳ: quality evaluation tools for observational research[J]. Chin J Evid Based Cardiovasc Med, 2012, 4(4): 297-299. doi: 10.3969/j.1674-4055.2012.04.004 [9] 杨家红, 陈皋, 张浩, 等. 四川省德阳地区乙型肝炎病毒相关性肝癌患者的病毒基因型分布及其临床特点[J]. 中华肝脏病杂志, 2013, 21(6): 473-474. DOI:10.3760/cma.j.issn.1007-3418.2013.030.20.Yang JH, Chen G, Zhang H, et al. Distribution of HBV genotypes and clinical characteristics of HBV-related hepatocellular carcinoma patients in Deyang District, Sichuan Province[J]. Chin J Hepatol, 2013, 21(6): 473-474. DOI: 10.3760/cma.j.issn.1007-3418.2013.03020. [10] 郑丹, 邓伟, 黄天壬, 等. 广西壮族自治区肝癌高发区HBV基因型、BCP/前C区突变与肝癌相关性的研究[J]. 中华流行病学杂志, 2015, 36(7): 725-729. DOI: 10.3760/cma.j.issn.0254-6450.2015.07.013.Zheng D, Deng W, Huang TR, et al. Relationship between hepatitis B virus genotype, BCP/Pre-C region mutations and risk of hepatocellular carcinoma in Guangxi Zhuang Autonomous Region[J]. Chin J Epidemiol, 2015, 36(7): 725-729. DOI: 10.3760/cma.j.issn.0254-6450.2015.07.013. [11] Chen Y, Yu D, Zhang W, et al. HBV subgenotype C2 infection, A1762T/G1764A mutations may contribute to hepatocellular carcinoma with cirrhosis in southeast China[J]. Iran J Public Health, 2012, 41(11): 10-18. [12] Kao JH, Chen PJ, Lai MY, et al. Hepatitis B genotypes correlate with clinical outcomes in patients with chronic hepatitis B[J]. Gastroenterology, 2000, 118(3): 554-559. DOI: 10.1016/s0016-5085(00)70261-7. [13] Fujie H, Moriya K, Shintani Y, et al. Hepatitis B virus genotypes and hepatocellular carcinoma in Japan[J]. Gastroenterology, 2001, 120(6): 1564-1565. DOI: 10.1053/gast.2001.24501. [14] 陈岳明, 高春芳, 戚鹏, 等. 乙型肝炎病毒基因型与慢性乙型病毒性肝炎及原发性肝细胞癌病理特点之间的关系[J]. 第二军医大学学报, 2009, 30(3): 279-282. DOI: 10.3724/SP.J.1008.2009.00279.Chen YM, Gao CF, Qi P, et al. Relationship of hepatitis B virus genotypes with clinicopathological characteristics in patients with chronic hepatitis B and hepatocellular carcinoma[J]. Acad J Second Mil Med Univ, 2009, 30(3): 279-282. DOI: 10.3724/SP.J.1008.2009.00279. [15] Asim M, Malik A, Sarma MP, et al. Hepatitis B virus BCP, Precore/core, X gene mutations/genotypes and the risk of hepatocellular carcinoma in India[J]. J Med Virol, 2010, 82(7): 1115-1125. DOI: 10.1002/jmv.21774. [16] Chen QY, Harrison TJ, Sabin CA, et al. The effect of HBV genotype C on the development of HCC differs between wild-type viruses and those with BCP double mutations (T(1762)A(1764))[J]. Hepa Mon, 2014, 14(2): e16214. DOI: 10.5812/hepatmon.16214. [17] Sung JJ, Tsui SK, Tse CH, et al. Genotype-specific genomic markers associated with primary hepatomas, based on complete genomic sequencing of hepatitis B virus[J]. J Virol, 2008, 82(7): 3604-3611. DOI: 10.1128/jvi.01197-07. [18] Toan NL, Song le H, Kremsner PG, et al. Impact of the hepatitis B virus genotype and genotype mixtures on the course of liver disease in Vietnam[J]. Hepatology, 2006, 43(6): 1375-1384. DOI: 10.1002/hep.21188. [19] Wen J, Song C, Jiang D, et al. Hepatitis B virus genotype, mutations, human leukocyte antigen polymorphisms and their interactions in hepatocellular carcinoma: a multi-centre case-control study[J]. Sci Rep, 2015, 5: 16489. DOI: 10.1038/srep16489. [20] Yin J, Zhang H, Li C, et al. Role of hepatitis B virus genotype mixture, subgenotypes C2 and B2 on hepatocellular carcinoma: compared with chronic hepatitis B and asymptomatic carrier state in the same area[J]. Carcinogenesis, 2008, 29(9): 1685-1691. DOI: 10.1093/carcin/bgm301. [21] Yu MW, Yeh SH, Chen PJ, et al. Hepatitis B virus genotype and DNA level and hepatocellular carcinoma: a prospective study in men[J]. J Natl Cancer Inst, 2005, 97(4): 265-272. DOI: 10.1093/jnci/dji043. [22] Yuen MF, Tanaka Y, Mizokami M, et al. Role of hepatitis B virus genotypes Ba and C, core promoter and precore mutations on hepatocellular carcinoma: a case control study[J]. Carcinogenesis, 2004, 25(9): 1593-1598. DOI: 10.1093/carcin/bgh172. [23] Li XD, Wang L, Zhong YW, et al. Hepatitis B virus (HBV) subgenotypes C2 and B2 differ in lamivudine- and adefovir-resistance-associated mutational patterns in HBV-infected Chinese patients[J]. J Clin Microbiol, 2010, 48(12): 4363-4369. DOI: 10.1128/jcm.01518-10. [24] Liu SJ, Zhang HW, Gu CY, et al. Associations between hepatitis B virus mutations and the risk of hepatocellular carcinoma: a meta-analysis[J]. J Natl Cancer Inst, 2009, 101(15): 1066-1082. DOI: 10.1093/jnci/djp180. [25] Livingston SE, Simonetti JP, McMahon BJ, et al. Hepatitis B virus genotypes in Alaska Native people with hepatocellular carcinoma: preponderance of genotype F[J]. J Infect Dis, 2007, 195(1): 5-11. DOI: 10.1086/509894. [26] Wong GL, Chan HL, Yiu KK, et al. Meta-analysis: The association of hepatitis B virus genotypes and hepatocellular carcinoma[J]. Aliment Pharmacol Ther, 2013, 37(5): 517-526. DOI: 10.1111/apt.12207. [27] Fang ZL, Sabin CA, Dong BQ, et al. HBV A1762T, G1764A mutations are a valuable biomarker for identifying a subset of male HBsAg carriers at extremely high risk of hepatocellular carcinoma: a prospective study[J]. AM J Gastroenterol, 2008, 103(9): 2254-2262. DOI: 10.1111/j.1572-0241.2008.01974.x. [28] Tanaka Y, Mukaide M, Orito E, et al. Specific mutations in enhancer Ⅱ/core promoter of hepatitis B virus subgenotypes C1/C2 increase the risk of hepatocellular carcinoma[J]. J Hepatol, 2006, 45(5): 646-653. DOI: 10.1016/j.jhep.2006.06.018. [29] Cho EY, Choi CS, Cho JH, et al. Association between hepatitis B virus X gene mutations and clinical status in patients with chronic hepatitis B infection[J]. Gut Liver, 2011, 5(1): 70-76. DOI: 10.5009/gnl.2011.5.1.70. -





 下载:
下载: