Association between abnormal renal function and sleep among male coal workers in Xingtai City
-
摘要:
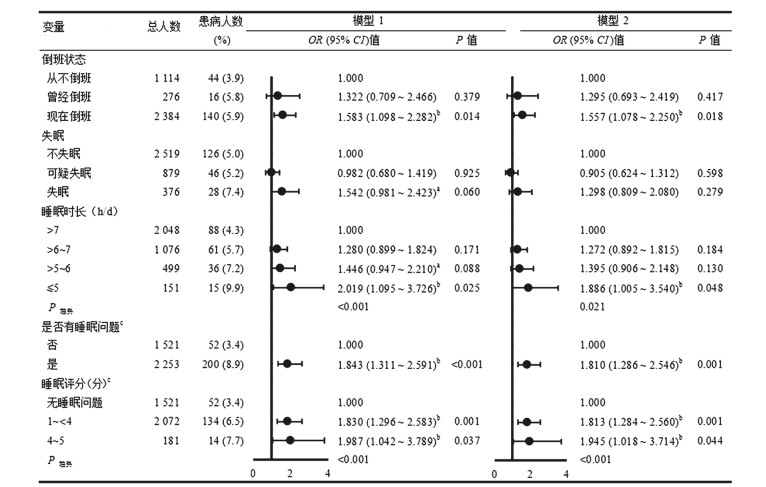
目的 探讨邢台市男性煤炭工人睡眠与肾功能异常之间的关系,为男性煤炭工人的肾脏疾病防治提供理论依据。 方法 采用现况研究,收集河北省邢台市2家煤炭公司的3 774名井下男性煤炭工人的问卷和血生化指标等信息。采用多因素Logistic回归分析模型分析倒班、睡眠时长和失眠或睡眠评分与肾功能异常的关系。 结果 男性工人的肾功能异常检出率为5.3%,倒班、睡眠时长≤5 h、失眠的工人占比分别为63.2%、4.0%及10.0%。调整年龄、睡眠时长、倒班状态、失眠等因素后,多因素Logistic回归分析模型分析结果显示,现在倒班(OR=1.557, 95% CI: 1.078~2.250, P=0.018)、睡眠时长≤5 h(OR=1.886, 95% CI: 1.005~3.540, P=0.048)、有睡眠问题组(OR=1.810, 95% CI: 1.286~2.546, P=0.001)与肾功能异常的联系减弱,失眠与肾功能异常联系无统计学意义(P=0.279)。根据倒班状态进行分层分析,调整相关混杂因素后发现,现在倒班的煤炭工人肾功能异常患病风险随睡眠评分等级的增加而增加(P趋势=0.001)。 结论 每天睡眠时长≤5 h、现在倒班与男性煤炭工人肾功能异常独立相关,且睡眠问题越严重,肾功能异常的患病风险越高。 Abstract:Objective To explore the relationship between sleep duration, insomnia, shift work and kidney function among male coal workers in Xingtai City, and to provide a theoretical basis for the prevention and treatment of kidney diseases in male coal workers. Methods A cross-sectional study was uesd. Relevant information was collected through questionnaires and blood biochemical analysis. Mutiple Logistic regression model was used to explore the relationship between abnormal renal function and sleep, night shift work. Results The prevalence of abnormal renal function among male workers in coal enterprises was 5.3%. The proportion of individuals with night shift work, sleep duration ≤5 h and insomnia were 63.2%, 4.0%, and 10.0% respectively. After adjusting for age, sleep duration, shift work and and insomnia, the results of multivariate Logistic regression analysis model showed that the relationship between shift work (OR=1.557, 95% CI: 1.078-2.250, P=0.018), sleep duration ≤ 5 h (OR=1.886, 95% CI: 1.005-3.540, P=0.048), group with sleep problems (OR=1.810, 95% CI: 1.286-2.546, P=0.001) and abnormal renal function was attenuated. The relationship between insomnia and abnormal renal function was not statistically significant (P=0.279). According to the stratified analysis of the shift work, after adjusting the related abnormal renal function among shift workers (Ptrend=0.001). Conclusions Sleep and shift work independently associate with abnormal renal function in male coal workers. The risk of abnormal kidney function increases with the severity of sleep problems. -
Key words:
- Sleep duration /
- Insomnia /
- Shift work /
- Coal worker /
- Abnormal renal function
-
表 1 2018年7月—2018年8月邢台市男性煤炭工人的基本特征[n (%)]
Table 1. Basic characteristic of male coal workers in Xingtai City from July to August 2018 [n (%)]
特征 总人群(N=3 774) 肾功能异常(n=200) χ2值 P值 特征 总人群(N=3 774) 肾功能异常(n=200) χ2值 P值 年龄(岁) a 160.326 b < 0.001 糖尿病家族史 2.777 0.096 20~ < 40 1 880(49.8) 28(1.5) 无 3 312(87.8) 168(5.1) 40~ < 50 1 042(27.6) 58(5.6) 有 462(12.2) 32(6.9) ≥50 852(22.6) 114(13.4) BMI(kg/m2) 35.354 b < 0.001 倒班状态 5.343 b 0.021 < 24 1 196(31.7) 32(2.7) 从不倒班 1 114(29.5) 44(3.9) 24~ < 28 1 620(42.9) 87(5.4) 曾经倒班 276(7.3) 16(5.8) ≥28 958(25.4) 81(8.5) 现在倒班 2 384(63.2) 140(5.9) 中心性肥胖 40.604 < 0.001 睡眠时长(h/d) 13.771 b 0.004 否 2 815(74.6) 111(3.9) ≤5 151(4.0) 15(9.9) 是 959(25.4) 89(9.3) >5~6 499(13.2) 36(7.2) 高血压 23.758 < 0.001 >6~7 1 076(28.5) 61(5.7) 否 2 367(62.7) 93(3.9) >7~8 1 294(34.3) 60(4.6) 是 1 407(37.3) 107(7.6) >8~9 557(14.8) 21(3.8) 糖尿病 0.218 0.641 >9 197(5.2) 7(3.6) 否 3 610(95.7) 190(5.3) 失眠 2.876 b 0.090 是 164(4.3) 10(6.1) 不失眠 2 519(66.7) 126(5.0) 高尿酸血症 31.040 < 0.001 可疑失眠 879(23.3) 46(5.2) 否 3 029(80.3) 130(4.3) 失眠 376(10.0) 28(7.4) 是 745(19.7) 70(9.4) 睡眠评分(分) 17.705 b < 0.001 血脂异常 23.503 < 0.001 无睡眠问题 1 521(40.3) 52(3.4) 否 2 765(73.3) 117(4.2) 1~<4 2 072(54.9) 134(6.5) 是 1009(26.7) 83(8.2) 4~5 181(4.8) 14(7.7) 肝酶异常 3.074 0.080 教育水平 33.375 b < 0.001 否 2 985(79.1) 168(5.6) 小学及以下 47(1.3) 6(12.8) 是 789(20.9) 32(4.1) 初中(技校)及高中(中专) 2 745(72.7) 175(6.4) 是否打鼾 11.997 0.001 本科(大专)及以上 982(26.0) 19(1.9) 否 1 808(47.9) 72(4.0) 吸烟情况 7.410 0.025 是 1 966(52.1) 128(6.5) 从不 1 490(39.5) 81(5.4) 是否服用降压药物 48.307 < 0.001 曾经 249(6.6) 22(8.8) 否 3 416(90.5) 153(4.5) 现在 2 035(53.9) 97(4.8) 是 358(9.5) 47(13.1) 饮酒情况 6.462 0.040 是否服用降糖药物 3.065 0.087 从不 728(19.3) 50(6.9) 否 3 729(98.8) 195(5.2) 曾经 163(4.3) 12(7.4) 是 45(1.2) 5(11.1) 现在 2 883(76.4) 138(4.8) 是否打胰岛素 6.411 0.022 身体锻炼次数(次/周) 5.345 0.021 否 3 720(98.6) 193(5.2) 从不 1 568(41.5) 76(4.8) 是 54(1.4) 7(13.0) < 4 1 134(30.0) 48(4.2) 是否服用中药 7.284 0.035 ≥4 1 072(28.5) 76(7.1) 否 3 760(99.6) 197(5.2) 高血压家族史 1.840 0.175 是 14(0.4) 3(21.4) 无 2 433(64.5) 120(4.9) 是否服用治疗睡眠药物 1.714 0.173 有 1 341(35.5) 80(6.0) 否 3 706(98.2) 194(5.2) 是 68(1.8) 6(8.8) 注:a 20~30年龄组无患病工人,将20~<30组和≥30组合并进行分析; b使用趋势性χ2检验。 表 2 睡眠评分和倒班状态的交互作用与肾功能异常关联性的交互作用分析
Table 2. Analysis of the interaction between sleep score and night shift work
睡眠评分 现在倒班
OR (95% CI)值从不或曾经倒班
OR (95% CI)值P相乘交互 RERI (95% CI)值 AP (95% CI)值 无睡眠问题 1.000 1.000 0.118 1.880(-0.025~3.785) 0.791(0.515~1.066) 1~3 2.171(1.437~3.279) 1.042(0.527~2.060) >3 2.239(1.086~4.618) 1.017(0.197~5.244) P趋势 0.001 0.923 注:调整变量同图 1的模型1。 -
[1] Webster AC, Nagler EV, Morton RL, et al. Chronic kidney disease[J]. Lancet, 2017, 389(10075): 1238-1252. DOI: 10.1016/s0140-6736(16)32064-5. [2] 龚珂, 秦东芳, 王学晶. 肾小球滤过率测量方法的研究进展[J]. 中华检验医学杂志, 2020, 43(4): 502-506. DOI: 10.3760/cma.j.cn114452-20190514-00293.Gong K, Qin DF, Wang XJ, et al. Research progress in the measurement of glomerular filtration rate[J]. Chin J Lab Med, 2020, 43(4): 502-506. DOI: 10.3760/cma.j.cn114452-20190514-00293. [3] Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review[J]. JAMA, 2015, 313(8): 837-846. DOI: 10.1001/jama.2015.0602. [4] Liu T, Liu S. The impacts of coal dust on miners' health: a review[J]. Environ Res, 2020, 190: 109849. DOI: 10.1016/j.envres.2020.109849. [5] James SM, Honn KA, Gaddameedhi S, et al. Shift work: disrupted circadian rhythms and sleep-implications for health and well-being[J]. Curr Sleep Med Rep, 2017, 3(2): 104-112. DOI: 10.1007/s40675-017-0071-6. [6] K Pavlova M, Latreille V. Sleep disorders[J]. Am J Med, 2019, 132(3): 292-299. DOI: 10.1016/j.amjmed.2018.09.021. [7] 苏畅, 王惠君, 张兵. 2015年中国十五省(自治区、直辖市)18~64岁成年居民睡眠状况[J]. 卫生研究, 2020, 49(3): 498-501. DOI: 10.19813/j.cnki.weishengyanjiu.2020.03.027.Su C, Wang HJ, Zhang B. Sleep status of adult residents aged 18 to 64 years old in 15 provinces of China in 2015[J]. J Hygiene Res, 2020, 49(3): 498-501. DOI: 10.19813/j.cnki.weishengyanjiu.2020.03.027. [8] Watson NF, Badr MS, Belenky G, et al. Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: methodology and discussion[J]. Sleep, 2015, 38(8): 1161-1183. DOI: 10.5664/jcsm.4950. [9] Bo Y, Yeoh EK, Guo C, et al. Sleep and the risk of chronic idneky disease: a cohort study[J]. J Clin Sleep Med, 2019, 15(3): 393-400. DOI: 10.5664/jcsm.7660. [10] Firsov D, Bonny O. Circadian rhythms and the kidney[J]. Nat Rev Nephrol, 2018, 14(10): 626-635. DOI: 10.1038/s41581-018-0048-9. [11] Drawz P, Rahman M. Chronic kidney disease[J]. Ann Intern Med, 2015, 162(11): ITC1-16. DOI: 10.7326/aitc201506020. [12] 张生奎, 王镇德, 杨荔, 等. 倒班作业与高尿酸血症的剂量反应关系研究[J]. 中华疾病控制杂志, 2018, 22(11): 1123-1127. DOI: 10.16462/j.cnki.zhjbkz.2019.11.011.Zhang SK, Wang ZD, Yang L, et al. Dose-response relationship between shift work and hyperuricemia[J]. Chin J Dis Control Prev, 2018, 22(11): 1123-1127. DOI: 10.16462/j.cnki.zhjbkz.2019.11.011. [13] Vanderweele TJ, Knol MJ. A tutorial on interaction[J]. Epidemiol Methods, 2014, 3(1): 33-72. DOI: 10.1515/em-2013-0005. [14] Boivin DB, Boudreau P. Impacts of shift work on sleep and circadian rhythms[J]. Pathologie Biologie, 2014, 62(5): 292-301. DOI: 10.1016/j.patbio.2014.08.001. [15] Li JJ, Huang Z, Hou JH, et al. Sleep and CKD in Chinese adults: a cross-sectional study[J]. Clin J Am Soc Nephrol, 2017, 12(6): 885-892. DOI: 10.2215/cjn.09270816. [16] Turek NF, Ricardo AC, Lash JP. Sleep disturbances as nontraditional risk factors for development and progression of CKD: review of the evidence[J]. Am J Kidney Dis, 2012, 60(5): 823-833. DOI: 10.1053/j.ajkd.2012.04.027. [17] Uhm JY, Kim HR, Kang GH, et al. The association between shift work and chronic kidney disease in manual labor workers using data from the Korea national health and nutrition examination survey (KNHANES 2011-2014)[J]. Ann Occup Environ Med, 2018, 30: 69. DOI: 10.1186/s40557-018-0279-z. [18] Ricardo AC, Knutson K, Chen J, et al. The association of sleep duration and quality with CKD progression[J]. J Am Soc Nephrol, 2017, 28(12): 3708-3715. DOI: 10.1681/asn.2016121288. [19] McMullan CJ, Curhan GC, Forman JP. Association of short sleep duration and rapid decline in renal function[J]. Kidney Int, 2016, 89(6): 1324-1330. DOI: 10.1016/j.kint.2015.12.048. [20] Bin YS. Is sleep quality more important than sleep duration for public health?[J]. Sleep, 2016, 39(9): 1629-1630. DOI: 10.5665/sleep.6078. -





 下载:
下载: