Analysis of comprehensive surveillance results of respiratory tract infectious diseases in Taizhou, 2012-2019
-
摘要:
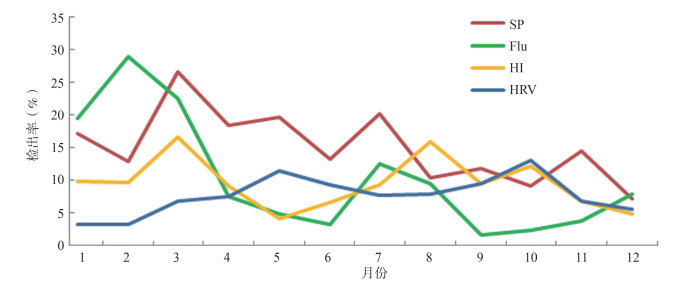
目的 了解泰州市流感样病例(influenza-like illness, ILI)和严重急性呼吸道感染(severe acute respiratory infection, SARI)病例的流行病学特征,为科学制定防控策略提供依据。 方法 收集哨点医院ILI病例和SARI病例基本信息并采集咽拭子标本,用PCR法开展13种呼吸道病原体检测,用χ2检验进行统计学分析。 结果 2012年4月―2019年12月ILI就诊百分比(ILI%)和SARI就诊百分比(SARI%)分别为7.27%和2.44%,具有秋冬季流行高峰。共检测956例ILI病例和557例SARI病例的标本,二者的病原阳性检出率分别为50.84%(486/956)、39.14%(218/557)。肺炎链球菌(Streptococcus pneumoniae, SP)、流感病毒(influenza virus, Flu)、流感嗜血杆菌(Haemophilus influenzae, HI)、人鼻病毒(Human rhinovirus, HRV)为优势病原体,其检出率分别为14.81%、9.25%、9.39%、7.73%。总混合感染率为30.11%(212/704),主要为SP合并其他病原体感染。低年龄组病原体检出阳性率高于高年龄组,0~ < 5岁儿童的检出率达34.83%(χ2=54.47, P < 0.001)。冠状病毒(human coronavirus, HCoV)的检出率为2.12%,以HCoV-OC43亚型为主(46.88%),各亚型季节分布不明显。 结论 泰州市哨点医院呼吸道综合监测发病呈秋冬季的流行高峰,主要病原体为SP、Flu、HI、HRV,15岁以下年龄组检出率较高,应针对重点人群采取综合性呼吸道疾病防控措施。 Abstract:Objective To understand the epidemiological characteristics of influenza-like illness (ILI) cases and severe acute respiratory infection (SARI) cases in Taizhou, so as to provide a basis for scientific prevention and control strategies. Methods The basic information of ILI and SARI cases and throat swab specimens were collected from the sentinel hospital and 13 respiratory pathogens were detected by RT-PCR method.χ2 test was used as statistical analysis method. Results From April 2012 to December 2019, with epidemic peaks in autumn and winter, the percentages of ILI visits (ILI%) and SARI visits (SARI%) were 7.27% and 2.44%, respectively. Finally, 956 ILI case specimens and 557 SARI case specimens were detected. The positive detection rates of the two types of cases were 50.84% (486/956) and 39.14% (218/557), separately. Streptococcus pneumoniae (SP), influenza virus (Flu), Haemophilus influenzae (HI) and Human rhinovirus (HRV) were the dominant pathogens in Taizhou city from April 2012 to December 2019, and their detection rates were 14.81%, 9.25%, 9.39% and 7.73%, respectively. The total mixed infection rate was 30.11% (212/704), which was mainly caused by SP complicated with other pathogenic infections. The positive rate of pathogen detection in the low-age group was higher than that in the high-age group, and the detection rate of children under 5 years old was 34.83% (χ2=54.47, P < 0.001). The detection rate of human coronavirus (HCoV) was 2.12%, with HCoV-OC43 subtype mainly (46.88%), and each subtype has no obvious seasonal distribution characteristics. Conclusions The incidence of comprehensive respiratory tract surveillance in sentinel hospitals in Taizhou City showed that the peak of the epidemic was in autumn and winter, and SP, Flu, HI, and HRV were main pathogens in this area. In the age group under 15 years old, the detection rate was higher. Comprehensive respiratory disease prevention and control measures should be taken for key populations. -
Key words:
- Respiratory infection /
- Pathogenic /
- Surveillance /
- Epidemic characteristics
-
表 1 2012―2019年泰州市呼吸道感染性疾病综合监测病原体检出情况分布
Table 1. Distribution of pathogens detected in comprehensive surveillance of respiratory tract infectious diseases in Taizhou from 2012 to 2019
病原体类型 ILI病例 SARI病例 阳性数(例) 检出率(%) 阳性数(例) 检出率(%) SP 169 17.68 55 9.87 Flu 107 11.19 33 5.92 HI 102 10.70 40 7.18 HRV 92 9.62 25 4.49 ADV 64 6.69 10 1.80 HSV 39 4.08 27 4.85 RSV 29 3.03 20 3.59 PIV 26 2.72 17 3.05 HCoV 25 2.62 7 1.26 HMPV 11 1.15 6 1.08 HBV 9 0.94 6 1.08 MP 9 0.94 33 5.92 CPN 2 0.21 4 0.72 合计 684 71.57 283 50.81 表 2 2012―2019年泰州市呼吸道感染性疾病综合监测病原体分年度构成(%)
Table 2. Annual composition of pathogens in the comprehensive monitoring of respiratory tract infectious diseases in Taizhou from 2012 to 2019 (%)
病原体类型 2012年 2013年 2014年 2015年 2016年 2017年 2018年 2019年 χ2值a P值 Flu 24.68 7.27 33.22 16.20 5.48 4.59 19.44 17.67 0.074 1.000 PIV 6.56 2.77 6.40 11.85 7.08 0.42 2.78 4.43 RSV 0.32 3.82 14.03 17.96 4.49 2.83 13.40 3.50 ADV 2.24 10.56 8.25 7.41 10.51 10.88 2.12 0.72 HRV 15.91 17.27 6.79 5.56 8.60 7.59 12.25 5.68 HMPV 0.64 0.00 5.78 6.85 0.00 2.77 2.94 2.17 HCoV 2.16 3.90 0.00 0.00 3.96 4.95 6.45 0.72 HBV 3.99 0.00 0.00 2.50 0.00 0.85 4.25 1.65 HSV 11.83 2.21 0.00 10.56 11.28 3.19 10.62 5.35 SP 23.19 45.60 10.49 16.76 17.44 40.16 11.52 14.86 HI 6.32 0.56 15.04 1.85 23.84 17.07 12.83 27.78 CPN 1.52 2.21 0.00 2.50 1.22 0.00 0.00 0.00 MP 0.64 3.82 0.00 0.00 6.10 4.69 1.39 15.46 合计 100.00 100.00 100.00 100.00 100.00 100.00 100.00 100.00 注:a表示χ2值为2012―2019年间进行构成比比较的结果。 表 3 2012―2019年泰州市呼吸道感染性疾病综合监测病原体分年度构成(%)
Table 3. Annual composition of pathogens in the comprehensive monitoring of respiratory tract infectious diseases in Taizhou from 2012 to 2019 (%)
病原体 年龄组 χ2值 P值 0~<5岁(n=700) 5~<15岁(n=473) 15~<25岁(n=46) 25~<60岁(n=122) ≥60岁(n=172) 合计 Flu-A 44(6.29) 32(6.77) 3(6.52) 7(5.74) 12(6.98) 98(6.48) 1.48 0.836 Flu-B 10(1.43) 26(5.50) 0(0.00) 2(1.64) 4(2.33) 42(2.78) 19.27 < 0.001 PIV-I 5(0.71) 1(0.21) 2(4.35) 0(0.00) 0(0.00) 8(0.53) 8.26 0.044 PIV-II 1(0.14) 0(0.00) 1(2.17) 0(0.00) 0(0.00) 2(0.13) 7.14 0.098 PIV-III 19(2.71) 4(0.85) 1(2.17) 1(0.82) 3(1.74) 28(1.85) 6.06 0.152 PIV-IV 3(0.43) 2(0.42) 0(0.00) 0(0.00) 0(0.00) 5(0.33) 1.01 1.000 RSV 41(5.86) 6(1.27) 0(0.00) 1(0.23) 1(0.58) 49(3.24) 32.09 < 0.001 ADV 37(5.29) 32(6.77) 2(4.35) 0(0.00) 3(1.74) 74(4.89) 20.52 < 0.001 HRV 75(10.71) 33(6.98) 2(4.35) 2(1.64) 5(2.91) 117(7.73) 25.5 < 0.001 HMPV 9(1.29) 6(1.27) 0(0.00) 0(0.00) 2(1.16) 17(1.12) 1.14 0.863 HCoV 21(3.00) 7(1.48) 1(2.17) 1(0.82) 2(1.16) 32(2.12) 4.49 0.303 HBV 13(1.86) 1(0.21) 0(0.00) 1(0.82) 0(0.00) 15(0.99) 8.77 0.041 HSV 24(3.43) 20(4.23) 2(4.35) 11(9.02) 9(5.23) 66(4.36) 6.79 0.172 SP 124(17.71) 77(16.28) 4(8.70) 9(7.38) 10(5.81) 224(14.81) 23.23 < 0.001 HI 78(11.14) 46(9.73) 2(4.35) 6(4.92) 10(5.81) 142(9.39) 10.52 0.038 CPN 1(0.14) 3(0.63) 0(0.00) 0(0.00) 2(1.16) 6(0.40) 4.65 0.249 MP 22(3.14) 18(3.81) 1(2.17) 1(0.82) 0(0.00) 42(2.78) 14.14 < 0.001 合计 527(34.83) 314(20.75) 23(1.52) 42(2.78) 63(4.16) 969(64.04) 54.47 < 0.001 表 4 2012―2019年泰州市ILI病例和SARI病例混合感染的主要类型
Table 4. The main types of co-infection of ILI cases and SARI cases in Taizhou from 2012 to 2019
混合感染类型 例数(例) 构成比(%) SP+HRV 20 9.43 SP+Flu-A 16 7.55 SP+ADV 15 7.08 SP+HI 15 7.08 SP+HSV 7 3.30 SP+HSV+HI 7 3.30 SP+HCoV 7 3.30 SP+HI+Flu-B 5 2.36 其他 120 56.60 合计 212 100.00 -
[1] 杨娟, 郑亚明, 刘欣欣, 等. 中国哨点监测住院严重急性呼吸道感染病例经济负担分析[J]. 国际病毒学杂志, 2015, 22(6): 361-366. DOI: 10.3760/cma.j.issn.1673-4092.2015.06.001.Yang J, Zheng YM, Liu XX, et al. Analysis on the economic burden of severe acute respiratory infection inpatients from sentinel hospitals in China[J]. Int J Virol, 2015, 22(6): 361-366. DOI: 10.3760/cma.j.issn.1673-4092.2015.06.001. [2] 顾文超, 唐海丰, 李晓君, 等. 上海市普陀区515例住院严重急性呼吸道感染病例监测结果分析[J]. 职业与健康, 2020, 36(11): 1492-1495. DOI: 10.13329/j.cnki.zyyjk.2020.0395.Gu WC, Tang HF, Li XJ, et al. Analysis on surveillance results of 515 inpatients with severe acute respiratory infection in Putuo District of Shanghai[J]. Occup Heal, 2020, 36(11): 1492-1495. DOI: 10.13329/j.cnki.zyyjk.2020.0395. [3] 马文瑛, 张慧, 姜中毅, 等. 兰州市2009—2013年住院病例中严重急性呼吸道感染病毒病原学监测研究[J]. 中国病毒病杂志, 2015, 5(4): 281-286. DOI: 10.16505/j.2095-0136.2015.04.011.Ma WY, Zhang H, Jiang ZY, et al. Viral etiology and clinical features of severe acute respiratory infection (SARI) among hospitalized patients in Lanzhou City of China from 2009 to 2013[J]. Chin J Viral Dis, 2015, 5(4): 281-286. DOI: 10.16505/j.2095-0136.2015.04.011. [4] 唐海丰, 李晓君, 胡焰, 等. 上海市普陀区监测点医院697例急性上呼吸道感染病例监测结果研究[J]. 现代医药卫生, 2020, 36(1): 47-49, 52. DOI: 10.3969/j.issn.1009-5519.2020.01.015.Tang HF, Li XJ, Hu Y, et al. Study on surveillance results of 697 cases of acute upper respiratory tract infection in hospital of Shanghai Putuo District[J]. Mod Med Heal, 2020, 36(1): 47-49, 52. DOI: 10.3969/j.issn.1009-5519.2020.01.015. [5] 李翔, 方斌, 叶国军, 等. 武汉市2012—2015年发热呼吸道症候群监测病例病毒检测结果分析[J]. 中华疾病控制杂志, 2018, 22(8): 833-836. DOI: 10.16462/j.cnki.zhjbkz.2018.08.017.Li X, Fang B, Ye GJ, et al. Analysis on the detection results of case surveillance of febrile respiratory syndrome in Wuhan City from 2012 to 2015[J]. Chin J Dis Control Prev, 2018, 22(8): 833-836. DOI: 10.16462/j.cnki.zhjbkz.2018.08.017. [6] 中国疾病预防控制中心. 中国流感疫苗预防接种技术指南(2019—2020)[J]. 中国病毒病杂志, 2019, 9(6): 419-428. DOI: 10.16505/j.2095-0136.2019.0085.Chinese Center for Disease Control and Prevention. Technical guidelines for influenza vaccination in China, 2019-2020[J]. Chin J Viral Dis, 2019, 9(6): 419-428. DOI: 10.16505/j.2095-0136.2019.0085. [7] Shooraj F, Mirzaei B, Mousavi SF, et al. Clonal diversity of Haemophilus influenzae carriage isolated from under the age of 6 years children[J]. BMC Res Notes, 2019, 12(1): 565. DOI: 10.1186/s13104-019-4603-7. [8] 吕志勇, 董方, 宋文琪, 等. 儿童感染肺炎链球菌的血清型和耐药性分析[J]. 中国感染与化疗杂志, 2020, 20(4): 417-422. DOI: 10.16718/j.1009-7708.2020.04.014.Lv ZY, Dong F, Song WQ, et al. Analysis of the serotype distribution and antimicrobial resistance of Streptococcus pneumoniae isolated from children[J]. Chin J Infect Chemother, 2020, 20(4): 417-422. DOI: 10.16718/j.1009-7708.2020.04.014. [9] Jacobs SE, Lamson DM, St George K, et al. Human rhinoviruses[J]. Clin Microbiol Rev. 2013, 26(1): 135-162. DOI: 10.1128/CMR.00077-12. [10] World Health Organization. WHO COVID-19 Dashboard[EB/OL]. (2020-08)[2020-08-27]. https://covid19.who.int/. [11] Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019[J]. N Engl J Med, 2020, 382(8): 727-733. DOI: 10.1056/nejmoa2001017. -





 下载:
下载: