The associations of Non-traditional lipid profiles with stroke: based on Inner Mongolia population
-
摘要:
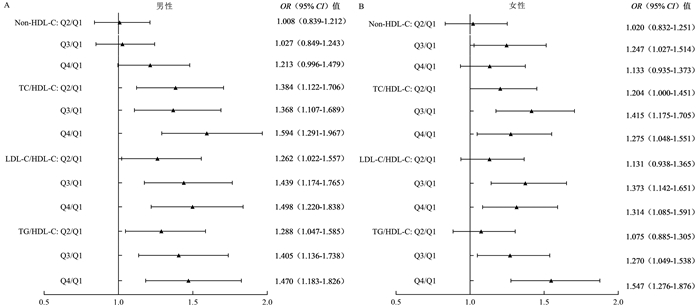
目的 非传统脂质参数已被证实与心血管疾病有关,而内蒙古地区作为脑卒中高发和特定的血脂特征地区,非传统脂质参数与脑卒中风险的关联性研究较少。本研究利用内蒙古地区“心血管病高危人群早期筛查与综合干预项目”探索内蒙古地区非传统脂质参数与脑卒中的关联。 方法 2015―2017年,收集中国北部内蒙古地区35~75岁常住人群的人口学基本信息及各项血脂指标,最终纳入32 518人参与本项研究。将各脂质参数分为四分位,以第1四分位为参照,采用多因素Logistic回归分析模型探索非传统脂质参数与脑卒中的OR值及95% CI值。 结果 本研究含脑卒中患者1 949人,以脑卒中为因变量,调整相关因素后的Logistic回归分析模型结果表明,以各非传统脂质参数第1四分位为参照,第4四分位的TC/HDL-C、LDL-C/HDL-C、TG/HDL-C与脑卒中有关,其对应OR值分别为1.390(95% CI: 1.206~1.601)、1.380(95% CI: 1.201~1.585)及1.473(95% CI: 1.276~1.699);且随着各脂质参数水平的升高,脑卒中风险增加(均有P < 0.001)。在不同性别、年龄中除非高密度脂蛋白胆固醇(Non-high density lipoprotein-cholesterol, Non-HDL-C)外,TC/HDL-C、LDL-C/HDL-C及TG/HDL-C与脑卒中风险相关。 结论 TC/HDL-C、LDL-C/HDL-C及TG/HDL-C为脑卒中的危险因素,相比于传统脂质参数,非传统脂质参数与脑卒中的关联更强,其可作为脑卒中风险分层及一级预防的新指标。 Abstract:Objective Non-traditional lipid profiles are recognized as predictors for cardiovascular disease, but there are few researches on the association between non-traditional lipid profiles and stroke risk in Inner Mongolia. The purpose of this study was to explore the association between non-traditional lipid profiles and stroke in Inner Mongolia through the Program of Screening and Intervention Subjects with High-Risk Cardiovascular Diseases Survey. Methods From 2015 to 2017, demographic basic information and various blood lipid indicators were collected from permanent residents aged 35-75 in Inner Mongolia, North China. A total of 32 518 people was finally included in this study. We categorized plasma lipid measurements into quartile and calculated odds ratios (ORs) and their 95% confidence intervals (CIs) using adjusted Multivariate Logistic regression models. Results The study included 1 949 stroke patients. Comparing with the lowest quarter, the OR of stroke risk in the highest were 1.390 (95% CI: 1.206-1.601) for total cholesterol/ high-density lipoprotein-cholesterol(TC/HDL-C), 1.380 (95% CI: 1.201-1.585) for low-density lipoprotein-cholesterol/ high-density lipoprotein-cholesterol(LDL-C/HDL-C), and 1.473 (95% CI: 1.276-1.699) for triglycerides/ high-density lipoprotein-cholesterol(TG/HDL-C), respectively. Higher lipid profiles related to an increased risk for stroke (all P < 0.001). The TC/HDL-C, LDL-C/HDL-C and TG/HDL-C were still associated with the risk of stroke in different genders and age groups except for Non-high-density lipoprotein cholesterol (Non-HDL-C). Conclusions We found that TC/HDL-C, LDL-C/HDL-C and TG/HDL-C were associated with an increased risk of stroke. Compared with traditional lipid parameters, non-traditional lipids are more strongly associated with stroke, which can be used as a new indicator for risk stratification and primary prevention of stroke. -
Key words:
- Non-traditional lipids /
- Stroke /
- Inner mongolia
-
表 1 调查人群基本特征[n(%)]
Table 1. Baseline characteristics of the population [n(%)]
变量 脑卒中 非脑卒中 合计 χ2/Z值 P值 年龄(岁) 363.562 < 0.001 ac <55 569(29.19) 15 733(51.47) 16 302(50.13) ≥55 1 380(70.81) 14 836(48.53) 16 216(49.87) 性别 27.159 < 0.001 ac 女性 1 017(52.18) 17 789(58.19) 18 806(57.83) 男性 932(47.82) 12 780(41.81) 13 712(42.17) 民族 6.826 0.009 ac 汉族 1 820(93.38) 28 034(91.71) 29 854(91.81) 蒙古族 129(6.62) 2 535(8.29) 2 664(8.19) BMI [M(P25, P75), kg/m2] 25.86(23.63, 28.28) 25.95(23.65, 28.27) 25.94(23.65, 28.27) -0.694 0.488 b 吸烟 479(24.58) 8 159(26.69) 8 638(26.56) 4.196 0.041 ac 饮酒 572(29.35) 9 734(31.84) 10 306(31.69) 5.266 0.022 ac 高血压病史 1 086(55.72) 11 929(39.02) 13 015(40.02) 212.806 < 0.001 ac 糖尿病病史 252(12.93) 2 886(9.44) 3 138(9.65) 25.577 < 0.001 ac 传统脂质参数[M(P25, P75), mmol/L] TC 4.55(3.84, 5.22) 4.53(3.92, 5.23) 4.53(3.91, 5.23) -1.372 0.170 b TG 1.40(1.04, 2.03) 1.37(1.00, 1.94) 1.37(1.00, 1.94) -3.495 < 0.001 bc HDL-C 1.30(1.07, 1.56) 1.36(1.11, 1.65) 1.36(1.11, 1.65) -6.585 < 0.001 bc LDL-C 2.47(1.94, 3.08) 2.43(1.92, 3.02) 2.44(1.92, 3.02) -1.026 0.305 b 血压参数[M(P25, P75), mm Hg] SBP 147.00(132.50, 161.00) 145.00(128.50, 163.50) 145.00(129.00, 163.00) -3.021 0.003 bc DBP 86.50(78.50, 94.25) 86.50(78.50, 96.50) 86.50(78.50, 96.50) -2.191 0.028 bc 非传统脂质参数[M(P25, P75), mmol/L] Non-HDL-C 3.20(2.58, 3.85) 3.14(2.55, 3.80) 3.15(2.55, 3.80) -1.298 0.194 b TC/HDL-C 3.45(2.85, 4.20) 3.35(2.73, 4.12) 3.35(2.74, 4.12) -4.278 < 0.001 bc LDL-C/HDL-C 1.91(1.42, 2.46) 1.81(1.33, 2.40) 1.81(1.34, 2.40) -4.497 < 0.001 bc TG/HDL-C 1.12(0.73, 1.74) 1.01(0.66, 1.61) 1.02(0.66, 1.62) -5.905 < 0.001 bc 注:a表示采用χ2检验进行检验;b表示采用Mann-Whitney U检验;c表示与0.05相比,差异有统计学意义。 表 2 非传统脂质参数与脑卒中的多因素Logistic回归分析模型[OR (95% CI)值]
Table 2. Logistic regression analysis of the non-traditional lipids and stroke [OR (95% CI)值]
脂质参数(mmol/L) 第1四分位组 第2四分位组 第3四分位组 第4四分位组 P趋势值 Non-HDL-C < 2.550 2.550~ < 3.150 3.150~ < 3.800 ≥3.800 模型1 1.000 0.951(0.832~1.087) 1.039(0.912~1.185) 1.024(0.897~1.168) 0.455 模型2 1.000 1.001(0.874~1.147) 1.117(0.977~1.278) 1.127(0.985~1.291) 0.032 TC/HDL-C < 2.736 2.736~ < 3.352 3.352~ < 4.121 ≥4.121 模型1 1.000 1.225(1.069~1.404) a 1.296(1.133~1.482) a 1.272(1.112~1.456) a < 0.001 模型2 1.000 1.271(1.106~1.460) a 1.370(1.192~1.575) a 1.390(1.206~1.601) a < 0.001 LDL-C/HDL-C < 1.339 1.339~ < 1.815 1.815~ < 2.400 ≥2.400 模型1 1.000 1.121(0.977~1.286) 1.277(1.119~1.458) a 1.233(1.079~1.410) a < 0.001 模型2 1.000 1.183(1.029~1.360) a 1.388(1.211~1.590) a 1.380(1.201~1.585) a < 0.001 TG/HDL-C < 0.662 0.662~ < 1.016 1.016~ < 1.622 ≥1.622 模型1 1.000 1.174(1.022~1.349) a 1.323(1.155~1.516) a 1.463(1.279~1.673) a < 0.001 模型2 1.000 1.166(1.012~1.343) a 1.312(1.138~1.511) a 1.473(1.276~1.699) a < 0.001 TC < 3.910 3.910~ < 4.530 4.530~ < 5.230 ≥5.230 模型1 1.000 0.791(0.693~0.903) a 0.908(0.798~1.033) 0.838(0.733~0.957) a 0.063 模型2 1.000 0.848(0.742~0.970) a 0.994(0.871~1.133) 0.926(0.808~1.060) 0.709 TG < 1.000 1.000~ < 1.370 1.370~ < 1.940 ≥1.940 模型1 1.000 1.112(0.973~1.271) 1.100(0.962~1.258) 1.244(1.091~1.420) a 0.002 模型2 1.000 1.113(0.971~1.274) 1.077(0.937~1.237) 1.218(1.061~1.399) a 0.012 HDL-C < 1.110 1.110~ < 1.360 1.360~ < 1.650 ≥1.650 模型1 1.000 0.815(0.719~0.924) a 0.772(0.679~0.878) a 0.622(0.542~0.713) a < 0.001 模型2 1.000 0.796(0.701~0.904) a 0.749(0.656~0.855) a 0.604(0.523~0.698) a < 0.001 LDL-C < 1.920 1.920~ < 2.440 2.440~ < 3.020 ≥3.020 模型1 1.000 0.964(0.844~1.101) 1.002(0.878~1.143) 1.019(0.893~1.161) 0.652 模型2 1.000 1.040(0.909~1.190) 1.107(0.968~1.266) 1.146(1.002~1.310) a 0.030 注:模型1:调整因素含性别、年龄;模型2:调整因素含性别、年龄、民族、BMI、是否吸烟、是否饮酒、目前是否患有高血压、目前是否患有糖尿病、是否服用调脂药物及脑卒中家族史情况;以各非传统脂质参数第1四分位为参照,a表示以第1四分位为参照,P < 0.05。 -
[1] Avan A, Digaleh H, Di Napoli M, et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017[J]. BMC Med, 2019, 17(1): 191. DOI: 10.1186/s12916-019-1397-3. [2] Liu L, Wang D, Wong KS, et al. Stroke and stroke care in China: huge burden, significant workload, and a national priority[J]. Stroke, 2011, 42(12): 3651-3654. DOI: 10.1161/strokeaha.111.635755. [3] GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2018, 392(10159): 1789-1858. DOI: 10.1016/s0140-6736(18)32279-7. [4] Wang WZ, Jiang B, Sun HX, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults[J]. Circulation, 2017, 135(8): 759-771. DOI: 10.1161/CIRCULATIONAHA.116.025250. [5] Xu GL, Ma MM, Liu XF, et al. Is there a stroke belt in China and why?[J]. Stroke, 2013, 44(7): 1775-1783. DOI: 10.1161/strokeaha.113.001238. [6] Pisciotta L, Bertolini S, Pende A. Lipoproteins, stroke and statins[J]. Curr Vasc Pharmacol, 2015, 13(2): 202-208. DOI: 10.2174/15701611113116660166. [7] Shahar E, Chambless LE, Rosamond WD, et al. Plasma lipid profile and incident ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) study[J]. Stroke, 2003, 34(3): 623-631. DOI: 10.1161/01.STR.0000057812.51734.FF. [8] Gorelick PB, Mazzone T. Plasma lipids and stroke[J]. J Cardiovasc Risk, 1999, 6(4): 217-221. DOI: 10.1177/204748739900600405. [9] Tirschwell DL, Smith NL, Heckbert SR, et al. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups[J]. Neurology, 2004, 63(10): 1868-1875. DOI: 10.1212/01.wnl.0000144282.42222.da. [10] Rist PM, Buring JE, Ridker PM, et al. Lipid levels and the risk of hemorrhagic stroke among women[J]. Neurology, 2019, 92(19): e2286-e2294. DOI: 10.1212/WNL.0000000000007454. [11] Glasser SP, Mosher A, Howard G, et al. What is the association of lipid levels and incident stroke?[J]. Int J Cardiol, 2016, 220: 890-894. DOI: 10.1016/j.ijcard.2016.06.091. [12] Gu XY, Yang XL, Li Y, et al. Usefulness of low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol as predictors of cardiovascular disease in Chinese[J]. Am J Cardiol, 2015, 116(7): 1063-1070. DOI: 10.1016/j.amjcard.2015.06.040. [13] Kurth T, Everett BM, Buring JE, et al. Lipid levels and the risk of ischemic stroke in women[J]. Neurology, 2007, 68(8): 556-562. DOI: 10.1212/01.wnl.0000254472.41810.0d. [14] Rodgers A, Macmahon S, Yee T, et al. Blood pressure, cholesterol, and stroke in eastern Asia. Eastern Stroke and Coronary Heart Disease Collaborative Research Group[J]. Lancet, 1998, 352(9143): 1801-1807. DOI: 10.1016/s0140-6736(98)03454-0. [15] Zhang Y, Tuomilehto J, Jousilahti P, et al. Total and high-density lipoprotein cholesterol and stroke risk[J]. Stroke, 2012, 43(7): 1768-1774. DOI: 10.1161/strokeaha.111.646778. [16] Jain M, Jain A, Yerragondu N, et al. The triglyceride paradox in stroke survivors: a prospective study[J]. Neurosci J, 2013, 2013: 870608. DOI: 10.1155/2013/870608. [17] Park JH, Lee J, Ovbiagele B. Nontraditional serum lipid variables and recurrent stroke risk[J]. Stroke, 2014, 45(11): 3269-3274. DOI: 10.1161/strokeaha.114.006827. [18] Bittner V, Hardison R, Kelsey SF, et al. Non-high-density lipoprotein cholesterol levels predict five-year outcome in the Bypass Angioplasty Revascularization Investigation (BARI)[J]. Circulation, 2002, 106(20): 2537-2542. DOI: 10.1161/01.cir.0000038496.57570.06. [19] Arsenault BJ, Rana JS, Stroes ES, et al. Beyond low-density lipoprotein cholesterol: respective contributions of non-high-density lipoprotein cholesterol levels, triglycerides, and the total cholesterol/high-density lipoprotein cholesterol ratio to coronary heart disease risk in apparently healthy men and women[J]. J Am Coll Cardiol, 2009, 55(1): 35-41. DOI: 10.1016/j.jacc.2009.07.057. [20] McLaughlin T, Reaven G, Abbasi F, et al. Is there a simple way to identify insulin-resistant individuals at increased risk of cardiovascular disease?[J]. Am J Cardiol, 2005, 96(3): 399-404. DOI: 10.1016/j.amjcard.2005.03.085. [21] Barzi F, Patel A, Woodward M, et al. A comparison of lipid variables as predictors of cardiovascular disease in the Asia Pacific region[J]. Ann Epidemiol, 2005, 15(5): 405-413. DOI: 10.1016/j.annepidem.2005.01.005. [22] Millán J, Pintó X, Muñoz A, et al. Lipoprotein ratios: Physiological significance and clinical usefulness in cardiovascular prevention[J]. Vasc Health Risk Manag, 2009, 5: 757-765. http://pdfs.semanticscholar.org/6da1/908ed1d9ceb030bd6a775920911d9e046e9f.pdf [23] Castelli WP, Anderson K, Wilson PW, et al. Lipids and risk of coronary heart disease. The Framingham Study[J]. Ann Epidemiol, 1992, 2(1-2): 23-28. DOI: 10.1016/1047-2797(92)90033-m. [24] da Luz PL, Cesena FH, Favarato D, et al. Comparison of serum lipid values in patients with coronary artery disease at <50, 50 to 59, 60 to 69, and > 70 years of age[J]. Am J Cardiol, 2005, 96(12): 1640-1643. DOI: 10.1016/j.amjcard.2005.07.080. [25] da Luz PL, Favarato D, Faria-Neto JR, et al. High ratio of triglycerides to HDL-Cholesterol predicts extensive coronary disease[J]. Clinics (Sao Paulo), 2008, 63(4): 427-432. DOI: 10.1590/s1807-59322008000400003. [26] Bittner V, Johnson BD, Zineh I, et al. The triglyceride/high-density lipoprotein cholesterol ratio predicts all-cause mortality in women with suspected myocardial ischemia: a report from the Women's Ischemia Syndrome Evaluation (WISE)[J]. Am Heart J, 2009, 157(3): 548-555. DOI: 10.1016/j.ahj.2008.11.014. [27] Fujihara K, Suzuki H, Sato A, et al. Carotid artery plaque and LDL-to-HDL cholesterol ratio predict atherosclerotic status in coronary arteries in asymptomatic patients with type 2 diabetes mellitus[J]. J Atheroscler Thromb, 2013, 20(5): 452-464. DOI: 10.5551/jat.14977. [28] Turak O, Afşar B, Ozcan F, et al. The role of plasma triglyceride/high-density lipoprotein cholesterol ratio to predict new cardiovascular events in essential hypertensive patients[J]. J Clin Hypertens (Greenwich), 2016, 18(8): 772-777. DOI: 10.1111/jch.12758. [29] Pikula A, Beiser AS, Wang J, et al. Lipid and lipoprotein measurements and the risk of ischemic vascular events: Framingham Study[J]. Neurology, 2015, 84(5): 472-479. DOI: 10.1212/wnl.0000000000001202. [30] Willey JZ, Xu Q, Boden-Albala B, et al. Lipid profile components and risk of ischemic stroke: the Northern Manhattan Study (NOMAS)[J]. Arch Neurol, 2009, 66(11): 1400-1406. DOI: 10.1001/archneurol.2009.210. [31] Yokokawa H, Yasumura S, Tanno K, et al. Serum low-density lipoprotein to high-density lipoprotein ratio as a predictor of future acute myocardial infarction among men in a 2.7-year cohort study of a Japanese northern rural population[J]. J Atheroscler Thromb, 2011, 18(2): 89-98. DOI: 10.5551/jat.5215. [32] Lu JP, Xuan S, Downing NS, et al. Protocol for the China PEACE (patient-centered evaluative assessment of cardiac events) million persons project pilot[J]. BMJ Open, 2016, 6(1): e010200. DOI: 10.1136/bmjopen-2015-010200. [33] Watanabe J, Kakehi E, Kotani K, et al. High-density lipoprotein cholesterol and risk of stroke subtypes: jichi medical school cohort study[J]. Asia Pac J Public Heal, 2020, 32(1): 27-34. DOI: 10.1177/1010539519900685. [34] Shen Y, Shi LZ, Nauman E, et al. Inverse association between HDL (high-density lipoprotein) cholesterol and stroke risk among patients with type 2 diabetes mellitus[J]. Stroke, 2019, 50(2): 291-297. DOI: 10.1161/strokeaha.118.023682. [35] Knopp RH, Paramsothy P, Retzlaff BM, et al. Sex differences in lipoprotein metabolism and dietary response: basis in hormonal differences and implications for cardiovascular disease[J]. Curr Cardiol Rep, 2006, 8(6): 452-459. DOI: 10.1007/s11886-006-0104-0. [36] Mittendorfer B, Patterson BW, Klein S. Effect of sex and obesity on basal VLDL-triacylglycerol kinetics[J]. Am J Clin Nutr, 2003, 77(3): 573-579. DOI: 10.1093/ajcn/77.3.573. [37] Burke AP, Farb A, Malcom G, et al. Effect of menopause on plaque morphologic characteristics in coronary atherosclerosis[J]. Am Heart J, 2001, 141(2 suppl): S58-S62. DOI: 10.1067/mhj.2001.109946. [38] Shin J, Chung JW, Jang HS, et al. Achieved low-density lipoprotein cholesterol level and stroke risk: a meta-analysis of 23 randomised trials[J]. Eur J Prev Cardiol, 2019: 2047487319830503. DOI: 10.1177/2047487319830503. [39] Liu X, Yan L, Xue F. The associations of lipids and lipid ratios with stroke: a prospective cohort study[J]. J Clin Hypertens (Greenwich), 2019, 21(1): 127-135. DOI: 10.1111/jch.13441. [40] Zheng J, Sun Z, Zhang X, et al. Non-traditional lipid profiles associated with ischemic stroke not hemorrhagic stroke in hypertensive patients: results from an 8.4 years follow-up study[J]. Lipids Health Dis, 2019, 18(1): 9. DOI: 10.1186/s12944-019-0958-y. [41] de la Riva P, Zubikarai M, Sarasqueta C, et al. Nontraditional lipid variables predict recurrent brain ischemia in embolic stroke of undetermined source[J]. J Stroke Cerebrovasc Dis, 2017, 26(8): 1670-1677. DOI: 10.1016/j.jstrokecerebrovasdis.2017.03.024. [42] Criqui MH, Golomb BA. Epidemiologic aspects of lipid abnormalities[J]. Am J Med, 1998, 105(1a): 48S-57S. DOI: 10.1016/s0002-9343(98)00212-5. [43] Wu J, Chen S, Zhou Y, et al. Non-high-density lipoprotein cholesterol on the risks of stroke: a result from the Kailuan study[J]. PLoS One, 2013, 8(9): e74634. DOI: 10.1371/journal.pone.0074634. [44] Imamura T, DoiY, Ninomiya T, et al. Non-high-density lipoprotein cholesterol and the development of coronary heart disease and stroke subtypes in a general Japanese population: The Hisayama Study[J]. Atherosclerosis, 2014, 233(2): 343-348. DOI: 10.1016/j.atherosclerosis.2014.01.005. [45] Okamura T, Kokubo Y, Watanabe M, et al. Low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol and the incidence of cardiovascular disease in an urban Japanese cohort study: The Suita study[J]. Atherosclerosis, 2009, 203(2): 587-592. DOI: 10.1016/j.atherosclerosis.2008.07.020. [46] Tanabe N, Iso H, Okada K, et al. Serum total and non-high-density lipoprotein cholesterol and the risk prediction of cardiovascular events-the JALS-ECC[J]. Circ J, 2010, 74(7): 1346-1356. DOI: 10.1253/circj.cj-09-0861. [47] Okamura T, Kokubo Y, Watanabe M, et al. Low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol and the incidence of cardiovascular disease in an urban Japanese cohort study: The Suita study[J]. Atherosclerosis, 2009, 203(2): 587-592. DOI: 10.1016/j.atherosclerosis.2008.07.020. [48] Kakehi E, Kotani K, Ishikawa S, et al. Serum non-high-density lipoprotein cholesterol levels and the incidence of ischemic stroke in a Japanese population: the Jichi Medical School cohort study[J]. Asia-Pac J Public Heal, 2015, 27(2): NP535-NP543. DOI: 10.1177/1010539513475649. [49] Yatsuya H, Iso H, Li Y, et al. Development of a risk equation for the incidence of coronary artery disease and ischemic stroke for middle-aged Japanese-Japan public health center-based prospective study[J]. Circ J, 2016, 80(6): 1386-1395. DOI: 10.1253/circj.cj-16-0081. [50] Saito I, Yamagishi K, Kokubo Y, et al. Non-high-density lipoprotein cholesterol and risk of stroke subtypes and coronary heart disease: the Japan public health center-based prospective (JPHC) study[J]. J Atheroscler Thromb, 2020, 27(4): 363-374. DOI: 10.5551/jat.50385. -





 下载:
下载: