A Meta-analysis of the association between postpartum depression and exclusive breastfeeding in the Chinese population
-
摘要:
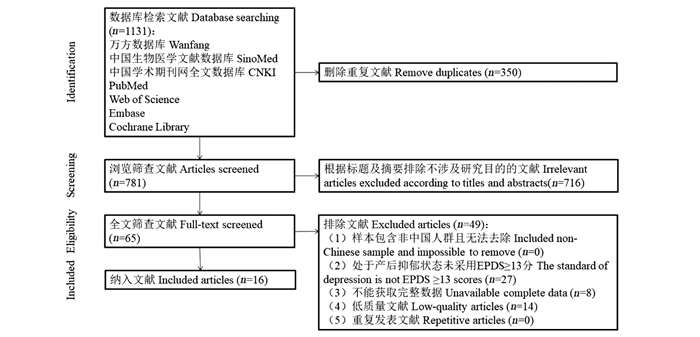
目的 探究中国人群产后抑郁状态与纯母乳喂养的关联强度。 方法 检索万方、SinoMed、知网等数据库,查找中国人群产后抑郁状态与纯母乳喂养情况的观察性研究。采用Stata 12.0软件进行Meta分析。并根据地区、产后时间、分组依据及纳入人群进行亚组分析。 结果 共纳入16篇观察性研究。总体分析抑郁状态组较对照组纯母乳喂养比例低,差异有统计学意义(OR=0.44, 95% CI: 0.36~0.54, P<0.001)。亚组分析提示处于产后抑郁状态的女性纯母乳喂养比例在东部地区显著降低(OR=0.45, 95% CI: 0.36~0.56, P<0.001),在中西部地区也降低(OR=0.41, 95% CI: 0.25~0.66, P<0.001);产后42 d内处于产后抑郁状态的产妇中纯母乳喂养比例降低(OR=0.48, 95% CI: 0.37~0.61, P<0.001),在产后42 d~6月降低更为显著(OR=0.35, 95% CI: 0.21~0.60, P<0.001);去除不同分组依据及纳入人群的研究,剩余研究结果与总体结果差异不大,差异均有统计学意义(OR=0.45, 95% CI: 0.36~0.56, P<0.001)。Meta回归分析提示研究间的异质性地区(P=0.906)、产后时间(P=0.528)、分组依据及纳入人群(P=0.722)差异无统计学意义。 结论 与对照组相比较,产后抑郁状态人群中纯母乳喂养的比例低。为提高中国人群6个月内纯母乳喂养率、降低产后抑郁患病率,建议从产前开始进行孕产期抑郁筛查及多学科协作干预。 Abstract:Objective To explore the relationship between postpartum depression and exclusive breastfeeding (EBF) in the Chinese population. Methods Observational studies about postpartum depression and feeding patterns were searched in databases including Wanfang, SinoMed, CNKI, and so on. Stata 12.0 was used for meta-analysis. Subgroup analysis for both the control and depression populations was performed according to region, postpartum time, and the groups and populations. Results A total of 16 observational studies were included. The rate of EBF in the postpartum depression group was lower than that in the control group, and the difference was statistically significant (OR=0.44, 95% CI: 0.36-0.54, P < 0.001). Subgroup analysis showed that the depression group had a lower EBF rate than the control group in eastern China (OR=0.45, 95% CI: 0.36-0.56, P < 0.001), as well as in central and western China (OR=0.41, 95% CI: 0.25-0.66, P < 0.001). There was a decreased rate of EBF among mothers that had depression within 42 days postpartum (OR=0.48, 95% CI: 0.37-0.61, P < 0.001) and more significantly between 42 days and 6 months postpartum (OR=0.35, 95% CI: 0.21-0.60, P < 0.001). Exclusion of some studies among the different groups and populations did not significantly alter the overall results and the differences were statistically significant (OR=0.45, 95% CI: 0.36-0.56, P < 0.001). Meta-regression analysis suggested that the source of heterogeneity among studies may not be related to the region (P=0.906), postpartum time(P=0.528), or the groups and populations (P=0.722). Conclusions The rate of EBF is lower in the postpartum depression population compared with the control group. To increase the EBF rate within 6 months and reduce the prevalence of postpartum depression in China, we recommend screening for depression during pregnancy and multidisciplinary collaborative intervention starting from the prenatal period. -
Key words:
- Depression /
- Postpartum /
- Breast Feeding /
- Meta-analysis
-
表 1 纳入文献基本特征
Table 1. Characteristics of included studies
年份
Year地区
District研究
Research产后调查时间/d
Postpartum investigation time /dNOS评分
NOS score抑郁状态组Depressive state group 对照组Control group 例数
Number纯母乳喂养
Exclusive breastfeeding混合喂养+人工喂养
Mixed feeding+Artificial feeding例数
Number纯母乳喂养
Exclusive breastfeeding混合喂养+人工喂养
Mixed feeding+Artificial feeding2009 广东广州
Guangdong, Guangzhou王利, 等 [9]
Wang Li, et al [9]42 8 17 3 14 93 50 43 2012 江苏南京
Jiangsu, Nanjing吴江平, 等 [10]
Wu Jiangping, et al [10]42 8 59 13 46 455 176 279 2014 北京
Beijing陈涵 [11]
Chen Han [11]7 7 53 11 42 331 124 207 2014 海南海口
Hainan, Haikou汤琼瑶, 等 [12]
Tang Qiongyao, et al [12]7 7 195 97 98 1 048 714 334 2016 广东深圳
Guangdong, Shenzhen孟利平, 等 [13]
Meng Liping, et al [13]42 8 357 165 192 1 843 1 006 837 2017 江苏苏州
Jiangsu, Suzhou吴贻红, 等 [14]
Wu Yihong, et al [14]14~42 7 114 58 56 508 280 228 2017 广东深圳
Guangdong, Shenzhen王月云, 等 [15]
Wang Yueyun, et al [15]14~60 7 313 100 213 3 221 1 527 1 694 2018 天津
Tianjin宋春华 [16]
Song Chunhua [16]21 8 123 30 93 8 151 3 659 4 492 2018 广东深圳
Guangdong, Shenzhen陈丽珊, 等 [17]
Lishan Chen, et al [17]14~21 7 49 8 41 1 117 551 566 2020 四川泸州
Sichuan, Luzhou张青, 等 [18]
Zhang Qing, et al [18]180 7 111 57 54 337 217 120 2020 上海
ShanghaiYing Liu, et al [19] 42 8 279 134 145 925 504 421 2020 四川成都
Sichuan, Chengdu赖立, 等 [20]
Lai Li, et al [20]30 7 38 28 10 42 37 5 60 38 23 15 42 35 7 90 38 17 21 42 35 7 120 38 14 24 42 31 11 2021 湖北十堰
Hubei, Shiyan李莉, 等 [7]
Li Li, et al [7]60 8 179 27 152 644 98 546 2021 浙江杭州
Zhejiang, Hangzhou马明月, 等 [21]
Ma Mingyue, et al [21]7 7 116 41 75 268 170 98 2021 浙江嘉兴
Zhejiang, Jiaxing王箫, 等 [22]
Wang Xiao, et al [22]42 7 63 32 31 209 150 59 90 63 30 33 211 153 58 180 63 18 45 209 140 69 2022 陕西西安
Shaanxi, Xi′an巨娣, 等 [8]
Ju Di, et al [8]0~90 7 86 16 70 594 227 367 注:NOS, 纽卡斯尔-渥太华量表。
Note: NOS, Newcastle-Ottawa Quality Assessment Scale.表 2 中国人群产后抑郁状态与纯母乳喂养关联强度的亚组分析
Table 2. Subgroup analysis of the association between postpartum depression and EBF in the Chinese population
亚组
Subgroups纳入研究数
Number of included researched样本量
Number of sample抑郁状态组例数
Number of depressive state group对照组例数
Number of the control groupI2/% 异质性检验(P值)
Heterogeneity test (P value)OR值value
(95% CI)P值
value地区District 东部地区East District 12 19 907 1 738 18 169 73.40 <0.001 0.45(0.36~0.56) <0.001 中西部地区Middle and West District 4 2 031 414 1 617 68.20 0.004 0.41(0.25~0.66) <0.001 时间Time 产后≤42 d Postpartum ≤42 d 12 16 453 1 463 14 990 69.80 <0.001 0.48(0.37~0.61) <0.001 产后42 d~6月Postpartum 42 d-6 months 4 2 057 530 1 527 77.80 <0.001 0.35(0.21~0.60) <0.001 分组依据及纳入人群
Grouping standards and including population相同Identical 13 20 996 1 908 19 088 71.6 <0.001 0.45(0.36~0.56) <0.001 不同Unidentical 3 942 244 698 61.9 0.072 0.38(0.22~0.67) 0.001 -
[1] 中国营养学会膳食指南修订专家委员会妇幼人群指南修订. 6月龄内婴儿母乳喂养指南[J]. 临床儿科杂志, 2016, 34(4): 287-291. DOI: 10.3969/j.issn.1000-3606.2016.04.011.Maternal and Child Working Group, Chinese Nutrition Society Expert Committee for Dietary Guidelines. Breastfeeding guidelines for infants up to 6 months of age[J]. J Clin Pediatr, 2016, 34(4): 287-291. DOI: 10.3969/j.issn.1000-3606.2016.04.011. [2] Duan Y, Yang Z, Bi Y, et al. What are the determinants of low exclusive breastfeeding prevalence in China? A cross-sectional study[J]. Matern Child Nutr, 2022, 18(2): e13324. DOI: 10.1111/mcn.13324. [3] Wu W, Zhang J, Silva Zolezzi I, et al. Factors influencing breastfeeding practices in China: A meta-aggregation of qualitative studies[J]. Matern Child Nutr, 2021, 17(4): e13251. DOI: 10.1111/mcn.13251. [4] 中华医学会妇产科学分会产科学组. 围产期抑郁症筛查与诊治专家共识[J]. 中华妇产科杂志, 2021, 56(8): 521-527. DOI: 10.3760/cma.j.cn112141-20210115-00022.Obstetric Subgroup, Society of Obstetrics and Gynecology, Chinese Medical Association. Experts consensus on screening and diagnosis of perinatal depression[J]. Chin J Obstet Gynecol, 2021, 56(8): 521-527. DOI: 10.3760/cma.j.cn112141-20210115-00022. [5] Figueiredo B, Canario C, Field T. Breastfeeding is negatively affected by prenatal depression and reduces postpartum depression[J]. Psychol Med, 2014, 44(5): 927-936. DOI: 10.1017/S0033291713001530. [6] Figueiredo B, Dias CC, Brandao S, et al. Breastfeeding and postpartum depression: state of the art review[J]. J Pediatr, 2013, 89(4): 332-338. DOI: 10.1016/j.jped. [7] 李莉, 任娟. 妇女产后抑郁症发生现状及相关因素研究[J]. 生殖医学杂志, 2021, 30(7): 907-912. DOI: 10.3969/j.issn.1004-3845.2021.07.012.Li L, Ren J. Related factors of postpartum depression in women[J]. Journal of Reproductive Medicine, 2021, 30(7): 907-912. DOI: 10.3969/j.issn.1004-3845.2021.07.012. [8] 巨娣, 田利红, 骆婧, 等. 西安地区孕妇产后抑郁症发生及相关因素分析[J]. 中国计划生育学杂志, 2022, 30(4): 738-742. DOI: 10.3969/j.issn.1004-8189.2022.04.002.Ju D, Tian LH, Luo J, et al. Analysis of the occurrence and the related factors of postpartum depression of pregnant women in Xi'an area[J]. Chin J Fam Plann, 2022, 30(4): 738-742. DOI: 10.3969/j.issn.1004-8189.2022.04.002. [9] 王利, 王利辉, 郭丽. 疾患儿母婴分离产妇抑郁情绪对产后42天母乳喂养率的影响[J]. 临床护理杂志, 2009, 8(6): 2-3, 29. DOI: 10.3969/j.issn.1671-8933.2009.06.001.Wang L, Wang LH, Guo L. The influence of the depression on breast milk feeding in mothers experienced mother-newborn separation[J]. Journal of Clinical Nursing, 2009, 8(6): 2-3, 29. DOI: 10.3969/j.issn.1671-8933.2009.06.001. [10] 吴江平, 梅士娟, 许前珍, 等. 545例产妇产后抑郁相关因素调查[J]. 中国妇幼保健, 2012, 27(6): 889-891. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201206035.htmWu JP, Mei SJ, Xu QZ, et al. Investigation on related factors of postpartum depression in 545 puerpera[J]. Maternal and Child Health Care of China, 2012, 27(6): 889-891. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201206035.htm [11] 陈涵. 产后抑郁症相关因素的调查分析及临床护理[J]. 国际护理学杂志, 2014, 33(2): 271-274. DOI: 10.3760/cma.j.issn.1673-4351.2014.02.011.Chen H. Investigation analysis and clinical nursing of related factors of postpartum depression[J]. International Journal of Nursing, 2014, 33(2): 271-274. DOI: 10.3760/cma.j.issn.1673-4351.2014.02.011. [12] 汤琼瑶, 陈燕娥, 李欣. 产后抑郁症的发病情况调查及其影响因素分析[J]. 中国妇幼保健, 2014, 29(23): 3795-3797. DOI: 10.7620/zgfybj.j.issn.1001-4411.2014.23.37.Tang QY, Chen YE, Li X. Prevalence and influencing factors of postpartum depression[J]. Maternal and Child Health Care of China, 2014, 29(23): 3795-3797. DOI: 10.7620/zgfybj.j.issn.1001-4411.2014.23.37. [13] 孟利平, 杜玉开, 李建梅, 等. 深圳市产妇产后抑郁流行现状及其影响因素[J]. 职业与健康, 2016, 32(16): 2223-2226. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYJK201616022.htmMeng LP, Du YK, Li JM, et al. Epidemic situation and influencing factors of postpartum depression in Shenzhen City[J]. Occupation Health, 2016, 32(16): 2223-2226. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYJK201616022.htm [14] 吴贻红, 赵宗权, 汤振源, 等. 产后抑郁症的筛查及相关因素分析[J]. 川北医学院学报, 2017, 32(4): 610-612. DOI: 10.3969/j.issn.1005-3697.2017.04.036.Wu YH, Zhao ZQ, Tang ZY, et al. Screening of postpartum depression and its high-risk factors[J]. J North Sichuan Medical College, 2017, 32(4): 610-612. DOI: 10.3969/j.issn.1005-3697.2017.04.036. [15] 王月云, 张莉娜, 王红, 等. 深圳市产妇产后抑郁症的流行状况及危险因素分析[J]. 华中科技大学学报(医学版), 2017, 46(6): 704-708. DOI: 10.3870/j.issn.1672-0741.2017.06.019.Wang YY, Zhang LN, Wang H, et al. Prevalence and risk factors of maternal postpartum depression: a cross-sectional study in Shenzhen[J]. Acta Med Univ Sci Technol Huazhong, 2017, 46(6): 704-708. DOI: 10.3870/j.issn.1672-0741.2017.06.019. [16] 宋春华. 天津市城区孕妇产后抑郁症流行状况、危险因素及预测的研究[D]. 天津: 天津医科大学, 2018.Song CH. Study on the prevalence, risk factors and prediction of postpartum depression in Tianjin urban pregnant women[D]. Tianjin: Tianjin Medical University, 2018. [17] 陈丽珊, 王家骥, 杨辉. 深圳市某社区产后抑郁流行情况及危险因素[J]. 职业与健康, 2018, 34(21): 2991-2994. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYJK201821028.htmChen LS, Wang JJ, Yang H. Prevalence and risk factors of postpartum depression in a community in Shenzhen City[J]. Occupation Health, 2018, 34(21): 2991-2994. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYJK201821028.htm [18] 张青, 李世珍, 刘青锋, 等. 四川省泸州市纯母乳喂养现状及其影响因素分析[J]. 华南预防医学, 2020, 46(5): 494-497. DOI: 10.12183/j.scjpm.2020.0494.Zhang Q, Li SZ, Liu QF, et al. Status and influencing factors of exclusive breastfeeding in Luzhou City, Sichuan Province[J]. South China J Prev Med, 2020, 46(5): 494-497. DOI: 10.12183/j.scjpm.2020.0494. [19] Liu Y, Guo N, Li T, et al. Prevalence and associated factors of postpartum anxiety and depression symptoms among women in Shanghai, China[J]. J Affect Disord, 2020, 274: 848-856. DOI: 10.1016/j.jad.2020.05.028. [20] 赖立, 王彩, 陈德娟. 产妇产后抑郁对婴儿喂养方式及婴儿体重的影响调查[J]. 实用预防医学, 2020, 27(7): 842-845. DOI: 10.3969/j.issn.1006-3110.2020.07.020.Lai L, Wang C, Chen DJ. Impact of maternal postpartum depression on infant feeding patterns and infant body weight[J]. Practical Prev Med, 2020, 27(7): 842-845. DOI: 10.3969/j.issn.1006-3110.2020.07.020. [21] 马明月, 周临, 孙增萍, 等. 二胎产妇产后抑郁状况及影响因素分析[J]. 中国妇幼健康研究, 2021, 32(3): 333-337. DOI: 10.3969/j.issn.1673-5293.2021.03.003.Ma MY, Zhou L, Sun ZP, et al. Analysis of postpartum depression and its influencing factors in parturient with a second child[J]. Chinese Journal of Woman and Child Health Research, 2021, 32(3): 333-337. DOI: 10.3969/j.issn.1673-5293.2021.03.003. [22] 王箫, 陈定华, 张莺, 等. 母亲产后抑郁症对儿童体格发育及喂养的影响[J]. 现代实用医学, 2021, 33(11): 1422-1425. DOI: 10.3969/j.issn.1671-0800.2021.11.009.Wang X, Chen DH, Zhang Y, et al. Effects of maternal postpartum depression on children' s physical development and feeding[J]. Modern Pract Med, 2021, 33(11): 1422-1425. DOI: 10.3969/j.issn.1671-0800.2021.11.009. [23] 陈璐, 胡金萍, 拓明花, 等. 产前抑郁与产后抑郁症的相关性[J]. 中华疾病控制杂志, 2020, 24(3): 330-334. DOI: 10.16462/j.cnki.zhjbkz.2020.03.016.Chen L, Hu JP, Tuo MH, et al. Correlation between prenatal depression and postpartum depression[J]. Chin J Dis Control Prev, 2020, 24(3): 330-334. DOI: 10.16462/j.cnki.zhjbkz.2020.03.016. [24] Kim S, Park M, Ahn S. The impact of antepartum depression and postpartum depression on exclusive breastfeeding: a systematic review and meta-analysis[J]. Clin Nurs Res, 2022, 31(5): 866-880. DOI: 10.1177/10547738211053507. [25] Grigoriadis S, Graves L, Peer M, et al. A systematic review and meta-analysis of the effects of antenatal anxiety on postpartum outcomes[J]. Arch Womens Ment Health. 2019, 22(5): 543-556. DOI:10.1007/s00737-018-0930-2.Epub 2018 Dec 6. [26] Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis[J]. J Clin Psychiatry. 2013, 74(4): e321-e341. DOI: 10.4088/JCP.12r07968. [27] Win NN, Binns CW, Zhao Y, et al. Breastfeeding duration in mothers who express breast milk: a cohort study[J]. Int Breastfeed J, 2006, 1: 28. DOI: 10.1186/1746-4358-1-28. -





 下载:
下载: