The association between hypertension disorders in pregnancy and the neurodevelopment of infants: a birth cohort study
-
摘要:
目的 探讨妊娠期高血压疾病(hypertension disorders in pregnancy, HDP)与婴儿神经行为发育的关系。 方法 基于佛山市妇幼保健信息系统出生队列数据,选取2016―2021年在佛山市妇幼保健院产检、分娩的孕产妇及其子代17 812对,采用《0岁~6岁儿童发育行为评估量表》评估婴儿不同月龄的神经行为发育情况。以孕期有HDP暴露史的研究对象为暴露组,采用1∶1倾向性评分匹配对照组,共纳入1 414对母子对。采用广义估计方程分析HDP与婴儿神经行为发育的关系。 结果 HDP组婴儿在3、6、8、12月龄的总发育商和各能区发育商均低于对照组(均P<0.05)。控制混杂因素后,HDP暴露仍是婴儿神经行为发育的危险因素,总发育商的β值(95% CI)为-5.72(-6.80~-4.63);HDP与婴儿大运动(β=-5.35,95% CI:-6.86~-3.84,P<0.01)、精细动作(β=-5.64,95% CI:-6.92~-4.35,P<0.01)、适应能力(β=-5.88,95% CI:-7.26~-4.49,P<0.01)、语言(β=-5.80,95% CI:-7.10~-4.50,P<0.01)和社会行为能区发育商(β=-5.91,95% CI:-7.11~-4.72,P<0.01)降低有关。 结论 HDP是婴儿神经行为发育的危险因素,与婴儿大运动、精细动作、适应能力、语言和社会行为能区发育呈负相关。 Abstract:Objective To investigate the association between hypertension disorders in pregnancy (HDP) and the neurodevelopment of infants. Methods The study utilized birth cohort data from the Foshan maternal and child health information system to select a sample of 17 812 pairs of maternals who received antenatal care at a women and children hospital and their offsprings born at the same facility. The neurodevelopment of the infants was assessed using the Neuropsychological Examination Scale for Chinese Children (NESCC) at various intervals throughout the study. Maternals who were exposed to HDP during gestation were categorized as the exposure group, with the control group selected using a 1:1 propensity score matching method. A total of 1 414 pairs of mothers and children were included in the study. The study employed generalized estimation equations to examine the association between HDP and the neurodevelopmental outcomes of infants. Results The study found that infants exposed to HDP exhibited lower development quotients in total and individual neurodevelopmental domains at 3, 6, 8 and 12 months compared to infants without HDP exposure (all P < 0.05). Even after confounding factors were controlled, HDP exposure remained a significant risk factor for the neurodevelopment of infants, with the partial regression coefficient (β) and (95% CI) of -5.72 (-6.80--4.63). Specifically, HDP exposure was negatively associated with gross motor, fine motor, adaptability, language, and social behavior development, with a partial regression coefficients (β) and 95% CI of -5.35 (-6.86--3.84), -5.64 (-6.92--4.35), -5.88 (-7.26--4.49), -5.80 (-7.10--4.50) and -5.91(-7.11--4.72), respectively. Conclusions HDP has been identified as a risk factor for the neurodevelopment of infants, exhibiting negative associations with the development of gross motor, fine motor, adaptability, language and social behavior -
Key words:
- Hypertension /
- Pregnancy-induced /
- Child development /
- Neurodevelopmental disorders
-
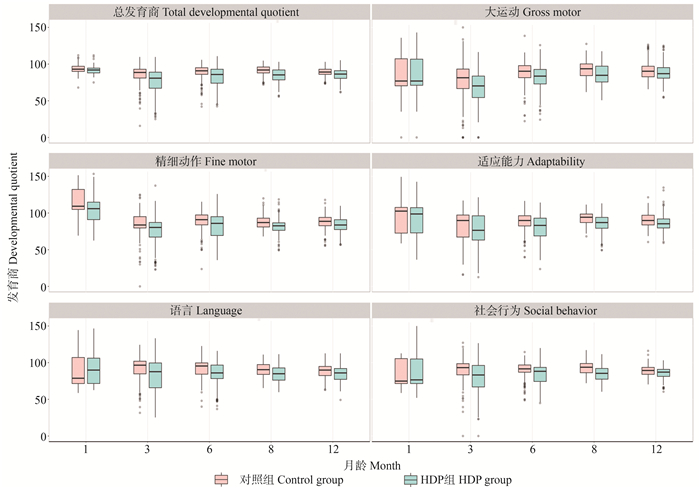
图 1 婴儿各月龄神经行为发育分布箱式图
HDP: 妊娠期高血压疾病; 箱式图的箱体宽度表示样本例数大小,箱体下端、中间和上端线条分别表示第25、50和75百分位数。箱体外上下的线分别表示第5百分位数和第95百分位数。
Figure 1. Box plot of distribution of infants neurodevelopment at each age
HDP: hypertension disorders in pregnancy; The box width represents the sample size, the lower, middle and the upper lines of the box indicate the 25th, 50th, and 75th percentiles, respectively. The lines up and down outside the box indicate the 5th and 95th percentiles.
表 1 研究对象基本特征
Table 1. Characteristics of the study subjects
变量variable 例数
Number(n=1 414)妊娠期高血压疾病 ①
Hypertension disorders in pregnancy ①χ2值
valueP值
value无No 有Yes 母亲相关变量Maternal-related variables 年龄组/岁Age group/years 0.00 1.000 <35 1 032 516(72.98) 516(72.98) ≥35 382 191(27.02) 191(27.02) 分娩方式Mode of delivery 109.36 <0.001 顺产Natural birth 500 344(48.66) 156(22.07) 剖宫产Cesarean birth 914 363(51.34) 551(77.93) 产次Parity 14.67 <0.001 初产妇Primipara 708 318(44.98) 390(55.16) 经产妇Multipara 706 389(55.02) 317(44.84) 胎数Fetal number 17.17 <0.001 单胎Single birth 1 334 685(96.89) 649(91.80) 双胎Twins 80 22(3.11) 58(8.20) BMI/(kg·m-2) 66.77 <0.001 低体重Low weight 105 69(9.76) 36(5.09) 正常体重Normal weight 955 519(73.41) 436(61.67) 超重Overweight 259 101(14.29) 158(22.35) 肥胖Obesity 95 18(2.54) 77(10.89) 妊娠合并糖尿病Pregnancy with diabetes 332 131(18.53) 201(28.43) 19.29 <0.001 妊娠期贫血Anemia in pregnancy 163 86(12.16) 77(10.89) 0.56 0.450 妊娠期甲状腺机能减退Hypothyroidism during pregnancy 119 51(7.21) 68(9.62) 2.65 0.100 婴儿相关变量Infant-related variables 婴儿性别Infant gender 1.50 0.220 男Male 743 383(54.17) 360(50.92) 女Female 671 324(45.83) 347(49.08) 注:①以人数(占比/%)表示。
Note: ① Number of people (proportion/%).表 2 妊娠期高血压疾病与婴儿神经行为发育的关联情况
Table 2. Association of hypertension disorders in pregnancy with the neurodevelopment of infants
模型Model 妊娠期高血压疾病与婴儿发育商的关联
Association of hypertension disorders in pregnancy with developmental quotient in infant总发育商
Total developmental quotient大运动
Gross motor精细动作
Fine motor适应能力
Adaptability语言
Language社会行为
Social behavior模型1 Model 1 -6.55(-7.64~-5.47) -5.68(-7.14~-4.18) -6.88(-8.14~-5.62) -6.63(-8.00~-5.27) -6.81(-8.09~-5.54) -6.78(-7.95~-5.58) P值value <0.01 <0.01 <0.01 <0.01 <0.01 <0.01 模型2 Model 2 -5.58(-6.65~-4.51) -5.00(-6.54~-3.47) -5.64(-6.92~-4.35) -5.65(-7.02~-4.27) -5.81(-7.11~-4.50) -5.82(-7.00~-4.63) P值value <0.01 <0.01 <0.01 <0.01 <0.01 <0.01 模型3 Model 3 -5.72(-6.80~-4.63) -5.35(-6.86~-3.84) -5.64(-6.92~-4.35) -5.88(-7.26~-4.49) -5.80(-7.10~-4.50) -5.91(-7.11~-4.72) P值value <0.01 <0.01 <0.01 <0.01 <0.01 <0.01 注:对照组为无妊娠期高血压疾病((hypertension disorders in pregnancy,HDP)暴露的子代。模型1:HDP与神经行为发育的单因素模型;模型2:调整母亲相关因素(年龄、分娩方式、产次、胎数、BMI、妊娠合并糖尿病、妊娠期贫血、妊娠期甲状腺机能减退);模型3:在模型2的基础上进一步调整了婴儿相关因素(性别、月龄)。
Notes: the control group was the offspring of mothers without hypertension orders of pregnancy (HDP). Model 1: a single-factor model of HDP and the neurodevelopment of infants; Model 2: adjusting for maternal-related factors (including age, mode of delivery, parity, fetal number, BMI, pregnancy with diabetes, anemia in pregnancy, hypothyroidism in pregnancy); Model 3: adjusting for infant-related factors (including gender and month age) further based on model 2. -
[1] Barker DJ, Gluckman PD, Godfrey KM, et al. Fetal nutrition and cardiovascular disease in adult life[J]. Lancet, 1993, 341(8850): 938-941. DOI: 10.1016/0140-6736(93)91224-a. [2] 中华医学会妇产科学分会妊娠期高血压疾病学组. 妊娠期高血压疾病诊治指南(2015)[J]. 中华妇产科杂志, 2015, 50(10): 721-728. DOI: 10.3760/cma.j.issn.0529-567x.2015.10.001.The Group of Hypertension Disorders in Pregnancy of Obstetrics and Gynecology Branch of Chinese Medical Association. Guidelines for the diagnosis and treatment of hypertension disorders in pregnancy(2015)[J]. Chin J Obstet Gynecol, 2015, 50(10): 721-728. DOI: 10.3760/cma.j.issn.0529-567X.2015.10.001. [3] Abalos E, Cuesta C, Grosso AL, et al. Global and regional estimates of preeclampsia and eclampsia: a systematic review[J]. Eur J Obstet Gynecol Reprod Biol, 2013, 170(1): 1-7. DOI: 10.1016/j.ejogrb.2013.05.005. [4] Sun BZ, Moster D, Harmon QE, et al. Association of preeclampsia in term births with neurodevelopmental disorders in offspring[J]. JAMA Psychiatry, 2020, 77(8): 823-829. DOI: 10.1001/jamapsychiatry.2020.0306. [5] Lahti-Pulkkinen M, Girchenko P, Tuovinen S, et al. Maternal hypertensive pregnancy disorders and mental disorders in children[J]. Hypertension, 2020, 75(6): 1429-1438. DOI: 10.1161/HYPERTENSIONAHA.119.14140. [6] Walker SP, Wachs TD, Gardner JM, et al. Child development: risk factors for adverse outcomes in developing countries[J]. Lancet, 2007, 369(9556): 145-157. DOI: 10.1016/S0140-6736(07)60076-2. [7] Obesity: preventing and managing the global epidemic. Report of a WHO consultation[J]. World Health Organ Tech Rep Ser, 2000, 894: 1-253. [8] 中华人民共和国国家卫生健康委员会. 0岁~6岁儿童发育行为评估量表: WS/T 580-2017[S]. 北京: 中国标准出版社, 2017: 1-24.National Health Commission of the People's Republic of China. Developmental behavior assessment scale of children aged from 0 to 6 years: WS/T 580-2017[S]. Beijing: China Standards Press, 2017: 1-24. [9] Thapar A, Cooper M, Rutter M. Neurodevelopmental disorders[J]. Lancet Psychiatry, 2017, 4(4): 339-346. DOI: 10.1016/S2215-0366(16)30376-5. [10] Walker CK, Ashwood P, Hertz-Picciotto I. Preeclampsia, placental insufficiency, autism, and antiphospholipid antibodies-reply[J]. JAMA Pediatr, 2015, 169(6): 606-607. DOI: 10.1001/jamapediatrics.2015.0345. [11] Wang H, László KD, Gissler M, et al. Maternal hypertensive disorders and neurodevelopmental disorders in offspring: a population-based cohort in two Nordic countries[J]. Eur J Epidemiol, 2021, 36(5): 519-530. DOI: 10.1007/s10654-021-00756-2. [12] Palatnik A, Mele LS, Casey BM, et al. Association between hypertensive disorders of pregnancy and long-term neurodevelopmental outcomes in the offspring[J]. Am J Perinatol, 2022, 39(9): 921-929. DOI: 10.1055/a-1692-0659. [13] Bharadwaj SK, Vishnu Bhat B, Vickneswaran V, et al. Oxidative stress, antioxidant status and neurodevelopmental outcome in neonates born to pre-eclamptic mothers[J]. Indian J Pediatr, 2018, 85(5): 351-357. DOI: 10.1007/s12098-017-2560-5. [14] Sala ME, Romero MF, Romero A, et al. Neurodevelopmental assessment of infants born to mothers with hypertensive disorder of pregnancy at six months of age[J]. J Dev Orig Health Dis, 2022, 13(2): 197-203. DOI: 10.1017/S204017442100026X. [15] 牛影. 妊娠期高血压疾病对出生结局及6月龄婴儿发育行为影响的出生队列研究[D]. 合肥: 安徽医科大学, 2016.Niu Y. Relation of pregnancy-related hypertension with birth outcomes and neurodevelpment in early infancy: results from Ma'anshan birth cohort study[D]. Hefei: Anhui Medical University, 2016. [16] Chen Z, Li RZ, Liu H, et al. Impact of maternal hypertensive disorders on offspring's neurodevelopment: a longitudinal prospective cohort study in China[J]. Pediatr Res, 2020, 88(4): 668-675. DOI: 10.1038/s41390-020-0794-9. [17] Noda M, Yoshida S, Mishina H, et al. Association between maternal hypertensive disorders of pregnancy and child neurodevelopment at 3 years of age: a retrospective cohort study[J]. J Dev Orig Health Dis, 2021, 12(3): 428-435. DOI: 10.1017/S2040174420000586. [18] Scime NV, Hetherington E, Tomfohr-Madsen L, et al. Hypertensive disorders in pregnancy and child development at 36 months in the All Our Families prospective cohort study[J]. PLoS One, 2021, 16(12): e0260590. DOI: 10.1371/journal.pone.0260590. [19] Heikura U, Hartikainen AL, Nordström T, et al. Maternal hypertensive disorders during pregnancy and mild cognitive limitations in the offspring[J]. Paediatr Perinat Epidemiol, 2013, 27(2): 188-198. DOI: 10.1111/ppe.12028. [20] Thompson RA, Nelson CA. Developmental science and the media. Early brain development[J]. Am Psychol, 2001, 56(1): 5-15. DOI: 10.1037/0003-066x.56.1.5. -





 下载:
下载: