-
摘要:
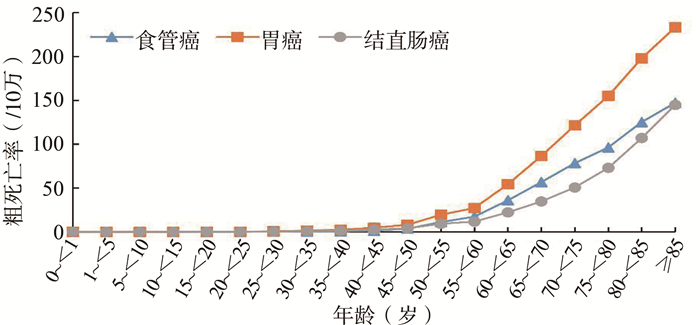
目的 分析2004―2018年中国消化道恶性肿瘤死亡状况及变化趋势。 方法 收集2004―2018年全国疾病监测地区消化道恶性肿瘤死亡数据,计算各种消化道恶性肿瘤粗死亡率和标化死亡率,采用Joinpoint回归分析模型分析标化死亡率变化趋势。 结果 2004―2018年,中国食管癌和胃癌标化死亡率呈下降趋势(AAPC食管癌=-4.7%, AAPC胃癌=-4.3%, 均有P<0.05),结直肠癌死亡率相对稳定(AAPC结直肠癌=0.4%, P=0.733)。各种消化道恶性肿瘤死亡率随年龄增长不断上升,男性标化死亡率均高于女性,且男性年均下降幅度较小;农村食管癌和胃癌标化死亡率高于城市,但农村年均下降速度较快;东部地区食管癌死亡率最高,中部地区胃癌标化死亡率最高,且中部地区下降速度较快;西部地区结直肠癌死亡率呈缓慢上升趋势。 结论 2004―2018年期间,中国食管癌和胃癌死亡状况有所好转,但西部地区结直肠癌死亡率仍呈上升趋势,应继续加大防治力度,以减轻消化道恶性肿瘤疾病负担。 Abstract:Objective To analyze the mortality status and trend of digestive tract malignant tumors in China from 2004 to 2018. Methods The mortality data of digestive tract malignant tumors in the national disease surveillance areas from 2004 to 2018 were collected. The crude and standardized mortality rates with various digestive tract malignant tumors were calculated. The trend of standardized mortality was analyzed using Joinpoint regression model. Results From 2004 to 2018, the standardized mortality rates of esophageal cancer and gastric cancer in China showed a general downward trend, with an average annual percent change (AAPC) of -4.7% and -4.3%(all P < 0.05), respectively. The mortality rate of colorectal cancer showed no significant change(AAPC=0.4%, P=0.733). The mortality rates of various digestive tract malignant tumors increased with age. The standardized mortality rates of various digestive tract malignant tumors among males were higher than those of females, and the average annual decline was smaller. The standardized mortality rates of esophageal cancer and gastric cancer in rural areas were higher than those in urban areas, but the average annual decrease was larger. The standardized mortality rate of esophageal cancer in eastern areas was the highest. The standardized mortality rate of gastric cancer in central areas was highest, and the rate of decline was faster. The mortality rate of colorectal cancer in western areas increased slowly. Conclusions From 2004 to 2018, the mortality rates of esophageal cancer and gastric cancer had improved, but the mortality rate of colorectal cancer was still on the rise in western areas. The preventive measures of digestive tract malignant tumors should be strengthened to reduce the burden of digestive tract malignant tumors. -
Key words:
- Digestive tract malignant tumor /
- Mortality /
- Trend analysis
-
表 1 2004―2018年中国消化道恶性肿瘤死亡率(/10万)
Table 1. Mortality of digestive tract malignant tumor in China from 2004 to 2018 (/100 000)
年份 食管癌 胃癌 结直肠癌 标化率比a 粗率 标化率 粗率 标化率 粗率 标化率 2004 15.46 18.43 25.23 29.99 7.31 8.66 2.13∶3.46∶1 2005 14.95 17.83 24.19 28.68 7.53 8.88 2.01∶3.23∶1 2006 12.81 14.93 18.87 21.85 7.17 8.28 1.80∶2.64∶1 2007 13.68 15.49 21.23 23.99 7.96 9.00 1.72∶2.67∶1 2008 13.20 14.40 20.64 22.45 8.07 8.77 1.64∶2.56∶1 2009 13.06 14.20 21.24 22.97 8.54 9.32 1.52∶2.46∶1 2010 12.05 13.03 20.39 21.90 8.27 9.11 1.43∶2.40∶1 2011 12.03 12.04 19.58 19.60 8.48 8.64 1.39∶2.37∶1 2012 11.84 11.09 20.01 18.77 8.81 8.26 1.34∶2.27∶1 2013 12.54 10.99 20.41 17.98 9.02 7.96 1.38∶2.26∶1 2014 12.84 11.03 21.10 18.24 9.65 8.33 1.32∶2.19∶1 2015 12.57 10.82 20.92 18.09 10.19 8.81 1.23∶2.05∶1 2016 12.51 10.07 20.51 16.64 10.47 8.49 1.19∶1.96∶1 2017 12.49 9.99 19.92 16.10 10.99 8.86 1.13∶1.82∶1 2018 12.36 9.44 19.69 15.22 11.58 8.95 1.05∶1.70∶1 合计 12.74 11.30 20.66 18.41 9.67 8.61 1.31∶2.14∶1 AAPC(%) -1.30 -4.70 -1.70 -4.30 3.30 0.40 P值 0.008 <0.001 0.003 <0.001 <0.001 0.733 注:a参考项为结直肠癌标化死亡率。 表 2 2004―2018年中国消化道恶性肿瘤死亡趋势变化a
Table 2. Death trends of digestive tract malignant tumor in China from 2004 to 2018 a
分类 变化趋势1a 变化趋势2a 变化趋势3a AAPC(95% CI)值 年份 APC(95% CI)值 年份 APC(95% CI)值 年份 APC(95% CI)值 男性 食管癌 2004―2018 -4.1(-4.6~-3.7) b -4.1(-4.6~-3.7) b 胃癌 2004―2018 -4.1(-4.8~-3.4) b -4.1(-4.8~-3.4) b 结直肠癌 2004―2018 0.1(-0.5~0.8) 0.1(-0.5~0.8) 女性 食管癌 2004―2018 -6.2(-7.1~-5.4) b -6.2(-7.1~-5.4) b 胃癌 2004―2018 -4.7(-5.7~-3.8) b -4.7(-5.7~-3.8) b 结直肠癌 2004―2009 1.4(-0.3~3.1) 2009―2012 -4.6(-11.6~2.9) 2012―2018 1.1(-0.2~2.4) -0.1(-1.5~1.5) 城市 食管癌 2004―2011 -6.2(-7.5~-4.9) b 2011―2014 6.0(-5.6~19.0) 2014―2018 -1.9(-5.3~1.7) -2.5(-4.7~-0.2) b 胃癌 2004―2016 -15.1(-25.2~-3.6) b 2016―2018 -2.4(-3.3~-1.5) b -4.3(-6.0~-2.6) b 结直肠癌 2004―2018 -0.4(-0.9~0.1) -0.4(-0.9~0.1) 农村 食管癌 2004―2018 -5.7(-6.4~-5.1) b -5.7(-6.4~-5.1) b 胃癌 2004―2018 -4.7(-5.5~-4.0) b -4.7(-5.5~-4.0) b 结直肠癌 2004―2018 0.4(-0.5~0.6) 0.4(-0.5~0.6) 东部 食管癌 2004―2012 -6.2(-7.6~-4.8) b 2012―2015 4.4(-10.6~21.8) 2015―2018 -6.6(-13.9~1.2) -4.1(-7.0~-1.0) b 胃癌 2004―2006 -12.2(-24.5~2.1) 2006―2018 -2.7(-3.7~-1.6) b -4.1(-6.0~-2.1) b 结直肠癌 2004―2018 0.1(-0.5~0.6) 0.1(-0.5~0.6) 中部 食管癌 2004―2018 -6.7(-7.4~-6.0) b -6.7(-7.4~-6.0) b 胃癌 2004―2018 -5.1(-6.0~-4.3) b -5.1(-6.0~-4.3) b 结直肠癌 2004―2018 -1.4(-2.4~-0.5) b -1.4(-2.4~-0.5) b 西部 食管癌 2004―2018 -3.4(-4.2~-2.7) b -3.4(-4.2~-2.7) b 胃癌 2004―2018 -4.7(-5.7~-3.6) b -4.7(-5.7~-3.6) b 结直肠癌 2004―2018 1.3(0.4~2.2) b 1.3(0.4~2.2) b 注:a基于最佳模型中连接点出现的个数和年份确定变化趋势列数及时间区间,变化趋势1、2、3分别代表不同时间区间内死亡率的变化趋势;bP<0.05。 -
[1] 任建松, 李倩, 关鹏, 等. 中国2008年消化道常见恶性肿瘤发病、死亡和患病情况的估计及预测[J]. 中华流行病学杂志, 2012, 33(10): 1052-1055. DOI: 10.3760/cma.j.issn.0254-6450.2012.10.013.Ren JS, Li Q, Guan P, et al. Estimation and prediction for incidence, mortality and prevalence of common gastrointestinal tract cancers in China, 2008[J]. Chin J Epidemiol, 2012, 33(10): 1052-1055. DOI: 10.3760/cma.j.issn.0254-6450.2012.10.013. [2] 高艳多. 1990-2015年中国消化道肿瘤死亡趋势的年龄-时期-出生队列模型分析[D]. 武汉: 武汉大学, 2017.Gao YD. An age-period-cohort model analysis of gastrointestinal cancer mortality from 1990 to 2015 in China[D]. Wuhan: Wuhan University, 2017. [3] 中国疾病预防控制中心慢性非传染性疾病预防控制中心. 中国死因监测数据集2018[M]. 北京: 中国科学技术出版社, 2018.Center for the Prevention and Control of Chronic Noncommunicable Diseases of Chinese Center for Disease Prevention and Control. China cause of death monitoring data in 2018[M]. Beijing: China Science and Technology Press, 2018. [4] Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates[J]. Stat Med, 2000, 19(3): 335-351. DOI: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [5] 刘晓雪, 宇传华, 周薇, 等. 中国近30年间结直肠癌死亡趋势分析[J]. 中国癌症杂志, 2018, 28(3): 177-183. DOI: 10.19401/j.cnki.1007-3639.2018.03.002.Liu XX, Yu CH, Zhou W, et al. Trends in colorectal cancer mortality for the last 30 years in China[J]. China Oncol, 2018, 28(3): 177-183. DOI: 10.19401/j.cnki.1007-3639.2018.03.002. [6] 贺君剑, 魏长慧, 李众, 等. 中国居民2004-2016年肝癌死亡趋势分析[J]. 郑州大学学报(医学版), 2020, 55(1): 119-122. DOI: 10.13705/j.issn.1671-6825.2019.04.150.He JJ, Wei CH, Li Z, et al. Analysis of liver cancer mortality trend among Chinese residents from 2004 to 2016[J]. J Zhengzhou Univ Med Sci, 2020, 55(1): 119-122. DOI: 10.13705/j.issn.1671-6825.2019.04.150. [7] 王静雷, 杨一兵, 耿云霞, 等. 1990-2017年中国胃癌发病、患病及死亡状况趋势分析[J]. 中国慢性病预防与控制, 2020, 28(5): 321-325. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.05.001.Wang JL, Yang YB, Geng YX, et al. Trend analysis of the morbidity, prevalence and mortality of stomach cancer in China from 1990 to 2017[J]. Chin J Prev Contr Chron Dis, 2020, 28(5): 321-325. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.05.001. [8] 郭康, 周脉耕, 石娅娅, 等. 2006-2012年中国人群食管癌死亡趋势分析[J]. 现代预防医学, 2015, 42(7): 1153-1156. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF201507001.htmGuo K, Zhou MG, Shi YY, et al. Trends and characteristics of mortality of esophagus cancer in China, 2006-2012[J]. Mod Prev Med, 2015, 42(7): 1153-1156. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF201507001.htm [9] 周家琛, 郑荣寿, 庄贵华, 等. 2000-2015年中国肿瘤登记地区胃癌发病趋势及年龄变化[J]. 实用肿瘤学杂志, 2020, 34(1): 1-5. DOI: 10.11904/j.issn.1002-3070.2020.01.001.Zhou JC, Zheng RS, Zhuang GH, et al. Analysis on the trend of gastric cancer incidence and age change in cancer registration areas of China, 2000 to 2015[J]. Prac Oncol J, 2020, 34(1): 1-5. DOI: 10.11904/j.issn.1002-3070.2020.01.001. [10] 陈万青, 李霓, 曹毛毛, 等. 2013-2017年中国城市癌症早诊早治项目基线结果分析[J]. 中国肿瘤, 2020, 29(1): 1-6. DOI: 10.11735/j.issn.1004-0242.2020.01.A001.Chen WQ, Li N, Cao MM, et al. Preliminary analysis of cancer screening program in urban China from 2013 to 2017[J]. China Cancer, 2020, 29(1): 1-6. DOI: 10.11735/j.issn.1004-0242.2020.01.A001. [11] Yuan Y. A survey and evaluation of population-based screening for gastric cancer[J]. Cancer Biol Med, 2013, 10(2): 72-80. DOI: 10.7497/j.issn.2095-3941.2013.02.002. [12] Wang GQ, Jiao GG, Chang FB, et al. Long-term results of operation for 420 patients with early squamous cell esophageal carcinoma discovered by screening[J]. Ann Thorac Surg, 2004;77(5): 1740-1744. DOI: 10.1016/j.athoracsur.2003.10.098. [13] 国家卫生健康委员会. 食管癌诊疗规范(2018年版)[J]. 中华消化病与影像杂志(电子版), 2019, 9(4): 118-144. DOI: 10.3877/cma.j.issn.2095-2015.2019.03.008.National Health Commission of the People's Republic of China. Guidelines for the Diagnosis and Treatment of Esophageal Cancer (2018 Edition)[J]. Chin J Dig Med Imageology Electron Ed, 2019, 9(3): 118-144. DOI: 10.3877/cma.j.issn.2095-2015.2019.03.008. [14] 王玮, 周志伟. 进展期胃癌围术期治疗进展[J]. 肿瘤综合治疗电子杂志, 2018, 4(2): 68-72. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLZD201802017.htmWang W, Zhou ZW. Development of the treatment for advanced gastric cancer in perioperative period[J]. J Multidiscip Cancer Manag Electron Version, 2018, 4(2): 68-72. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLZD201802017.htm [15] 朱建飞, 豆亚伟, 田伟, 等. 术前吸烟及饮酒状态对食管鳞状细胞癌术后复发和转移的影响[J]. 中国胸心血管外科临床杂志, 2021, 28(2): 219-224. DOI: 10.7507/1007-4848.202004047.Zhu JF, Dou YW, Tian W, et al. Effects of smoking and drinking status before operation on recurrence and metastasis of esophageal squamous cell carcinoma[J]. Chin J Clin Thorac Cardiovasc Surg, 2021, 28(2): 219-224. DOI: 10.7507/1007-4848.202004047. [16] Wang JB, Fan JH, Liang H, et al. Attributable causes of esophageal cancer incidence and mortality in China[J]. PLoS One, 2012, 7(8): e42281. DOI: 10.1371/journal.pone.0042281. [17] 董佩, 石菊芳, 邱五七, 等. 2015-2017年中国城市居民肿瘤防治健康素养现况及相关因素分析[J]. 中华预防医学杂志, 2020, 54(1): 76-83. DOI: 10.3760/cma.j.issn.0253-9624.2020.01.015.Dong P, Shi JF, Qiu WQ, et al. Analysis on the health literacy of the cancer prevention and treatment and its related factors among urban residents in China from 2015 to 2017[J]. Chin J Prev Med, 2020, 54(1): 76-83. DOI: 10.3760/cma.j.issn.0253-9624.2020.01.015. [18] 丁璐璐, 朱健, 张永辉, 等. 江苏省启东市1972-2016年胃癌死亡趋势分析[J]. 肿瘤防治研究, 2020, 47(10): 782-787. DOI: 10.3971/j.issn.1000-8578.2020.20.0142.Ding LL, Zhu J, Zhang YH, et al. Mortality trends of stomach cancer in Qidong City, 1972-2016[J]. Cancer Res Prev Treat, 2020, 47(10): 782-787. DOI: 10.3971/j.issn.1000-8578.2020.20.0142. [19] 马瑞忠, 刘洪明. 消化道肿瘤腹膜后淋巴结转移的治疗进展[J]. 中国医药指南, 2012, 10(17): 78-81. DOI: 10.3969/j.issn.1671-8194.2012.17.050.Ma RZ, Liu HM. Progress in the treatment of retroperitoneal lymph node metastasis in gastrointestinal tumors[J]. Guid China Med, 2012, 10(17): 78-81. DOI: 10.3969/j.issn.1671-8194.2012.17.050. [20] 王贵齐, 魏文强. 上消化道癌筛查和早诊早治项目的新转变: 机会性筛查[J]. 中华预防医学杂志, 2019, 53(11): 1084-1087. DOI: 10.3760/cma.j.issn.0253-9624.2019.11.002.Wang GQ, Wei WQ. A new transition of the screening, early diagnosis and early treatment project of the upper gastrointestinal cancer: opportunistic screening[J]. Chin J Prev Med, 2019, 53(11): 1084-1087. DOI: 10.3760/cma.j.issn.0253-9624.2019.11.002. [21] 孙可欣, 郑荣寿, 张思维, 等. 2015年中国分地区恶性肿瘤发病和死亡分析[J]. 中国肿瘤, 2019, 28(1): 1-11. DOI: 10.11735/j.issn.1004-0242.2019.01.A001.Sun KX, Zheng XR, Zhang SW, et al. Report of cancer incidence and mortality in different areas of China, 2015[J]. China Cancer, 2019, 28(1): 1-11. DOI: 10.11735/j.issn.1004-0242.2019.01.A001. [22] Gu MJ, Huang QC, Bao CZ, et al. Attributable causes of colorectal cancer in China[J]. BMC Cancer, 2018, 18(1): 38. DOI: 10.1186/s12885-017-3968-z. [23] Liu X, Bi Y, Wang H, et al. Different trends in colorectal cancer mortality between age groups in China: an age-period-cohort and Joinpoint analysis[J]. Public Health, 2019, 166: 45-52. DOI: 10.1016/j.puhe.2018.08.007. -





 下载:
下载: