Association of body mass index with activities of daily life among middle-aged and older Chinese
-
摘要:
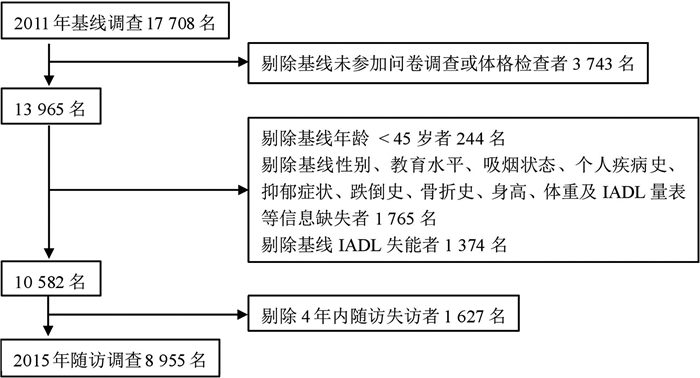
目的 探究中国中老年人BMI与工具性日常生活活动能力(instrumental activities of daily living, IADL)之间的关系。 方法 本研究基于中国健康与养老追踪调查(China health and retirement longitudinal study, CHARLS)2011-2015年的随访数据,剔除基线存在IADL失能者,最终纳入研究对象8 955名。采用二分类Logistic线性回归分析模型分析BMI与IADL失能发生风险的关联。 结果 经过4年的随访,2 186名(24.41%)研究对象发生IADL失能,其中男性和女性发生率分别为18.79%和29.89%。低体重、正常体重、超重及肥胖组的IADL失能发生率分别为42.64%、25.13%、19.85%和23.49%。与正常体重组相比,低体重、超重及肥胖组IADL失能发生风险的OR值分别为1.381(95% CI: 1.117~1.707, P=0.003)、0.830(95% CI: 0.727~0.948, P=0.006)和0.985(95% CI: 0.819~1.185, P=0.874)。 结论 与正常体重组相比,中老年人群中低体重与IADL失能的发生呈正向关联,而超重则与IADL失能呈负相关关系,肥胖与IADL失能之间不存在统计学意义。 Abstract:Objective To examine the association between BMI and the incidence of disability assessed by instrumental activities of daily living (IADL) among middle-aged and older Chinese. Methods This study was based on the China health and retirement longitudinal study 2011-2015 (baseline to second follow-up visits). After excluding participants with IADL-defined disability at baseline, 8 955 participants were included in the study. Binary Logistic liner regression model was performed to determine the association bewteen BMI and incidence of IADL-defined disability. Results During 4 years of follow-up, 2 186 (24.41%) participants developed disability (18.79% in men and 29.89% in women). The incidence rates of disability were 42.64%, 25.13%, 19.85% and 23.49% in the underweight, normal weight, overweight and obesity groups, respectively. Compared with participants with normal weight, the adjusted odds ratio of disability in participants who were underweight, overweight and obese were 1.381 (95% CI: 1.117-1.707, P=0.003)、0.830 (95% CI: 0.727-0.948, P=0.006) and 0.985 (95% CI: 0.819-1.185, P=0.874), respectively. Conclusions Compared with participants with normal weight, underweight was positively associated with risk of disability, and there was an inverse association between overweight and disability, while no significant association was observed between obesity and disability. -
Key words:
- BMI /
- Activities of daily life /
- Disability /
- Cohort study
-
表 1 研究对象的基线特征及4年内发生IADL失能情况比较a
Table 1. Baseline characteristics and incidence of IADL disability at the end of 4- year follow-up among study populationsa
特征 BMI分组 H值 P值 工具性日常活动能力失能 Z/t/χ2值 P值 低体重 正常体重 超重 肥胖 否 是 调查人数(名) 523 4 759 2 630 1 043 6 769 2 186 年龄(岁) 63.30±9.39 58.57±8.80 57.10±8.32 56.51±8.50 237.781b < 0.001 56.76±8.12 62.54±9.34 -25.096c < 0.001 BMI(kg/m2) 17.32±1.09 21.53±1.50 25.74±1.12 30.53±2.94 7367.342b < 0.001 23.75±3.69 23.02±3.93 8.585c < 0.001 男性 256(48.95) 2 656(55.81) 1 142(43.42) 364(34.90) 152.655b < 0.001 3 588 (53.01) 830 (37.97) 149.484d < 0.001 农村 466(89.10) 4 022(84.51) 2 013(76.54) 795(76.22) 50.282b < 0.001 5 343(78.93) 1 953(89.34) 118.908d < 0.001 教育程度 80.999b < 0.001 1021.876d < 0.001 文盲 181(34.61) 1 114(23.41) 554(21.06) 243(23.30) 1 080(15.96) 1 012(46.29) 小学及以下e 233(44.55) 2 106(44.25) 1 028(39.09) 413(39.60) 2 915(43.06) 865(39.57) 初中 71(13.58) 1 024(21.52) 680(25.86) 270(25.89) 1 819(26.87) 226(10.34) 高中及以上 38(7.27) 515(10.82) 368(13.99) 117(11.22) 955(14.11) 83(3.80) 婚姻状态 12.067b 0.007 164.857d < 0.001 已婚 447(85.47) 4 190(88.04) 2 413(91.75) 962(92.23) 6 192(91.48) 1 820(83.26) 分居或离异 5(0.96) 67(1.41) 19(0.72) 10(0.96) 88(1.30) 13(0.59) 丧偶 67(12.81) 462(9.71) 194(7.38) 67(6.42) 452(6.68) 338(15.46) 未婚 4(0.76) 40(0.84) 4(0.15) 4(0.38) 37(0.55) 15(0.69) 吸烟状态 102.206b < 0.001 60.480d < 0.001 从不吸烟 281(53.73) 2 555(53.69) 1 733(65.89) 755(72.39) 3 872(57.20) 1 452(66.42) 现在吸烟 204(39.01) 1 840(38.66) 647(24.60) 186(17.83) 2 311(34.14) 566(25.89) 过去吸烟 38(7.27) 364(7.65) 250(9.51) 102(9.78) 586(8.66) 168(7.69) 饮酒状态 34.046b < 0.001 41.952d < 0.001 从未饮酒 362(69.22) 3 085(64.82) 1 846(70.19) 793(76.03) 4 489(66.32) 1 597(73.06) 现在饮酒 129(24.67) 1 405(29.52) 634(24.11) 190(18.22) 1 898(28.04) 460(21.04) 过去饮酒 32(6.12) 269(5.65) 150(5.70) 60(5.75) 382(5.64) 129(5.90) 慢性疾病数量(种) 154.101b < 0.001 103.085d < 0.001 < 1 169(32.31) 1 810(38.03) 856(32.55) 239(22.91) 2 476(36.58) 598(27.36) 1~ 270(51.63) 2 391(50.24) 1 286(48.90) 512(49.09) 3 345(49.42) 1 114(50.96) 3 84(16.06) 558(11.73) 488(18.56) 292(28.00) 948(14.01) 474(21.68) 慢性疾病种类 高血压病 58(11.09) 731(15.36) 727(27.64) 470(45.06) 273.042b < 0.001 1 406(20.77) 580(26.53) 31.778d < 0.001 糖尿病 9(1.72) 157(3.30) 191(7.26) 119(11.41) 22.441b < 0.001 341(5.04) 135(6.18) 4.252d 0.039 慢性肺部疾病 100(19.12) 442(9.29) 201(7.64) 86(8.25) 17.641b 0.001 556(8.21) 273(12.49) 35.943d < 0.001 心脏疾病 52(9.94) 366(7.69) 311(11.83) 186(17.83) 29.310b < 0.001 621(9.17) 294(13.45) 32.919d < 0.001 中风 7(1.34) 52(1.09) 47(1.79) 28(2.68) 0.746b 0.862 84(1.24) 50(2.29) 12.273d < 0.001 关节炎或风湿病 179(34.23) 1 520(31.94) 843(32.05) 366(35.09) 3.171b 0.366 2 019(29.83) 889(40.67) 88.557d < 0.001 抑郁症状 243(46.46) 1 679(35.28) 774(29.43) 307(29.43) 49.125b < 0.001 1 981(29.27) 1 022(46.75) 226.682d < 0.001 认知功能评分f 10.58±3.83 11.64±3.57 12.22±3.50 12.25±3.61 83.877b < 0.001 12.38±3.33 9.77±3.80 22.929c < 0.001 跌倒和骨折史 90(17.21) 699(14.69) 392(14.90) 156(14.96) 0.901b 0.825 942(13.92) 395(18.07) 22.440d < 0.001 注:a年龄、BMI及认知功能评分以(x±s)表示,其余均以英文字符表示;b使用Kruskal-Wallis H检验;c使用Mann-Whitney U检验;d使用χ2检验;e小学及以下包括:未读完小学,但能够读、写;私塾;小学毕业;f认知功能状态缺失2 039人,慢性疾病种类均为基线调查时自报疾病。 表 2 不同BMI分组人群IADL各项功能受损情况[n(%)]
Table 2. IADL disability by categories of BMI [n(%)]
功能 BMI分组 合计 χ2值 P值a 低体重 正常体重 超重 肥胖 做家务 45(8.60)b 257(5.40) 133(5.06) 77(7.38) 512(5.72) 16.466 0.001 做饭 43(8.22)b 254(5.34) 123(4.68) 49(4.7) 469(5.24) 11.758 0.008 购物 42(8.03)b 249(5.23) 106(4.03) 63(6.04) 460(5.14) 17.430 0.001 理财 62(11.85) 411(8.64) 186(7.07) 83(7.96) 742(8.29) 14.780 0.002 吃药 19(3.63) 136(2.86) 55(2.09) 31(2.97) 241(2.69) 6.204 0.102 打电话 146(27.92)b 691(14.52) 270(10.27)b 110(10.55)b 1 217(13.59) 127.876 < 0.001 IADLc失能 223(42.64)b 1 196(25.13) 522(19.85)b 245(23.49) 2 186(24.41) 125.667 < 0.001 注:a χ2检验;b组间的多重比较采用χ2分割法:与正常体重组比较P < 0.05;c工具性日常生活活动能力(instrumental activities of daily living, IADL)。 表 3 BMI与IADL失能发生风险关联的Logistic线性回归分析模型分析
Table 3. Association of BMI with IADL disability in Logistic liner regression model
BMI分组 病例数/调查人数(n/N) 模型1a 模型2b 模型3c OR(95% CI)值 P值 OR(95% CI)值 P值 OR(95% CI)值 P值 正常体重 1 196/4 759 1.000 1.000 1.000 低体重 223/523 1.506(1.225~1.850) < 0.001 1.508(1.226~1.855) < 0.001 1.381(1.117~1.707) 0.003 超重 522/2 630 0.819(0.721~0.931) 0.002 0.816(0.718~0.928) 0.002 0.830(0.727~0.948) 0.006 肥胖 245/1 043 1.022(0.858~1.217) 0.805 1.016(0.853~1.210) 0.861 0.985(0.819~1.185) 0.874 注:a模型1:调整了年龄、性别、居住地、婚姻状态和文化程度;b模型2:在模型1的基础上,进一步调整了吸烟和饮酒;c模型3:在模型2的基础上,进一步调整基线自报患高血压、糖尿病(血糖升高)、慢性肺部疾病、心脏疾病、中风、关节炎或风湿病、抑郁症状、认知功能状态、跌倒史和骨折史。 -
[1] WHO. 中国老龄化与健康国家评估报告[EB/OL]. (2016-05-01)[2019-09-09]. http://www.who.int/ageing/publications/china-country-assessment/zh/.WHO. China country assessment report on ageing and health[EB/OL]. (2016-05-01)[2019-09-09]. http://www.who.int/ageing/publications/china-country-assessment/zh/. [2] Corona LP, Pereira de Brito TR, Nunes DP, et al. Nutritional status and risk for disability in instrumental activities of daily living in older Brazilians[J]. Public Health Nutr, 2014, 17(2): 390-395. DOI: 10.1017/S1368980012005319. [3] 张小宁, 陈爽. 中国老年人失能情况及影响因素研究[J]. 中国全科医学, 2019, 22(31): 3841-3844. DOI: 10.12114/j.issn.1007-9572.2019.00.508.Zhang XN, Chen S. Prevalence and associated factors of disability in elders living in China[J]. Chin Gen Pract, 2019, 22(31): 3841-3844. DOI: 10.12114/j.issn.1007-9572.2019.00.508. [4] 张晗, 王志会, 王丽敏, 等. 中国社区老年居民日常生活活动能力失能状况调查[J]. 中华流行病学杂志, 2019(3): 266-271. DOI:10.3760/cma.J.issn.0254-6450.2019.03.003.Zhang H, Wang ZH, Wang LM, et al. Study on activities of daily living disability in community-dwelling older adults in China[J]. Chin J Epidemiol, 2019(3): 266-271. DOI: 10.3760/cma.j.issn.0254-6450.2019.03.003. [5] Yang M, Hao Q, Luo L, et al. Body mass index and disability in Chinese nonagenarians and centenarians[J]. J Am Med Dir Assoc, 2014, 15(4): 303, e1-6. DOI: 10.1016/j.jamda.2013.10.011. [6] Zhao Y, Hu Y, Smith JP, et al. Cohort profile: the China health and retirement longitudinal study (CHARLS)[J]. Int J Epidemiol, 2014, 43(1): 61-68. DOI: 10.1093/ije/dys203. [7] 张文娟, 魏蒙. 中国老年人的失能水平到底有多高?——多个数据来源的比较[J]. 人口研究, 2015, 39(3): 34-47. https://www.cnki.com.cn/Article/CJFDTOTAL-RKYZ201503003.htmZhang WJ, Wei M. Disability level of the Chinese elderly: comparison from multiple data sources[J]. Population Research, 2015, 39(3): 34-47. https://www.cnki.com.cn/Article/CJFDTOTAL-RKYZ201503003.htm [8] Li J, Cacchione PZ, Hodgson N, et al. Afternoon napping and cognition in Chinese older adults: findings from the China Health and Retirement Longitudinal Study Baseline Assessment[J]. J Am Geriatr Soc, 2017, 65(2): 373-380. DOI: 10.1111/jgs.14368. [9] Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living[J]. Mater Sci Forum, 1969, 9: 179-186. http://www.ncbi.nlm.nih.gov/pubmed/5349366/ [10] Samper-Ternent R, Al Snih S. Obesity in older adults: epidemiology and implications for disability and disease[J]. Rev Clin Gerontol, 2012, 22(1): 10-34. DOI: 10.1017/s0959259811000190. [11] Zhang S, Tomata Y, Sugiyama K, et al. Body mass index and the risk of incident functional disability in elderly Japanese: The OHSAKI cohort 2006 study[J]. Medicine (Baltimore), 2016, 95(31): e4452. DOI: 10.1097/MD.0000000000004452. [12] Lv YB, Yuan JQ, Mao C, et al. Association of body mass index with disability in activities of daily living among Chinese adults 80 years of age or older[J]. JAMA Netw Open, 2018, 1(5): e181915. DOI: 10.1001/jamanetworkopen.2018.1915. [13] 齐士格, 王志会, 王丽敏, 等. 中国城乡老年人群两年内日常生活活动能力受损发生情况及影响因素[J]. 中华流行病学杂志, 2019(3): 272-276. DOI: 10.3760/cma.j.issn.0254-6450.2019.03.004.Qi SG, Wang ZH, Wang LM, et al. Incidence of activities of daily living disability and related factors in community-dwelling olderadults in China[J]. Chin J Epidemiol, 2019(3): 272-276. DOI: 10.3760/cma.j.issn.0254-6450.2019.03.004. [14] Lang T, Streeper T, Cawthon P, et al. Sarcopenia: etiology, clinical consequences, intervention, and assessment[J]. Osteoporos Int, 2010, 21(4): 543-559. DOI: 10.1007/s00198-009-1059-y. [15] Zimmer Z, Fang XH, Tang Z. Fifteen-year disability trends among older persons in the Beijing municipality of China[J]. J Aging Health, 2014, 26(2): 207-230. DOI: 10.1177/0898264313513609. -





 下载:
下载: