The causal association between ischemic stroke and the risk of membranous nephropathy based on two-sample Mendelian randomization
-
摘要:
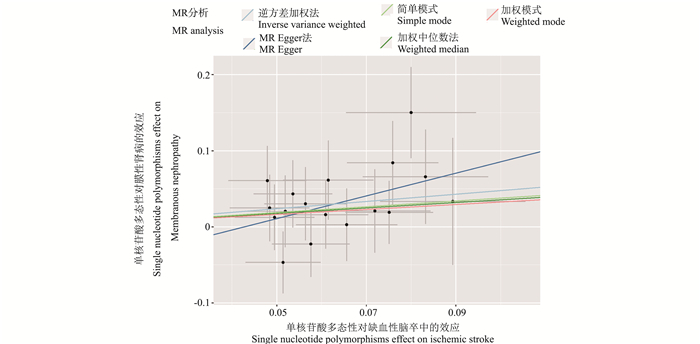
目的 采用两样本孟德尔随机化(Mendelian randomization,MR)方法探讨缺血性脑卒中和膜性肾病发病之间的因果关系。 方法 从全基因组关联分析研究数据中筛出相互独立且与缺血性脑卒中密切相关的单核苷酸多态性(single nucleotide polymorphisms,SNPs)作为工具变量,以比值比作为评估指标,并采用逆方差加权法、加权中位数法和MR-Egger法探讨缺血性脑卒中和膜性肾病发病的因果关联。 结果 本研究共筛选到17个缺血性脑卒中相关的SNPs。逆方差加权法分析结果显示缺血性脑卒中是膜性肾病的危险因素(OR=1.61,95% CI: 1.11~2.33,P=0.01)。敏感性分析与主分析结果一致,证实了研究的稳健性,异质性检验表明SNPs不存在异质性。 结论 从遗传学角度,本研究提示缺血性脑卒中和膜性肾病存在关联。因此,加强对缺血性脑卒中患者膜性肾病的筛查和预防具有重要的指导意义,可降低缺血性脑卒中患者发生膜性肾病的风险。 Abstract:Objective To investigate the causal relationship between ischemic stroke and incidence of membranous nephropathy using a Two-sample Mendelian randomization (MR) method. Methods Single nucleotide polymorphisms (SNPs), which were independent of each other and closely associated with ischemic stroke were identified from a Genome-Wide Association analysis. The identified SNPs were used as instrumental variables. Odds ratios were obtained from the MR analyses on the causal association between ischemic stroke and membranous nephropathy using the inverse variance weighted analysis, weighted median method, and MR-Egger method. Results A total of 17 SNPs that were associated with ischemic stroke were identified in this study. The inverse variance weighted analysis showed that ischemic stroke was associated with higher risk of membranous nephropathy (OR=1.61, 95% CI: 1.11-2.33, P=0.01). Results of the sensitivity analysis were consistent with those of the main analysis, confirming the robustness of this study. No heterogeneity among SNPs was observed in this study. Conclusions From a genetic perspective, the present study suggested an association between ischaemic stroke and elevated risk of membranous nephropathy. Strengthening screening and prevention of membranous nephropathy among patients diagnosed with ischemic stroke is of great clinical and public health significance. -
Key words:
- Ischemic stroke /
- Membranous nephropathy /
- Mendelian randomization /
- Causal inference
-
表 1 缺血性脑卒中和膜性肾病的SNPs特征
Table 1. The SNPs features of ischemic stroke and membranous nephropathy
序号
No.SNPs CHR EA OA 和IS的关系Association with IS 和MN的关系Association with MN β值value sx P值value F值value β值value sx P值value 1 rs1052053 1 G A -0.06 0.01 <0.05 43.83 0.02 0.04 <0.05 2 rs1053007 19 G A 0.05 0.01 <0.05 30.31 0.06 0.05 <0.05 3 rs11957829 5 G A -0.07 0.01 <0.05 33.62 -0.02 0.05 <0.05 4 rs12445022 16 A G 0.06 0.01 <0.05 41.09 0.02 0.04 <0.05 5 rs17035646 1 A G 0.05 0.01 <0.05 37.10 0.04 0.04 <0.05 6 rs2005108 11 T C 0.08 0.01 <0.05 30.44 0.15 0.06 <0.05 7 rs2107595 7 A G 0.08 0.01 <0.05 55.37 0.08 0.05 <0.05 8 rs3184504 12 C T -0.08 0.01 <0.05 58.73 -0.02 0.04 <0.05 9 rs35436 12 T C -0.05 0.01 <0.05 30.93 -0.01 0.04 <0.05 10 rs42039 7 T C -0.07 0.01 <0.05 33.70 0.00 0.05 <0.05 11 rs4932370 15 A G 0.05 0.01 <0.05 30.48 0.02 0.05 <0.05 12 rs4959130 6 A G 0.08 0.01 <0.05 35.32 0.07 0.06 <0.05 13 rs6825454 4 C T 0.06 0.01 <0.05 37.58 0.03 0.05 <0.05 14 rs7304841 12 C A -0.05 0.01 <0.05 29.57 -0.02 0.04 <0.05 15 rs7859727 9 T C 0.05 0.01 <0.05 37.44 -0.05 0.04 <0.05 16 rs9526212 13 G A 0.06 0.01 <0.05 37.08 0.06 0.05 <0.05 17 rs9909858 17 C T 0.09 0.02 <0.05 30.39 0.03 0.08 <0.05 注:SNPs,单核苷酸多态性;CHR,染色体号;EA,效应等位基因;OA,非效应等位基因;IS,缺血性脑卒中; MN,膜性肾病。
Note:SNPs,single nucleotide polymorphisms;CHR,chromosome number;EA,effector allele;OA,non-effect allele; IS, ischemic stroke; MN, membranous nephropathy.表 2 3种MR分析方法
Table 2. Three MR analysis methods
MR方法methods SNPs β值value sx OR值value(95% CI) P值value IVW 17 0.476 0.189 1.61(1.11~2.33) 0.01 MR-Egger 17 1.493 1.022 4.45(0.60~33.02) 0.16 加权中位数Weighted median 17 0.355 0.255 1.43(0.87~2.35) 0.16 注:MR, 孟德尔随机化; IVW, 逆方差加权法; SNPs, 单核苷酸多态性。
Note:MR, mendelian randomization; IVW, Inverse variance weighting method; SNPs, single nucleotide polymorphisms. -
[1] Li JN, Cui Z, Long JY, et al. Primary glomerular nephropathy among hospitalized patients in a national database in China[J]. Nephrol Dial Transplant, 2018, 33(12): 2173-2181. DOI: 10.1093/ndt/gfy022. [2] Xu X, Wang GB, Chen N, et al. Long-term exposure to air pollution and increased risk of membranous nephropathy in China[J]. J Am Soc Nephrol, 2016, 27(12): 3739-3746. DOI: 10.1681/ASN.2016010093. [3] 张慧, 杨薇, 魏丹, 等. 中国终末期肾病患者认知障碍影响因素的Meta分析[J]. 中国全科医学, 2022, 25(21): 2651-2660. DOI: 10.12114/j.issn.1007-9572.2022.0203.Zhang H, Yang W, Wei D, et al. Factors associated with cognitive impairment in Chinese patients with end-stage renal disease: a meta-analysis[J]. Chin Gen Prac, 2022, 25(21): 2651-2660. DOI: 10.12114/j.issn.1007-9572.2022.0203. [4] Feigin VL, Owolabi MO. Pragmatic solutions to reduce the global burden of stroke: a world stroke organization-lancet neurology commission[J]. Lancet Neurology, 2023, 22(12): 1160-1206. DOI: 10.1016/S1474-4422(23)00277-6. [5] Kumai Y, Kamouchi M, Hata J, et al. Proteinuria and clinical outcomes after ischemic stroke[J]. Neurology, 2012, 78(24): 1909-1915. DOI: 10.1212/WNL.0b013e318259e110. [6] Chwojnicki K, Król E, Wierucki Ł, et al. Renal dysfunction in post-stroke patients[J]. PLoS One, 2016, 11(8): e0159775. DOI: 10.1371/journal.pone.0159775. [7] Zou HH, Li YB, Xu GS. Management of anticoagulation and antiplatelet therapy in patients with primary membranous nephropathy[J]. BMC Nephrol, 2019, 20(1): 442. DOI: 10.1186/s12882-019-1637-y. [8] 和思敏, 张雨, 彭刘庆, 等. 倾向性评分与孟德尔随机化国内研究现状[J]. 中华疾病控制杂志, 2022, 26(3): 325-330. DOI: 10.16462/j.cnki.zhjbkz.2022.03.014.He SM, Zhang Y, Peng LQ, et al. Research progress of propensity score and Mendelian randomization in China[J]. Chin J Dis Control Prev, 2022, 26(3): 325-330. DOI: 10.16462/j.cnki.zhjbkz.2022.03.014. [9] Malik R, Chauhan G, Traylor M, et al. Publisher Correction: Multiancestry genome-wide association study of 520, 000 subjects identifies 32 loci associated with stroke and stroke subtypes[J]. Nat Genet, 2019, 51(7): 1192-1193. DOI: 10.1038/s41588-019-0449-0. [10] Xie JY, Liu LL, Mladkova N, et al. The genetic architecture of membranous nephropathy and its potential to improve non-invasive diagnosis[J]. Nat Commun, 2020, 11(1): 1600. DOI: 10.1038/s41467-020-15383-w. [11] Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data[J]. Genet Epidemiol, 2013, 37(7): 658-665. DOI: 10.1002/gepi.21758. [12] Bowden J, Davey Smith G, Haycock PC, et al. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted Median estimator[J]. Genet Epidemiol, 2016, 40(4): 304-314. DOI: 10.1002/gepi.21965. [13] Zhang Y, Liu ZP, Choudhury T, et al. Habitual coffee intake and risk for nonalcoholic fatty liver disease: a two-sample Mendelian randomization study[J]. Eur J Nutr, 2021, 60(4): 1761-1767. DOI: 10.1007/s00394-020-02369-z. [14] Weiner DE, Tighiouart H, Amin MG, et al. Chronic kidney diease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies[J]. J Am Soc Nephrol, 2004, 15(5): 1307-1315. DOI: 10.1097/01.asn.0000123691.46138.e2. [15] Zhang J, Shu JL, You Q, et al. Ischemic stroke in anti-phospholipase A2 receptor antibody-positive primary membranous nephropathy: clinical and neuroimaging characteristics[J]. Chin Med J, 2020, 133(3): 361-363. DOI: 10.1097/CM9.0000000000000610. [16] Hoxha E, Reinhard L, Stahl RAK. Membranous nephropathy: new pathogenic mechanisms and their clinical implications[J]. Nat Rev Nephrol, 2022, 18(7): 466-478. DOI: 10.1038/s41581-022-00564-1. [17] Zhang CY, Wang XB, He ML, et al. Proteinuria is an independent risk factor for first incident stroke in adults under treatment for hypertension in China[J]. J Am Heart Assoc, 2015, 4(12): e002639. DOI: 10.1161/JAHA.115.002639. [18] Pallavi R, Sunggeun L, Baumstein D, et al. Stroke in a young woman as a presenting manifestation of membranous nephropathy[J]. Am J Ther, 2016, 23(3): e950-e954. DOI: 10.1097/MJT.0000000000000075. [19] Mohammadian R, Tarighatnia A, Naghibi M, et al. Vertebrobasilar artery stroke as the heralding sign of systemic lupus erythematosus[J]. J Stroke Cerebrovasc Dis, 2018, 27(5): e80-e85. DOI: 10.1016/j.jstrokecerebrovasdis.2017.12.003. [20] Campbell BCV, Mitchell PJ, Churilov L, et al. Tenecteplase versus alteplase before thrombectomy for ischemic stroke[J]. N Engl J Med, 2018, 378(17): 1573-1582. DOI: 10.1056/NEJMoa1716405. [21] Hârza M, Ismail G, Mitroi G, et al. Histological diagnosis and risk of renal vein thrombosis, and other thrombotic complications in primitive nephrotic syndrome[J]. Rom J Morphol Embryol, 2013, 54: 555-560. DOI: 2013;54(3):555-560. [22] Xie Z, Tong S, Chu X, et al. Chronic kidney disease and cognitive impairment: the kidney-brain axis[J]. Kidney Dis(Basel), 2022, 8(4): 275-285. DOI: 10.1159/000524475. [23] El Husseini N, Fonarow GC, Smith EE, et al. Association of kidney function with 30-day and 1-year poststroke mortality and hospital readmission[J]. Stroke, 2018, 49(12): 2896-2903. DOI: 10.1161/STROKEAHA.118.022011. [24] Zhao Q, Yan T, Chopp M, et al. Brain-kidney interaction: renal dysfunction following ischemic stroke[J]. J Cereb Blood Flow Metab, 2020, 40(2): 246-262. DOI: 10.1177/0271678X19890931. -





 下载:
下载: