The prevalence of the metabolic associated fatty liver disease among residents aged 30 to 79 in Dongguan City of Guangdong Province
-
摘要:
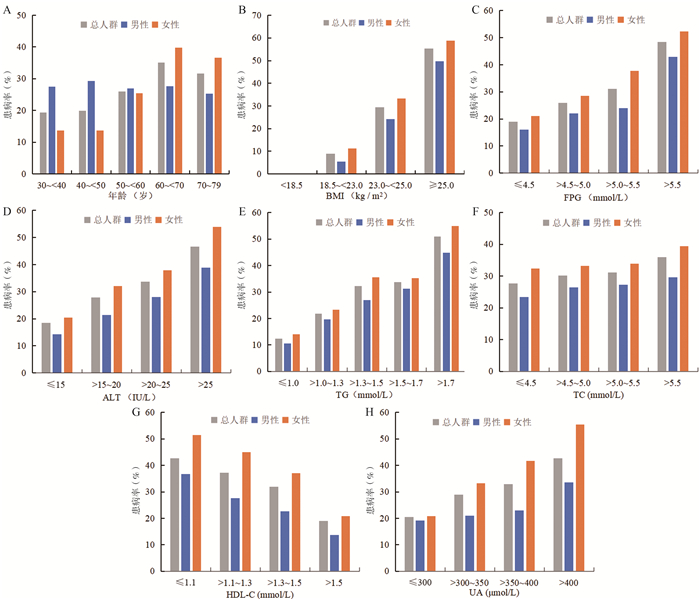
目的 了解广东省东莞市30~79岁居民代谢相关脂肪性肝病(metabolic associated fatty liver disease, MAFLD) 的患病情况,探讨不同人群特征对MAFLD患病的影响。 方法 利用华南区域自然人群慢性病前瞻性队列研究在广东省东莞市的基线调查数据,包括体格检查、腹部超声检查和临床检验,共纳入8 670名研究对象。参考国际专家小组共识声明判断MAFLD患病情况。采用多因素Logistic回归分析模型分析男、女性MAFLD患病的影响因素。 结果 东莞市30~79岁居民MAFLD患病率为31.85%。男性各年龄段MAFLD患病率的差异无统计学意义(χ2 =2.958, P=0.565),女性患病率随年龄的增加而呈线性增长的趋势(χ趋势2=81.429, P<0.001)。MAFLD患病率随BMI、FPG、ALT、TG、TC、血尿酸(uric acid, UA)等代谢指标的升高而升高,随HDL-C的升高而降低。多因素Logistic回归分析模型结果显示年龄≥50岁的女性患MAFLD风险较高(OR=2.37, 95% CI: 1.74~3.23, P<0.001)。 结论 东莞市30~79岁居民MAFLD患病率为31.85%,与BMI、FPG、TG、TC等代谢指标之间呈线性关联。年龄≥50岁可能是女性患MAFLD的危险因素。 Abstract:Objective To explore the prevalence of metabolic associated fatty liver disease (MAFLD) and the impact of different characteristics among residents aged 30 to 79 in Dongguan City of Guangdong Province. Methods Baseline data were collected in Dongguan City, Guangdong Province of South China Cohort, including physical examination, ultrasound, and laboratory tests. According to the inclusion and exclusion criteria, we included 8 670 participants and defined the status of MAFLD referred to the consensus statement of international experts. Multivariate Logistic regression analysis model was used to analyze the factors according to gender. Results The prevalence of MAFLD was 31.85% among residents aged 30 to 79 in Dongguan City. The prevalence was similar among males in different age groups (χ2 =2.958, P=0.565), while it linearly increased with age in females (χtrend2=81.429, P < 0.001). The prevalence showed a linear increase with BMI, FPG, ALT, TG, TC, uric acid (UA) while a linear decrease with HDL-C. The results of multivariate Logistic regression analysis model showed that females ≥50 years old had a higher risk of MAFLD (OR=2.37, 95% CI: 1.74~3.23, P < 0.001). Conclusions The prevalence of MAFLD was 31.85% among residents aged 30 to 79 in Dongguan City, and there was a linear association between the prevalence of MAFLD and various metabolic indices including BMI, FPG, TG, and TC. Age ≥50 years old may be a risk factor of MAFLD in females. -
Key words:
- Metabolic associated fatty liver disease /
- Prevalence /
- Residents
-
表 1 2018―2019年广东省东莞市30~79岁调查对象的基本特征[n(%)]
Table 1. Basic characteristics of participants aged 30 to 79 in Dongguan City, Guangdong Province from 2018 to 2019 [n(%)]
变量 总人群(N=8 670) 男性(n=3 525) 女性(n=5 145) t/t’/Z/χ2值 P值 年龄[(x±s), 岁] 65.33±9.34 65.55±9.42 65.18±9.28 -1.847 0.065 高血压 4.436 0.035 有 3 947(46.07) 1 551(44.70) 2 396(47.01) 无 4 620(53.93) 1 919(55.30) 2 701(52.99) 超重/肥胖 0.144 0.705 是 5 498(63.41) 2 227(63.18) 3 271(63.58) 否 3 172(36.59) 1 298(36.82) 1 874(36.42) 糖尿病 2.075 0.150 是 686(8.10) 296(8.62) 390(7.75) 无 7 783(91.90) 3 139(91.38) 4 644(92.25) 代谢功能失调 369.934 <0.001 是 5 618(64.80) 1 864(52.88) 3 754(72.96) 否 3 052(35.20) 1 661(47.12) 1 391(27.04) WC[(x±s), cm] 85.49±9.48 86.55±9.09 84.76±9.68 -8.704 <0.001 BMI[(x±s), kg/m2] 24.30±3.47 24.11±3.21 24.42±3.63 4.108 <0.001 SBP[(x±s), mm Hg] 137.31±19.35 136.19±18.13 138.07±20.11 4.499 <0.001 DBP[(x±s), mm Hg] 81.05±10.66 81.96±10.72 80.43±10.57 -6.537 <0.001 FPG[M(P25, P75), mmol/L] 4.98(4.57, 5.57) 4.99(4.57, 5.59) 4.97(4.57, 5.56) -0.855 0.393 ALT[M(P25, P75), IU/L] 20.00(15.00, 26.10) 21.00(16.00, 28.00) 19.00(14.90, 25.00) -10.882 <0.001 AST[M(P25, P75), IU/L] 22.00(18.80, 26.31) 22.00(19.00, 27.00) 22.00(18.43, 26.00) -3.710 <0.001 TBIL[M(P25, P75), μmol/L] 13.20(10.60, 16.59) 14.20(11.20, 17.80) 12.70(10.20, 15.70) -14.094 <0.001 TG[M(P25, P75), mmol/L] 1.38(0.99, 2.02) 1.33(0.94, 1.93) 1.43(1.02, 2.06) -5.909 <0.001 TC[(x±s), mmol/L] 5.28±1.08 5.04±1.04 5.45±1.07 17.330 <0.001 HDL-C[(x±s), mmol/L] 1.37±0.34 1.27±0.32 1.43±0.33 23.190 <0.001 LDL-C[(x±s), mmol/L] 3.26±0.92 3.16±0.90 3.32±0.93 8.264 <0.001 血尿素[M(P25, P75), mmol/L] 5.44(4.57, 6.51) 5.57(4.67, 6.67) 5.37(4.51, 6.40) -6.590 <0.001 血肌酐[M(P25, P75), μmol/L] 72.00(61.00, 85.00) 85.00(75.00, 97.00) 64.00(56.90, 73.00) -54.159 <0.001 UA[(x±s), μmol/L] 364.69±98.50 401.51±96.88 339.53±91.43 -29.510 <0.001 表 2 2018―2019年广东省东莞市不同性别、年龄调查对象MAFLD患病率
Table 2. The prevalence of MAFLD according to gender and age group among participants in Dongguan City, Guangdong Province from 2018 to 2019
年龄组(岁) 性别 总人数 患病人数 患病率(%) χ2值 P值 30~<40 男 91 25 27.47 6.484 0.011 女 131 18 13.74 40~<50 男 225 66 29.33 20.797 <0.001 女 337 46 13.65 50~<60 男 286 77 26.92 0.207 0.649 女 398 101 25.38 60~<70 男 1 620 448 27.65 65.079 <0.001 女 2 584 1 030 39.86 70~79 男 1 303 329 25.25 44.133 <0.001 女 1 695 621 36.64 表 3 2018―2019年广东省东莞市男、女性MAFLD患病的多因素Logistic回归分析
Table 3. Multivariate Logistic regression for MAFLD according to gender among participants in Dongguan City, Guangdong Province from 2018 to 2019
自变量 男性 女性 β值 OR(95% CI)值 P值 β值 OR(95% CI)值 P值 年龄≥50(岁) 0.218 1.24(0.92~1.69) 0.161 0.862 2.37(1.74~3.23) <0.001 超重/肥胖 1.750 5.75(4.28~7.34) <0.001 1.547 4.70(3.86~5.71) <0.001 糖尿病 0.815 2.26(1.70~3.01) <0.001 0.784 2.19(1.71~2.81) <0.001 WC异常 0.952 2.59(2.15~3.13) <0.001 0.897 2.45(1.98~3.04) <0.001 血压异常 0.223 1.25(1.02~1.54) 0.035 0.207 1.23(1.04~1.45) 0.013 TG异常 0.871 2.39(1.99~2.87) <0.001 0.925 2.52(2.18~2.92) <0.001 HDL-C异常 0.075 1.08(0.88~1.33) 0.477 0.346 1.41(1.22~1.63) <0.001 ALT异常 0.655 1.93(1.17~3.17) 0.010 0.960 2.61(1.98~3.44) <0.001 高尿酸血症 0.341 1.41(1.18~1.68) <0.001 0.537 1.71(1.49~1.97) <0.001 -
[1] Nan Y, An J, Bao J, et al. The Chinese Society of Hepatology position statement on the redefinition of fatty liver disease[J]. J Hepatol, 2021, 75(2): 454-461. DOI: 10.1016/j.jhep.2021.05.003. [2] Zhou F, Zhou J, Wang W, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis[J]. Hepatology, 2019, 70(4): 1119-1133. DOI: 10.1002/hep.30702. [3] Eslam M, Sanyal AJ, George J. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease[J]. Gastroenterology, 2020, 158(7): 1999-2014. DOI: 10.1053/j.gastro.2019.11.312. [4] Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement[J]. J Hepatol, 2020, 73(1): 202-209. DOI: 10.1016/j.jhep.2020.03.039. [5] Xian YX, Weng JP, Xu F. MAFLD vs. NAFLD: shared features and potential changes in epidemiology, pathophysiology, diagnosis, and pharmacotherapy[J]. Chin Med J (Engl), 2020, 134(1): 8-19. DOI: 10.1097/CM9.0000000000001263. [6] Nabi O, Lacombe K, Boursier J, et al. Prevalence and risk factors of nonalcoholic fatty liver disease and advanced fibrosis in general population: the French Nationwide NASH-CO Study[J]. Gastroenterology, 2020, 159(2): 791-793. DOI: 10.1053/j.gastro.2020.04.048. [7] Eguchi Y, Hyogo H, Ono M, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study[J]. J Gastroenterol, 2012, 47(5): 586-595. DOI: 10.1007/s00535-012-0533-z. [8] Huang TD, Behary J, Zekry A. Non-alcoholic fatty liver disease: a review of epidemiology, risk factors, diagnosis and management[J]. Intern Med J, 2020, 50(9): 1038-1047. DOI: 10.1111/imj.14709. [9] Chen YL, Li H, Li S, et al. Prevalence of and risk factors for metabolic associated fatty liver disease in an urban population in China: a cross-sectional comparative study[J]. BMC Gastroenterol, 2021, 21(1): 212. DOI: 10.1186/s12876-021-01782-w. [10] Li H, Guo M, An Z, et al. Prevalence and risk factors of metabolic associated fatty liver disease in Xinxiang, China[J]. Int J Environ Res Public Health, 2020, 17(6): 1818. DOI: 10.3390/ijerph17061818. [11] Liu D, Shen Y, Zhang R, et al. Prevalence and risk factors of metabolic associated fatty liver disease among people living with HIV in China[J]. J Gastroenterol Hepatol, 2020, 36(6): 1670-1678. DOI: 10.1111/jgh.15320. [12] Eguchi Y, Hyogo H, Ono M, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study[J]. J Gastroenterol, 2012, 47(5): 586-595. DOI: 10.1007/s00535-012-0533-z. [13] Lai X, Yang L, Legare S, et al. Dose-response relationship between serum uric acid levels and risk of incident coronary heart disease in the Dongfeng-Tongji Cohort[J]. Int J Cardiol, 2016, 224: 299-304. DOI: 10.1016/j.ijcard.2016.09.035. [14] Wong WV, Wong GL, Woo J, et al. Impact of the new definition of metabolic associated fatty liver disease on the epidemiology of the disease[J]. Clin Gastroenterol Hepatol, 2021, 19(10): 2161-2171. DOI: 10.1016/j.cgh.2020.10.046. [15] Zhou YJ, Li YY, Nie YQ, et al. Prevalence of fatty liver disease and its risk factors in the population of South China[J]. World J Gastroenterol, 2007, 13(47): 6419-6424. DOI: 10.3748/wjg.v13.i47.6419. [16] Wong VW, Chu WC, Wong GL, et al. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography[J]. Gut, 2012, 61(3): 409-415. DOI: 10.1136/gutjnl-2011-300342. [17] Park SH, Jeon WK, Kim SH, et al. Prevalence and risk factors of non-alcoholic fatty liver disease among Korean adults[J]. J Gastroenterol Hepatol, 2006, 21(1 Pt 1): 138-143. DOI: 10.1111/j.1440-1746.2005.04086.x. [18] Yoneda M, Thomas E, Sumida Y, et al. The influence of menopause on the development of hepatic fibrosis in nonobese women with nonalcoholic fatty liver disease[J]. Hepatology, 2014, 60(5): 1792. DOI: 10.1002/hep.27097. [19] Yang JD, Abdelmalek MF, Pang H, et al. Gender and menopause impact severity of fibrosis among patients with nonalcoholic steatohepatitis[J]. Hepatology, 2014, 59(4): 1406-1414. DOI: 10.1002/hep.26761. [20] Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases[J]. Hepatology, 2018, 67(1): 328-357. DOI: 10.1002/hep.29367. [21] Dietrich P, Hellerbrand C. Non-alcoholic fatty liver disease, obesity and the metabolic syndrome[J]. Best Pract Res Clin Gastroenterol, 2014, 28(4): 637-653. DOI: 10.1016/j.bpg.2014.07.008. [22] Mantovani A, Byrne CD, Bonora E, et al. Nonalcoholic fatty liver disease and risk of incident type 2 diabetes: a meta-analysis[J]. Diabetes Care, 2018, 41(2): 372-382. DOI: 10.2337/dc17-1902. -





 下载:
下载: