-
摘要:
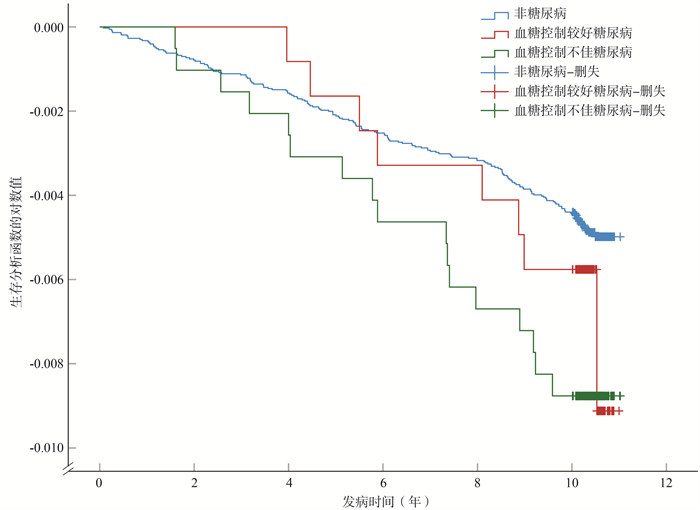
目的 探讨血糖控制与结核病发病风险之间的关系。 方法 在中国东部地区对40 311名研究对象开展队列研究,通过10年的随访,探讨结核病发病的危险因素。排除了基线调查时发现的结核病患者,通过与南京市结核病管理信息系统进行匹配发现结核病患者。主要通过匹配身份证号码、姓名、年龄、出生日期和地址。并建立了Cox比例风险模型,调整了年龄、性别、吸烟状况等因素。 结果 经过10年(中位随访时间为8.4年)的随访,共发现204名活动性结核病患者,发病密度为59.0/10万人年(95% CI:51.3~67.5)。其中,糖尿病患者有25人,占12.3%,发病密度为71.3/10万人年(95% CI:47.2~103.8)。共发现7名血糖控制不佳糖尿病患者发病,发病密度为84.4/10万人年(95% CI:50.8~132.4)。当把人群按照FPG是否≥7.0 mmol/L分组时,研究发现,与FPG < 7.0 mmol/L相比,FPG≥7.0 mmol/L人群发生结核病的风险提高0.89倍[风险比(hazard ratio, HR)=1.89,95% CI: 1.13~3.13,P=0.014]。 结论 此次大规模的人群队列研究发现,糖尿病患者血糖控制不佳增加了其发生结核病的风险。因此,加强对血糖控制不佳糖尿病患者的筛查可以及早发现结核病,有利于降低中国结核病的发生与流行。 Abstract:Objective To evaluate the association between glycemic control among diabetes and active tuberculosis. Methods We conducted a population-based census in eastern China including 40 311 individuals. We investigated risk factors for active tuberculosis by excluding tuberculosis at baseline and linked all participants to the Infectious Disease Reporting Management System and tuberculosis Management Information System of Nanjing City. We followed participants for ten years. We matched participants using unique health identity card numbers, name, age, birthdate, and address. We constructed Cox Proportional hazard models adjusting for age, sex, smoking. Results After 10 years follow-up, 204 individuals progressed to tuberculosis (incidence rate, 71.3 per 100 000 person-years, 95% CI: 51.3-67.5), of whom 25 were diabetes, accounting for 12.3% (incidence rate, 59.0 per 100 000 person-years, 95% CI: 47.2-103.8) and 7 diabetes were with poor glycemic control (incidence rate, 84.4 per 100 000 person-years, 95% CI: 50.8-132.4). Diabetic patients had a significantly higher hazard of tuberculosis [hazard ratio (HR)=1.56, 95% CI: 1.01-2.39, P=0.044]. Diabetics with FPG≥7.0 mmol/L showed nearly one-fold increased risk of active tuberculosis (HR=1.89, 95% CI: 1.13-3.13, P=0.014). Conclusions In this large population-based cohort study in a medium tuberculosis burden region, we found that diabetes increased the hazard of tuberculosis disease and diabetics with poor glycemic control control aggravated this relationship. Strengthening the screening of diabetes patients with poor glycemic control control can improve the efficiency of tuberculosis detection in diabetes patients and help reduce the prevalence of tuberculosis in China. -
Key words:
- Mycobacterium tuberculosis /
- Diabetes /
- Glycemic control /
- Tuberculosis
-
表 1 40 311受试者按照糖尿病分组的人口学特征[n(%)]
Table 1. Demographic characteristics of 40 311 participants stratified by diabetes status [n(%)]
组别 合计 非糖尿病 糖尿病 χ2值 P值 性别 2.34 0.126 女 22 067(54.7) 20 258(54.9) 1 809(53.5) 男 18 244(45.3) 16 671(45.1) 1 573(46.5) 年龄[M(P25, P75), 岁] 50(37,61) 49(35,60) 59(50,67) BMI(kg/m2) 36.77 < 0.001 < 18.5 1 880(4.7) 1 738(4.7) 142(4.2) 18.5~ < 24.0 22 566(56.3) 20 818(56.7) 1 748(52.1) 24.0~ < 28.0 12 449(31.0) 11 312(30.8) 1 137(33.9) ≥28.0 3 212(8.0) 2 884(7.8) 328(9.8) 吸烟史 4.36 0.035 否 31 566(78.3) 28 966(78.4) 2 600(76.9) 是 8 745(21.7) 7 963(21.6) 782(23.1) 饮酒史 1.02 0.312 否 33 917(84.1) 31 092(84.2) 2 825(83.5) 是 6 394(15.9) 5 837(15.8) 557(16.5) FPG[M(P25, P75), mmol/L] 5.1(4.6, 5.6) 5.0(4.6, 5.4) 7.2(6.1, 8.5) 表 2 根据基线糖尿病水平分组的结核病发病密度
Table 2. Tuberculosis incidence rate stratified by diabetes status
分组 发病数(n) 观察人年数(人年) 发病密度(万人年) 发病密度95% CI(万人年) 所有受试者 204 345 793 59.0 51.3~67.5 糖尿病 否 179 383 046 48.6 40.3~54.0 是 25 35 043 71.3 47.2~103.8 血糖控制较好 8 12 677 63.1 29.3~119.8 血糖控制不佳 17 20 134 84.4 50.8~132.4 FPG(mmol/L) < 7.0 150 326 447 46.0 39.0~53.8 ≥7.0 17 20 134 84.4 50.8~132.4 表 3 结核病发病风险的单因素Cox比例风险模型
Table 3. A univariate Cox proportional risk model for the risk of developing tuberculosis
组别 活动性结核病 发病例数/总人数(% a) HR(95% CI)值 P值 性别 女 82/22 067(0.4) 1.00 男 122/18 244(0.7) 1.80(1.36~2.39) < 0.001 年龄(岁) 1.00(0.99~1.01) 0.897 BMI(kg/m2) < 18.5 11/1 880(0.6) 1.00 18.5~ < 24.0 135/22 566(0.6) 1.02(0.55~1.89) 0.943 24.0~ < 28.0 46/12 449(0.4) 0.63(0.33~1.22) 0.170 ≥28.0 12/3 212(0.4) 0.64(0.28~1.45) 0.282 吸烟史 否 150/31 566(0.5) 1.00 是 54/8 745(0.6) 1.30(0.95~1.78) 0.096 饮酒史 否 169/33 917(0.5) 1.00 是 35/6 394(0.5) 1.12(0.78~1.61) 0.554 糖尿病 否 179/36 929(0.5) 1.00 是 25/3 382(0.7) 1.53(1.01~2.32) 0.047 血糖控制较好 8/1 219(0.7) 1.35(0.66~2.74) 0.409 血糖控制不佳 17/1 948(0.9) 1.81(1.10~2.98) 0.019 FPG(mmol/L) < 7.0 150/31 436(0.5) 1.00 ≥7.0 17/1 948(0.9) 1.85(1.12~3.05) 0.017 连续性变量 1.08(1.00~1.16) 0.077 注:a为发病率。 表 4 结核病发病风险的多因素Cox比例风险模型
Table 4. A multifactorial Cox proportional risk model for the risk of developing tuberculosis
组别 模型Ⅰ 模型Ⅱ 模型Ⅲ 模型Ⅳ HR(95% CI)值 P值 HR(95% CI)值 P值 HR(95% CI)值 P值 HR(95% CI)值 P值 性别 女 1.00 1.00 1.00 1.00 男 1.89(1.38~2.59) < 0.001 1.90(1.38~2.60) < 0.001 1.82(1.27~2.60) 0.001 1.82(1.27~2.60) 0.001 年龄(岁) 1.00(0.99~1.01) 0.609 1.00(0.99~1.01) 0.623 1.00(0.99~1.01) 0.518 1.00(0.99~1.01) 0.592 吸烟史 否 1.00 1.00 1.00 1.00 是 0.90(0.63~1.27) 0.541 0.89(0.63~1.27) 0.524 1.03(0.70~1.51) 0.896 1.03(0.70~1.51) 0.896 糖尿病 否 1.00 1.00 是 1.56(1.01~2.39) 0.044 血糖控制较好 1.37(0.67~2.79) 0.395 血糖控制不佳 1.85(1.12~3.07) 0.017 FPG(mmol/L) < 7.0 1.00 ≥7.0 1.89(1.13~3.13) 0.014 连续性变量 1.07(0.99~1.16) 0.070 注:模型Ⅰ:糖尿病以二分类变量(是、否)纳入模型;模型Ⅱ:糖尿病以三分类变量(否、血糖控制较好、血糖控制不佳)纳入模型;模型Ⅲ:FPG以二分类变量(FPG<7.0 mmol/L、FPG≥7.0 mmol/L)纳入模型;模型Ⅳ:FPG以连续性变量纳入模型。 -
[1] WHO. Global strategy and targets for tuberculosis prevention, care and control after 2015[R]. Geneva: WHO, 2014. [2] Raviglione M, Marais B, Floyd K, et al. Scaling up interventions to achieve global tuberculosis control: progress and new developments[J]. Lancet, 2012, 379(9829): 1902-1913. DOI: 10.1016/S0140-6736(12)60727-2. [3] Lönnroth K, Roglic G, Harries AD. Improving tuberculosis prevention and care through addressing the global diabetes epidemic: from evidence to policy and practice[J]. Lancet Diabetes Endo, 2014, 2(9): 730-739. DOI: 10.1016/S2213-8587(14)70109-3. [4] McMurry HS, Mendenhall E, Rajendrakumar A, et al. Coprevalence of type 2 diabetes mellitus and tuberculosis in low-income and middle-income countries: a systematic review[J]. Diabetes Metab Res Rev, 2019, 35(1): e3066. DOI: 10.1002/dmrr.3066. [5] Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies[J]. PLoS Med, 2008, 5(7): e152. DOI: 10.1371/journal.pmed.0050152. [6] Stevenson CR, Critchley JA, Forouhi NG, et al. Diabetes and the risk of tuberculosis: a neglected threat to public health?[J]. Chronic Illn, 2007, 3(3): 228-245. DOI: 10.1177/1742395307081502. [7] Leegaard A, Riis A, Kornum JB, et al. Diabetes, glycemic control, and risk of tuberculosis: a population-based case-control study[J]. Diabetes Care, 2011, 34(12): 2530-2535. DOI: 10.2337/dc11-0902. [8] Lin CH, Kuo SC, Hsieh MC, et al. Effect of diabetes mellitus on risk of latent TB infection in a high TB incidence area: a community-based study in Taiwan[J]. BMJ Open, 2019, 9(10): e029948. DOI: 10.1136/bmjopen-2019-029948. [9] Pealing L, Wing K, Mathur R, et al. Risk of tuberculosis in patients with diabetes: population based cohort study using the UK Clinical Practice Research Datalink[J]. BMC Med, 2015, 13: 135. DOI: 10.1186/s12916-015-0381-9. [10] Kumpatla S, Sekar A, Achanta S, et al. Characteristics of patients with diabetes screened for tuberculosis in a tertiary care hospital in South India[J]. Public Health Action, 2013, 3(Suppl 1): S23-S28. DOI: 10.5588/pha.13.0035. [11] Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies[J]. PLoS Med, 2008, 5(7): e152. DOI: 10.1371/journal.pmed.0050152. [12] Dooley KE, Chaisson RE. Tuberculosis and diabetes mellitus: convergence of two epidemics[J]. Lancet Infect Dis, 2009, 9(12): 737-746. DOI: 10.1016/S1473-3099(09)70282-8. [13] Lu P, Zhang Y, Liu Q, et al. Association of BMI, diabetes, and risk of tuberculosis: a population-based prospective cohort[J]. Int J Infect Dis, 2021, 109: 168-173. DOI: 10.1016/j.ijid.2021.06.053. [14] Lu P, Liu Q, Zhou Y, et al. Predictors of discordant tuberculin skin test and QuantiFERON-TB Gold In-tube results in Eastern China: a population-based, cohort study[J]. Clin Infect Dis, 2021, 72(11): 2006-2015. DOI: 10.1093/cid/ciaa519. [15] Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation[J]. Diabet Med, 1998, 15(7): 539-553. DOI: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [16] Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults[J]. JAMA, 2013, 310(9): 948-959. DOI: 10.1001/jama.2013.168118. [17] 诸骏仁, 高润霖, 赵水平, 等. 中国成人血脂异常防治指南(2016年修订版)[J]. 中国循环杂志, 2016, 31(10): 937-950. Zhu JR, Gao RL, Zhao SP, et al. Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (revised in 2016)[J]. Chin Cir J, 2016, 31(10): 937-950. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH201610002.htm [18] Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China[J]. N Engl J Med, 2010, 362(12): 1090-1101. DOI: 10.1056/NEJMoa0908292. [19] Bragg F, Holmes MV, Iona A, et al. Association between diabetes and cause-specific mortality in rural and urban areas of China[J]. JAMA, 2017, 317(3): 280-289. DOI: 10.1001/jama.2016.19720. [20] Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies[J]. PLoS Med, 2008, 5(7): e152. DOI: 10.1371/journal.pmed.0050152. [21] Leung CC, Lam TH, Chan WM, et al. Diabetic control and risk of tuberculosis: a cohort study[J]. Am J Epidemiol, 2008, 167(12): 1486-1494. DOI: 10.1093/aje/kwn075. [22] Lee PH, Fu H, Lai TC, et al. Glycemic control and the risk of tuberculosis: a cohort study[J]. PLoS Med, 2016, 13(8): e1002072. DOI: 10.1371/journal.pmed.1002072. [23] Baker MA, Lin HH, Chang HY, et al. The risk of tuberculosis disease among persons with diabetes mellitus: a prospective cohort study[J]. Clin Infect Dis, 2012, 54(6): 818-825. DOI: 10.1093/cid/cir939. [24] MacRury SM, Gemmell CG, Paterson KR, et al. Changes in phagocytic function with glycaemic control in diabetic patients[J]. J Clin Pathol, 1989, 42(11): 1143-1147. DOI: 10.1136/jcp.42.11.1143. [25] Bagdade J, Stewart M, Walters E. Impaired granulocyte adherence: a reversible defect in host defense in patients with poorly controlled diabetes[J]. Diabetes, 1978, 27(6): 677-681. DOI: 10.2337/diab.27.6.677. [26] Singhal A, Jie L, Kumar P, et al. Metformin as adjunct antituberculosis therapy[J]. Sci Transl Med, 2014, 6(263): 263ra159. DOI: 10.1126/scitranslmed.3009885. [27] Yamashiro S, Kawakami K, Uezu K, et al. Lower expression of Th1-related cytokines and inducible nitric oxide synthase in mice with streptozotocin-induced diabetes mellitus infected with Mycobacterium tuberculosis[J]. Clin Exp Immunol, 2005, 139(1): 57-64. DOI: 10.1111/j.1365-2249.2005.02677.x. -





 下载:
下载: