Correlation between circadian disruption and depressive symptom in male undergraduates in Chongqing
-
摘要:
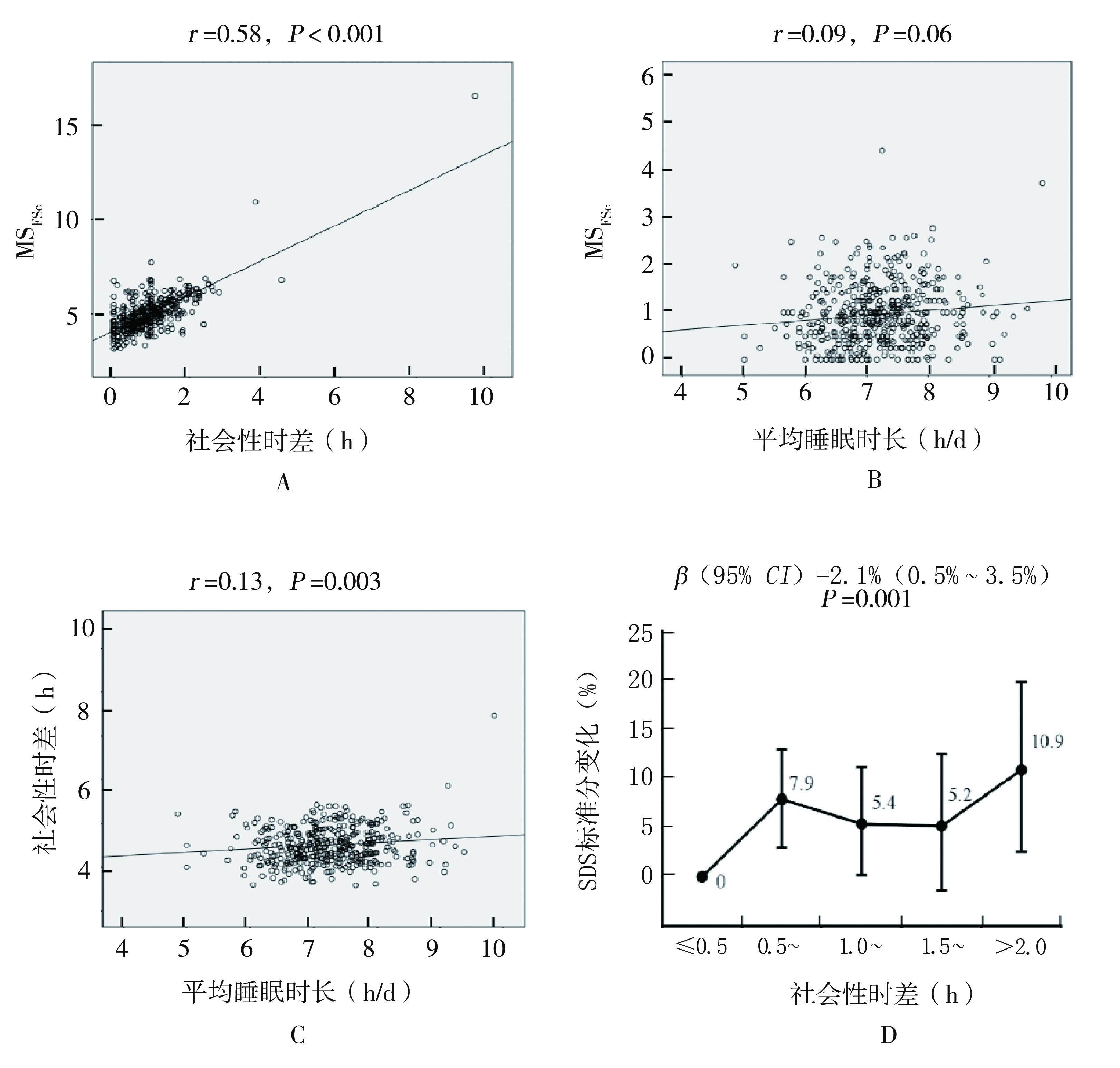
目的 分析重庆市青年男性人群中昼夜节律紊乱是否与抑郁症状存在关联。 方法 采用中文版慕尼黑睡眠时型问卷(Munich chronotype questionnaire, MCTQ)测量社会性时差(用来反映昼夜节律紊乱的指标), 同时测量了平均睡眠时长和反映生物钟特性的睡眠时型指标。采用抑郁自评量表(self-rating depression scale, SDS)的标准分测量抑郁症状。 结果 研究对象的社会性时差为0.9(0.5, 1.3)h, 其与睡眠时型指标之间呈现较强的相关性(r=0.73, P < 0.001)。社会性时差与SDS标准分呈正相关, 校正睡眠时型、睡眠时长、年龄、体重指数、体育运动、吸烟、饮酒、饮茶等因素后, 社会性时差每增加0.5h, SDS标准分相应增加2.1%(95% CI:0.5%~3.5%, P=0.011)。 结论 社会性时差与SDS标准分呈正相关, 提示昼夜节律紊乱可能与抑郁症状有关。 Abstract:Objective To analyze the association between circadian disruption and depressive symptoms in Chongqing young males. Methods Among 587 male college students in Chongqing, the Chinese version of the Munich chronotype questionnaire(MCTQ) was used to measure social jetlag(an indicator of circadian disruption), mean sleep duration and chronotype, which reflected individual biological clock. Depression symptom was measured using standard score of the Self-rating Depression Scale(SDS). Results The subjects' social jetlag was 0.9(0.5 to 1.3) h. There was a strong correlation between social jetlag and chronotype indicator(correlation coefficient = 0.58, P < 0.001).The social jetlag was positively correlated with the SDS standard score. For every 0.5 hour increase in the social jetlag, the SDS standard score increased by 2.1%(95%CI: 0.5%-3.5%, P= 0.011). Conclusion There is a correlation between social jetlag and SDS standard score, suggesting that circadian disruption may be related to depressive symptom. -
Key words:
- Circadian clock /
- Sleep /
- Munich chronotype questionnaire /
- Depression
-
表 1 研究对象的特征分布
Table 1. Characteristic distribution of the study subjects
变量 频数 数据分布(%) 年龄(岁) 587 20.0(20.0, 21.0)a 体重指数(kg/m2) 587 21.0(19.6, 22.9)a < 18.5 62 10.6 18.5~ 437 74.4 24.0~ 71 12.1 ≥28.0 17 2.9 吸烟行为 从不吸烟 460 78.4 曾经吸烟, 现已戒烟 19 3.3 吸烟 107 18.3 饮酒行为 从不饮酒 294 50.5 曾经饮酒, 现已戒酒 7 1.2 饮酒 284 48.3 饮茶行为 从不饮茶 364 62.0 曾经饮茶 102 17.5 饮茶 120 20.5 体育运动 不参加 99 16.9 参加 488 83.1 平均睡眠时长(h/d) 535 7.1(6.7, 7.6)a ≤6.5 93 6.2(6.0, 6.3)a 6.5~ 128 6.8(6.7, 6.9)a 7.0~ 145 7.3(7.1, 7.4)a 7.5~ 115 7.8(7.6, 7.9)a 8.0~ 30 8.2(8.1, 8.3)a 8.5~ 15 8.6(8.6, 8.6)a > 9.0 9 9.2(9.1, 9.4)a MSFSc分类(睡眠时型) 414 4.9(4.4, 5.5)a 早起型(上1/3) 136 4.2(4.0, 4.4)a 中间型(中1/3) 146 4.9(4.7, 5.1)a 晚起型(下1/3) 132 5.8(5.6, 6.2)a 社会性时差(h) 556 0.9(0.5, 1.3)a ≤0.5 200 0.3(0.0, 0.4)a 0.5~ 177 0.8(0.7, 1.0)a 1.0~ 112 1.3(1.2, 1.4)a 1.5~ 58 1.8(1.7, 1.9)a > 2.0 39 2.3(2.2, 2.6)a SDS标准分 587 38(32, 45)a 注:aM(P25, P75)。 表 2 MCTQ各指标与SDS标准分的关联分析(单因素)
Table 2. Association of MCTQ indicators and SDS standard score (univariate analysis)
睡眠指标 样本量 SDS标准分a P值 Kruskal-Wallis法 Jonckheere-Terpstra法 社会性时差分类(h) 0.002 0.02 ≤0.5 200 35(31, 42) 0.5~ 177 40(33, 46) 1.0~ 112 38(32, 45) 1.5~ 58 38(32, 46) > 2.0 39 41(35, 46) 平均睡眠时长分类(h/d) 0.262 0.600 ≤6.5 93 38(33, 47) 6.5~ 128 37(32, 43) 7.0~ 145 38(32, 43) 7.5~ 115 36(31, 42) 8.0~ 30 39(32, 50) 8.5~ 15 37(32, 52) > 9.0 9 42(32, 52) MSFSc分类(睡眠时型) 0.142 0.126 早起型 136 36(32, 43) 中间型 146 37(32, 43) 晚起型 132 39(32, 46) 注:aM(P25, P75)。 -
[1] Wang R, Liu Y, Xue D, et al. Depressive symptoms among Chinese residents: how are the natural, built, and social environments correlated?[J]. BMC public health, 2019, 19(1): 887. DOI: 10.1186/s12889-019-7171-9. [2] Qin X, Wang S, Hsieh CR. The prevalence of depression and depressive symptoms among adults in China: estimation based on a national household survey[J]. China Economic Review, 2018, (51): 271-282. DOI: 10.1016/j.chieco.2016.04.001. [3] 王婷, 周艳辉, 罗阳.湖南省青春期女性焦虑、抑郁现状调查及其影响因子的预测[J].中华疾病控制杂志, 2019, 23(8): 971-976. DOI: 10.3760/cma.j.issn.1674-6554.2000.03.016.Wang T, Zhou YH, Luo Y. Anxiety, depression status of adolescent females and prediction of related influencing factors in Hunan Province[J]. Chin J Dis Prev, 2019, 23(8): 971-976. DOI: 10.3760/cma.j.issn.1674-6554.2000.03.016. [4] Takahashi JS, Hong HK, Ko CH, et al. The genetics of mammalian circadian order and disorder: implications for physiology and disease[J]. Nat Rev Genet, 2008, 9(10): 764-775. DOI: 10.1038/nrg2430. [5] Bunney WE, Bunney BG. Molecular clock genes in man and lower animals: possible implications for circadian abnormalities in depression[J]. Neuropsychopharmacology, 2000, 22(4): 335-345. DOI: 10.1016/S0893-133X(99)00145-1. [6] Landgraf D, Long JE, Welsh DK. Depression-like behaviour in mice is associated with disrupted circadian rhythms in nucleus accumbens and periaqueductal grey[J]. Eur J neurosci, 2016, 43(10): 309-320. DOI: 10.1111/ejn.13085. [7] Griesauer I, Diao W, Ronovsky M, et al. Circadian abnormalities in a mouse model of high trait anxiety and depression[J]. Ann Med, 2014, 46(3): 148-154. DOI: 10.3109/07853890.2013.866440. [8] Levandovski R, Dantas G, Fernandes LC, et al. Depression scores associate with chronotype and social jetlag in a rural population[J]. Chronobiol Int, 2011, 28(9): 771-778. DOI: 10.3109/07420528.2011.602445. [9] De Souza CM, Hidalgo MP. Midpoint of sleep on school days is associated with depression among adolescents[J]. Chronobiol Int, 2014, 31(2): 199-205. DOI: 10.3109/07420528.2013.838575. [10] Knapen, SE, Riemersma-van der Lek RF, Antypa N, et al. Social jetlag and depression status: results obtained from the Netherlands study of depression and anxiety[J]. Chronobiol Int, 2018, 35(1): 1-7. DOI: 10.1080/07420528.2017.1374966. [11] Roenneberg T, Wirz-Justice A, Merrow, M. Life between clocks: daily temporal patterns of human chronotypes[J]. J Biol Rhythms, 2003, 18(1): 80-90. DOI: 10.1177/0748730402239679. [12] Roenneberg T, Pilz LK, Zerbini G, et al. Chronotype and social jetlag: a(self)-ritical review[J]. Biology, 2019, 8(3): 54. DOI: 10.3390/biology8030054. [13] Zou P, Wang X, Sun L, et al. Semen quality in Chinese college students: associations with depression and physical activity in a cross-sectional study[J]. Psychosom Med, 2018, 80(6): 564-572. DOI: 10.1097/PSY.0000000000000595. [14] 陈卿.睡眠行为、昼夜节律与男(雄)性精液参数的关联研究[D].重庆: 第三军医大学, 2015.Chen Q. Association among sleep behaviors, circadian system and semen parameters in males[D]. Chongqing: Third Military Medical University, 2015. [15] Roenneberg T, Allebrandt KV, Merrow M, et al. Social jetlag and obesity[J]. Curr Biol: CB, 2012, 22(10): 939-943. DOI: 10.1016/j.cub.2012.03.038. [16] Gamble KL, Motsinger-Reif AA, Hida A, et al. Shift work in nurses: contribution of phenotypes and genotypes to adaptation[J]. PLoS One, 2011, 6(4): e18395. DOI: 10.1371/journal.pone.0018395. [17] Kim HI, Lee HJ, Cho CH, et al. Association of CLOCK, ARNTL, and NPAS2 gene polymorphisms and seasonal variations in mood and behavior[J]. Chronobiol Int, 2015, 32(6): 785-791. DOI: 10.3109/07420528.2015.1049613. [18] Bellivier F, Geoffroy PA, Etain B, et al. Sleep-and circadian rhythm-associated pathways as therapeutic targets in bipolar disorder[J]. Expert Opin Ther Targets, 2015, 19(6): 747-763. DOI: 10.1517/14728222.2015.1018822. [19] Salgado-Delgado R, Tapla Osorio A, Saderi N, et al. Disruption of circadian rhythms: a crucial factor in the etiology of depression[J]. Depress Res Treat, 2011, 2011: 1-9. DOI: 10.1155/2011/839743. [20] Gouin JP, Connors J, Kiecolt-Glaser JK, et al. Altered expression of circadian rhythm genes among individuals with a history of depression[J]. J Affect Disord, 2010, 126(1-2): 161-166. DOI: 10.1016/j.jad.2010.04.002. [21] Zhang Z, Cajochen C. Social jetlag and chronotypes in the Chinese population: analysis of data recorded by wearable devices[J]. J Med Internet Res, 2019, 21(6): e13482. DOI: 10.2196/13482. [22] Wittmann M, Dinich J, Merrow M, et al. Social jetlag: misalignment of biological and social time[J]. Chronobiol Int, 2006, 23(1-2): 497-509. DOI: 10.1080/07420520500545979. [23] Zavada A, Gordijn MC, Beersma DG, et al. Comparison of the munich chronotype questionnaire with the Horne-Ostberg's morningness-eveningness score[J]. Chronobiol Int, 2005, 22(2): 267-278. DOI: 10.1081/cbi-200053536. -





 下载:
下载: