A comparative study of differences in cognitive frailty in older adults with different social participation patterns
-
摘要:
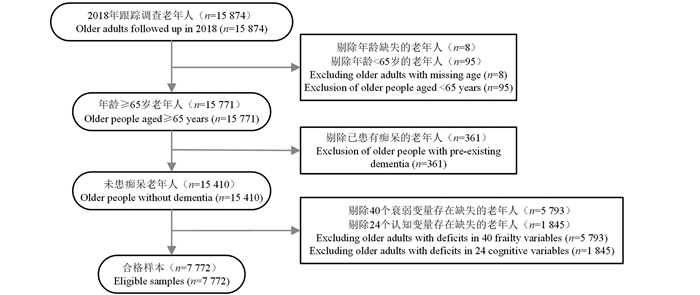
目的 了解老年人认知衰弱现状,并探究不同社会参与模式老年人认知衰弱的差异和影响因素。 方法 利用2018年中国老年人健康影响因素跟踪调查数据,应用多因素非条件logistic回归分析模型和Fairlie分解法对老年人认知衰弱情况进行分析。 结果 7 772名老年人中群体交往型老年人认知衰弱患病率为5.83%,自我消遣型老年人的认知衰弱患病率为21.53%,差异有统计学意义(χ2=426.10, P<0.001)。多因素logistic回归分析模型分析结果显示,低龄、有教育背景、有配偶、较好的经济条件、饮酒、锻炼和有家庭支持是认知衰弱的保护因素。Fairlie分解结果显示,两种社会参与模式的健康差异中55.63%的部分是可由观测因素解释的,而44.37%的健康差异是两种模式本身造成的。 结论 群体交往型老年人认知衰弱情况好于自我消遣型老年人,应鼓励高龄老年人积极参与群体社会活动,加强锻炼,缩小健康差异。 -
关键词:
- 认知衰弱 /
- 社会参与 /
- Fairlie分解法 /
- 老年人
Abstract:Objective To understand the current status of cognitive frailty in older adults, investigating the divergence in cognitive frailty and its contributing factors across various patterns of social participation. Methods Utilizing the 2018 Chinese longitudinal healthy longevity survey, we performed a multi-factor stepwise forward logistic regression analysis and Fairlie decomposition to discern the status of cognitive frailty in older adults. Results The prevalence of cognitive frailty among the 7 772 older adults was 5.83% for the group interaction type and 21.53% for the self-pastime type, with a statistically significant difference (χ2=426.10, P < 0.001). Multifactorial logistic regression results showed that low age, having an educational background, having a spouse, better economic conditions, alcohol drinking, exercising and having family support were protective factors for cognitive frailty. Fairlie decomposition results showed that 55.63% of the health differences between the two social participation patterns were explainable by observed factors, while 44.37% of the health differences were caused by the two patterns themselves. Conclusions The cognitive frailty status was better in group-interactive older adults than in self-pastime older adults. To mitigate health disparities, it is recommended that older adults are encouraged to actively engage in social activities and maintain regular exercise. -
Key words:
- Cognitive frailty /
- Social participation /
- Fairlie decomposition method /
- The elderly
-
表 1 不同特征老年人认知衰弱患病情况比较
Table 1. Comparison of the prevalence of cognitive frailty in older adults with different characteristics
变量Variable 合计Total (n=7 772) 无认知衰弱
Subjects without cognitivefrailty (n=6 954)认知衰弱
Subjects with cognitivefrailty (n=818)χ2值value P值value 年龄组/岁Age group/years 381.09 < 0.001 65~<80 3 212 3 134(45.07) 78(9.54) ≥80 4 560 3 820(54.93) 740(90.46) 性别Sex 84.63 < 0.001 男Male 3 602 3 347(48.13) 255(31.17) 女Female 4 170 3 607(51.87) 563(68.83) 教育背景Education background 265.27 < 0.001 有Yes 4 833 4 538(65.26) 295(36.06) 无No 2 939 2 416(34.74) 523(63.94) 婚姻状况Marital status 259.82 < 0.001 有配偶With spouse 3 635 3 470(49.90) 165(20.17) 无配偶Without spouse 4 137 3 484(50.10) 653(79.83) 经济状况Economic situation 43.31 < 0.001 较好good 6 989 6 307(90.70) 682(83.37) 较差poor 783 647(9.30) 136(16.63) 居住地Residency 0.18 0.674 城镇Urban 4 393 3 925(56.44) 468(57.21) 农村Rural 3 379 3 029(43.56) 350(42.79) 吸烟Smoking status 33.04 < 0.001 是Yes 1 268 1 192(17.14) 76(9.29) 否No 6 504 5 762(82.86) 742(90.71) 饮酒Alcohol drinking 39.36 < 0.001 是Yes 1 224 1 157(16.64) 67(8.19) 否No 6 548 5 797(83.36) 751(91.81) 锻炼Exercise 161.22 < 0.001 是Yes 2 748 2 623(37.72) 125(15.28) 否No 5 024 4 331(62.28) 693(84.72) 社会参与Social participation 426.10 < 0.001 群体交往型Group interaction type 5 450 5 132(73.80) 318(38.88) 自我消遣型Self-pastime type 2 322 1 822(26.20) 500(61.12) 注:①以[人数(占比/%)]表示。
Note: ① [Number of people (proportion/%)].表 2 不同社会参与模式老年人认知衰弱影响因素的多因素logistic回归分析
Table 2. Multifactorial logistic regression analysis of factors influencing cognitive frailty in older adults with different social participation patterns
变量Variable 对照组Control group 群体交往型Group interaction type β sx Wald值value OR值value(95% CI) P值value 年龄组/岁Age group/years ≥80 65~<80 1.359 0.170 64.168 3.892(2.791~5.427) < 0.001 性别Sex 男Male 女Female - - - - - 教育背景Education background 有Yes 无No -0.663 0.125 28.147 0.515(0.403~0.658) < 0.001 婚姻状况Marital status 有配偶With spouse 无配偶Without spouse -0.388 0.146 7.054 0.678(0.509~0.903) 0.008 经济状况Economic situation 较好Good 较差Poor -0.432 0.172 6.310 0.649(0.464~0.909) 0.012 饮酒Alcohol drinking 是Yes 否No -0.394 0.195 4.076 0.675(0.460~0.989) 0.043 锻炼Exercise 是Yes 否No -0.523 0.135 15.048 0.593(0.455~0.772) < 0.001 家庭支持Family support 有Yes 无No -0.569 0.143 15.718 0.566(0.427~0.750) < 0.001 居住地Residency 城镇Urban 农村Rural 0.299 0.123 5.919 1.348(1.060~1.715) 0.015 变量Variable 对照组Control group 自我消遣型Self-pastime type β sx Wald值value OR值 value(95% CI) P值value 年龄组/岁Age group/years ≥80 65~<80 1.347 0.214 39.462 3.845(2.526~5.853) < 0.001 性别Sex 男Male 女Female -0.264 0.129 4.171 0.768(0.596~0.989) 0.041 教育背景Education background 有Yes 无No -0.429 0.119 12.908 0.651(0.515~0.823) < 0.001 婚姻状况Marital status 有配偶With spouse 无配偶Without spouse -0.348 0.151 5.304 0.706(0.525~0.949) 0.021 经济状况Economic situation 较好Good 较差Poor -0.544 0.153 12.627 0.580(0.430~0.784) < 0.001 饮酒Alcohol drinking 是Yes 否No -0.407 0.2 4.118 0.666(0.450~0.986) 0.042 锻炼Exercise 是Yes 否No -0.909 0.181 25.152 0.403(0.282~0.575) < 0.001 家庭支持Family support 有Yes 无No -0.667 0.134 24.815 0.513(0.395~0.667) < 0.001 居住地Residency 城镇Urban 农村Rural - - - - - 注:“-”变量未纳入回归分析。
Note: "-" variable was not included the regression analysis.表 3 不同社会参与模式老年认知衰弱差异的Fairlie分解
Table 3. Fairlie decomposition of differences in cognitive frailty in older adults with different social participation patterns
变量Variable 对照组Control group β 贡献率构成比/%
Composition ratio of the contribution rate /%P值
value总差异Total differences 0.157 100.00 系数效应Coefficient effect 0.070 44.37 特征效应Characteristic effect 0.087 55.63 性别Sex 男Male 女Female 0.003 2.03 0.047 年龄组/岁Age group/years ≥80 65~<80 0.031 20.01 < 0.001 教育背景Education background 有Yes 无No 0.011 6.73 < 0.001 婚姻状况Marital status 有配偶With spouse 无配偶Without spouse 0.006 4.09 0.024 经济状况Economic situation 较好Good 较差Poor 0.003 1.94 0.001 居住地Residency 城镇Urban 农村Rural < 0.001 0.04 0.764 吸烟Smoking status 有Yes 无No 0.001 0.80 0.325 饮酒Alcohol drinking 有Yes 无No 0.002 1.36 0.076 锻炼Exercise 有Yes 无No 0.023 14.50 < 0.001 医疗服务可及性Accessibility of health services 有Yes 无No 0.001 0.53 0.321 家庭支持Family support 有Yes 无No 0.006 3.67 < 0.001 -
[1] Bu ZH, Huang AL, Xue MT, et al. Cognitive frailty as a predictor of adverse outcomes among older adults: a systematic review and meta-analysis[J]. Brain Behav, 2021, 11(1): e01926. DOI: 10.1002/brb3.1926. [2] Kelaiditi E, Cesari M, Canevelli M, et al. Cognitive frailty: rational and definition from an (I.A.N.A. /I.A.G.G. ) international consensus group[J]. J Nutr Health Aging, 2013, 17(9): 726-734. DOI: 10.1007/s12603-013-0367-2. [3] 陈近近, 蒋秋焕, 陈超然, 等. 老年人认知衰弱的研究进展[J]. 护理研究, 2020, 34(4): 669-672. DOI: 10.12102/j.issn.1009-6493.2020.04.021.Chen JJ, Jiang QH, Chen CR, et al. Research progress of cognitive frailty in the elderly[J]. Chinese Nursing Research, 2020, 34(4): 669-672. DOI: 10.12102/j.issn.1009-6493.2020.04.021. [4] Lyu XZ, Li WY, Ma Y, et al. Cognitive decline and mortality among community-dwelling Chinese older people[J]. BMC Med, 2019, 17(1): 63. DOI: 10.1186/s12916-019-1295-8. [5] Dominguez LJ, Veronese N, Vernuccio L, et al. Nutrition, physical activity, and other lifestyle factors in the prevention of cognitive decline and dementia[J]. Nutrients, 2021, 13(11): 4080. DOI: 10.3390/nu13114080. [6] Chiu CJ, Li ML, Chou CY. Trends and biopsychosocial correlates of physical disabilities among older men and women in Taiwan: examination based on ADL, IADL, mobility, and frailty[J]. BMC Geriatr, 2022, 22(1): 148. DOI: 10.1186/s12877-022-02838-6. [7] Ma LN, Zhang L, Zhang YX, et al. Cognitive frailty in China: results from China comprehensive geriatric assessment study[J]. Front Med (lausanne), 2017, 4: 174. DOI: 10.3389/fmed.2017.00174. [8] 周小炫, 谢敏, 陶静, 等. 简易智能精神状态检查量表的研究和应用[J]. 中国康复医学杂志, 2016, 31(6): 694-696, 706. DOI: 10.3969/j.issn.1001-1242.2016.06.019.Zhou XX, Xie M, Tao J, et al. Study and application of the mini-mental state examination[J]. Chin J Rehabil Med, 2016, 31(6): 694-696, 706. DOI: 10.3969/j.issn.1001-1242.2016.06.019. [9] 陈涛. 老年人认知衰弱的年龄与性别差异研究[D]. 济南: 山东大学, 2021.Chen T. Influence of age and gender on cognitive frailty in Chinese older adults[D]. Jinan: Shandong University, 2021. [10] Chen Q, Tang BH, Zhai YH, et al. Dynamic statistical model for predicting the risk of death among older Chinese people, using longitudinal repeated measures of the frailty index: a prospective cohort study[J]. Age Ageing, 2020, 49(6): 966-973. DOI: 10.1093/ageing/afaa056. [11] Sha S, Xu YB, Chen L. Loneliness as a risk factor for frailty transition among older Chinese people[J]. BMC Geriatr, 2020, 20(1): 300. DOI: 10.1186/s12877-020-01714-5. [12] 朱荟. 中国老年人社会参与对其孤独感的影响探究——基于CLHLS 2018数据的验证[J]. 人口与发展, 2021, 27(5): 12-23.Zhu H. On the influence of social participation on loneliness of the elderly in China——based on data of CLHLS 2018[J]. Population and Development, 2021, 27(5): 12-23. [13] Fairlie RW. An extension of the Blinder-Oaxaca decomposition technique to logit and probit models[J]. J Econ Soc Meas, 2005, 30(4): 305-316. DOI: 10.3233/jem-2005-0259. [14] 刘凌晨, 程宏宇, 彭希哲. 中国老年人社会参与模式对认知衰退的影响[J]. 中国人口科学, 2022(4): 103-114. DOI: 10.3969/j.issn.1674-2982.2018.05.001.Liu LC, Cheng HY, Peng XZ. The Influence of Social Participation Model on Cognitive Decline of the Elderly in China[J]. Chin J Popul Sci, 2022(4): 103-114. DOI: 10.3969/j.issn.1674-2982.2018.05.001. [15] Seesen M, Sirikul W, Ruangsuriya J, et al. Cognitive frailty in Thai community-dwelling elderly: prevalence and its association with malnutrition[J]. Nutrients, 2021, 13(12): 2943. DOI: 10.3390/nu13124239. [16] 陈颖勇, 张正敏, 左倩倩, 等. 社区老年人认知衰弱风险预测模型的构建及验证[J]. 中华护理杂志, 2022, 57(2): 197-203. DOI: 10.3761/j.issn.0254-1769.2022.02.012.Chen YY, Zhang ZM, Zuo QQ, et al. Construction and validation of a prediction model for the risk of cognitive frailty among the elderly in a community[J]. Chin J Nurs, 2022, 57(2): 197-203. DOI: 10.3761/j.issn.0254-1769.2022.02.012. [17] Gómez-Gómez ME, Zapico SC. Frailty, cognitive decline, neurodegenerative diseases and nutrition interventions[J]. Int J Mol Sci, 2019, 20(11): 2842. DOI: 10.3390/ijms20112842. [18] Kojima G, Liljas A, Iliffe S, et al. A systematic review and meta-analysis of prospective associations between alcohol consumption and incident frailty[J]. Age Ageing, 2018, 47(1): 26-34. DOI: 10.1093/ageing/afx086. [19] 关欣, 王斗, 乔琳琳, 等. 北京市城乡1018名老年居民衰弱的现况调研及中医证候分析[J]. 中华中医药杂志, 2020, 35(10): 5210-5213. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY202010122.htmGuan X, Wang D, Qiao LL, et al. Investigation of current condition of frailty of 1018 elderly residents in Beiing and analysis of TCM syndromes[J]. China Journal of Traditional Chinese Medicine and Pharmacy, 2020, 35(10): 5210-5213. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY202010122.htm [20] 刘云, 魏利荣, 刘晓凤, 等. 我国养老机构老年人衰弱患病率meta分析[J]. 职业与健康, 2022, 38(22): 3120-3124, 3128. DOI: 10.13329/j.cnki.zyyjk.2022.0646.Liu Y, Wei LR, Liu XF, et al. Meta-analysis on prevalence of frailty among elderly people in elderly care institutions in China[J]. Occup and Health, 2022, 38(22): 3120-3124, 3128. DOI: 10.13329/j.cnki.zyyjk.2022.0646. -





 下载:
下载: