Persistent carriage of Streptococcus pneumoniae and its influencing factors among children in kindergartens
-
摘要:
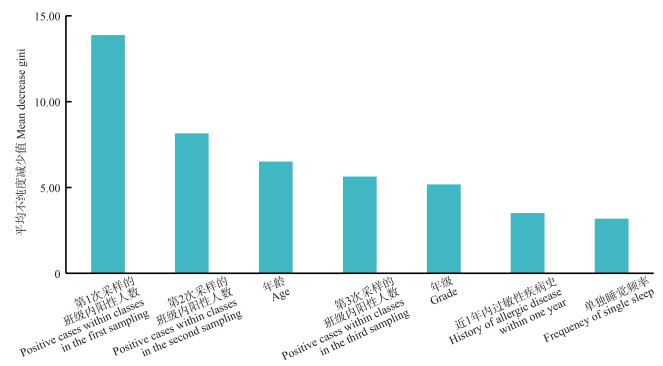
目的 探索幼儿园儿童肺炎链球菌的持续携带状况及其影响因素。 方法 采用多阶段分层整群抽样方法,抽取佛山市顺德区6所幼儿园的健康儿童,对所有儿童进行3次鼻拭子采样并分离鉴定肺炎链球菌。采用单因素χ2检验和多因素logistic回归分析模型分析儿童肺炎链球菌持续携带的影响因素。鉴于3次采样的班级内阳性数具有不独立性且相关性较强,本研究分别拟合3个多因素logistic回归分析模型(即模型1~3)。除“班级内阳性人数”变量外,3个模型在控制混杂因素及分析方法上保持一致。运用随机森林模型对肺炎链球菌持续携带相关的影响因素进行重要性排序。 结果 儿童肺炎链球菌持续携带率为6.6%。模型1的多因素logistic回归分析结果表明:班级内阳性人数越多,肺炎链球菌持续携带率越高且呈现单调递增趋势。以0~<4人阳性组为对照,其他组的OR分别为2.35(95% CI : 1.12~4.90,P=0.023)、5.86(95% CI : 2.75~12.49,P < 0.001)、9.43(95% CI : 4.68~19.02,P < 0.001);随着儿童年龄的增长,肺炎链球菌持续携带率呈现递减趋势。以0~<3岁组为对照,其他组OR分别为0.38(95% CI : 0.20~0.72,P=0.003)、0.29(95% CI : 0.15~0.55,P < 0.001)、0.29(95% CI : 0.14~0.60,P=0.001);近1年内过敏性疾病史是肺炎链球菌持续携带的保护因素(OR=0.44, 95% CI : 0.20~0.98,P=0.045)。模型2和模型3的研究结果与模型1基本一致。 结论 班级内阳性人数增多是幼儿园儿童肺炎链球菌持续携带的重要危险因素;年龄的增长与近1年内过敏性疾病史是幼儿园儿童肺炎链球菌持续携带的保护因素。 Abstract:Objective To explore the prevalence and influencing factors of persistent carriage of Streptococcus pneumoniae (S. pneumoniae) in kindergarten children. Methods A multi-stage stratified cluster sampling method was used in this study. Healthy children were sampled from six kindergartens in Shunde District, Foshan City. All children underwent three nasal swab samplings, followed by isolation and identification of S. pneumoniae. Univariate chi-square tests and multivariate logistic regression analysis models were used to analyze the factors influencing persistent carriage of S. pneumoniae in children. Given the non-independence and strong correlation of the number of positive cases within classes across three samples, this study has developed three separate multivariable logistic regression analysis models (namely, models 1 to 3). Apart from the variable "number of positive cases within the class", all three models maintain consistency in controlling for confounding factors and in the analytical methods used. A random forest model was applied to rank the importance of factors associated with persistent carriage of S. pneumoniae. Results The persistence carriage rate of S. pneumoniae in children was 6.6%. The results of the multivariable logistic regression analysis in model 1 indicated that a higher number of positive cases within a class was associated with an increased rate of persistent carriage of S. pneumoniae, showing a monotonic increasing trend. Compared to the group with 0 to < 4 positive cases, the odds ratios for other groups were 2.35 (95% CI: 1.12-4.90, P=0.023), 5.86 (95% CI: 2.75-12.49, P < 0.001), and 9.43 (95% CI: 4.68-19.02, P < 0.001), respectively. The rate of persistent carriage of S. pneumoniae decreased with increasing age. Compared to the group aged 0 to < 3 years, the odds ratios for other age groups were 0.38 (95% CI: 0.20-0.72, P=0.003), 0.29 (95% CI: 0.15-0.55, P < 0.001), and 0.29 (95% CI: 0.14-0.60, P=0.001), respectively. A history of allergic diseases within the past year was identified as a protective factor for the persistent carriage of S. pneumoniae, with an odds ratio of 0.44 (95% CI: 0.20-0.98, P=0.045). The findings from models 2 and 3 were consistent with those from model 1. Conclusions An increased number of positive cases within a class is a significant risk factor for the persistent carriage of S. pneumoniae among kindergarten children; whereas, an increase in age and a history of allergic diseases within the past year serve as protective factors against the persistent carriage of S. pneumoniae in this population. -
Key words:
- Streptococcus pneumoniae /
- Carriage /
- Influencing factors /
- Child
-
表 1 基本人口学特征与肺炎链球菌持续携带的关系
Table 1. Association between basic characteristics and persistent carriage of S. pneumoniae
影响因素Impact factors 人数Number of people 携带人数(占比/%) Number of carriers (proportion/%) χ2值value P值value 性别Gender 0.09 0.767 男Male 873 59(6.8) 女Female 720 46(6.4) 年龄组/岁Age group/years 32.70 < 0.001 ① 0~<3 106 20(18.9) 3~<4 379 35(9.2) 4~<5 496 27(5.4) 5~7 612 23(3.8) 年级Grade 29.02 < 0.001 ① 小班Junior class 521 59(11.3) 中班Middle class 504 28(5.6) 大班Senior class 568 18(3.2) 地区Area 2.31 0.128 城镇Rural 736 41(5.6) 农村Urban 857 64(7.5) 户籍Household registration 0.26 0.608 佛山市Foshan 918 58(6.3) 其他Others 675 47(7.0) 民族Nationality 0.01 0.906 汉族Han 1 506 99(6.6) 其他Others 87 6(6.9) 早产儿Premature infant 0.02 0.900 是Yes 80 5(6.3) 否No 1 513 100(6.6) 父亲文化程度Father′s education 0.45 0.789 初中及以下Junior high school and below 471 30(6.4) 高中/中专High/technical secondary school 652 41(6.3) 大学及以上College and above 470 34(7.2) 母亲文化程度Mother′s education 0.37 0.830 初中及以下Junior high school and below 491 30(6.1) 高中/中专High/technical secondary school 568 40(7.0) 大学及以上College and above 534 35(6.6) 第1次采样的班级内阳性人数/人Positive cases within classes in the first sampling 79.23 < 0.001 ① 0~<4 524 11(2.1) 4~<7 635 27(4.3) 7~<10 187 22(11.8) 10~16 247 45(18.2) 第2次采样的班级内阳性人数/人Positive cases within classes in the second sampling 43.46 < 0.001 ① 0~<4 335 6(1.8) 4~<7 564 27(4.8) 7~<10 320 20(6.3) 10~16 374 52(13.9) 第3次采样的班级内阳性人数/人Positive cases within classes in the third sampling 10.36 0.001 ① 0~<4 348 14(4.0) 4~<7 468 24(5.1) 7~<10 499 41(8.2) 10~18 278 26(9.4) 注:①趋势χ2检验。
Note: ① Chi-square test of trend.表 2 医院/社区相关因素与肺炎链球菌持续携带的关系
Table 2. Association between hospital/community factors and persistent carriage of S. pneumoniae
影响因素Impact factors 人数Number of people 携带人数(占比) Number of carriers (proportion/%) χ2值value P值value 近1年内过敏性疾病史History of allergic disease within one year 4.82 0.028 有Yes 220 7(3.2) 无No 1 373 98(7.1) 近1年内医院相关暴露史Hospital-related exposure within one year 0.89 0.345 有Yes 115 10(8.7) 无No 1 478 95(6.4) 近1年内家庭成员医院相关暴露史Hospital-related exposures in family members within one year 1.55 0.214 有Yes 250 12(4.8) 无No 1 343 93(6.9) 肺炎链球菌结合疫苗接种史History of PCV vaccination 0.12 0.941 有Yes 488 32(6.6) 无No 642 41(6.4) 不详Unknown 463 32(6.9) b型流感嗜血疫苗接种史History of Hib vaccination 0.01 0.995 有Yes 355 23(6.5) 无No 784 52(6.6) 不详Unknown 454 30(6.6) 单独睡觉频率Frequency of single sleep 4.13 0.042 ① 否No 1 395 98(7.0) 偶尔Occasionally 99 5(5.1) 经常Often 99 2(2.0) 参加托管班/兴趣班Care/Interest classes 1.35 0.245 有Yes 522 29(5.6) 无No 1 071 76(7.1) 宠物接触史History of pet exposure 3.99 0.136 否No 1 180 79(6.7) 偶尔Occasionally 360 26(7.2) 经常Often 53 0(0.0) 呼吸道感染史-抗生素使用史Respiratory infection and antibiotic use 0.50 0.920 有感染有用药Infection and use 423 28(6.6) 有感染无用药Infection but non-use 558 36(6.5) 无感染有用药Non-infection but use 28 1(3.6) 无感染无用药Non-infection and non-use 584 40(6.9) 同住小孩数/人Number of children living together 2.11 0.146 0 99 10(10.1) ≥1 1 494 95(6.4) 注:①趋势χ2检验。
Note: ① Chi-square test of trend.表 3 肺炎链球菌持续携带的多因素logistic回归分析模型
Table 3. Multivariate logistic regression models for persistent carriage of S. pneumoniae
模型Model 影响因素Impact factors β值value SE Wald值value OR值value (95% CI) P值value 模型1 Model 1 年龄组/岁Age group/years 0~<3 1.00 3~<4 -0.98 0.33 -2.95 0.38(0.20~0.72) 0.003 4~<5 -1.25 0.33 -3.77 0.29(0.15~0.55) < 0.001 5~7 -1.23 0.36 -3.38 0.29(0.14~0.60) 0.001 第1次采样的班级内阳性人数/人Positive cases within classes in the first sampling 0~<4 1.00 4~<7 0.85 0.38 2.27 2.35(1.12~4.90) 0.023 7~<10 1.77 0.39 4.58 5.86(2.75~12.49) < 0.001 10~16 2.24 0.36 6.27 9.43(4.68~19.02) < 0.001 近1年内过敏性疾病史History of allergic disease within one year -0.82 0.41 -2.01 0.44(0.20~0.98) 0.045 单独睡觉频率Frequency of single sleep 0.34 0.28 1.21 1.41(0.81~2.46) 0.228 模型2 Model 2 年龄组/岁Age group/years 0~<3 1.00 3~<4 -0.95 0.32 -2.96 0.39(0.21~0.73) 0.003 4~<5 -1.39 0.33 -4.28 0.25(0.13~0.47) < 0.001 5~7 -1.41 0.34 -4.16 0.24(0.13~0.47) < 0.001 第2次采样的班级内阳性人数/人Positive cases within classes in the second sampling 0~<4 1.00 4~<7 1.03 0.46 2.23 2.81(1.13~6.94) 0.026 7~<10 1.32 0.48 2.77 3.75(1.47~9.55) 0.006 10~16 2.03 0.45 4.53 7.61(3.16~18.32) < 0.001 近1年内过敏性疾病史History of allergic disease within one year -0.77 0.40 -1.90 0.46(0.21~1.02) 0.057 单独睡觉频率Frequency of single sleep 0.35 0.29 1.21 1.42(0.81~2.48) 0.226 模型3 Model 3 年龄组/岁Age group/years 0~<3 1.00 3~<4 -0.74 0.31 -2.41 0.48(0.26~0.87) 0.016 4~<5 -1.28 0.32 -3.96 0.28(0.15~0.52) < 0.001 5~7 -1.61 0.33 -4.81 0.20(0.10~0.39) < 0.001 第3次采样的班级内阳性人数/人Positive cases within classes in the third sampling 0~<4 1.00 4~<7 0.39 0.35 1.12 1.48(0.75~2.93) 0.261 7~<10 0.76 0.32 2.36 2.14(1.14~4.02) 0.018 10~18 0.80 0.35 2.31 2.23(1.13~4.40) 0.021 近1年内过敏性疾病史History of allergic disease within one year -0.82 0.40 -2.04 0.44(0.20~0.97) 0.041 单独睡觉频率Frequency of single sleep 0.40 0.28 1.41 1.49(0.85~2.60) 0.159 -
[1] Daningrat WOD, Amalia H, Ayu IM, et al. Carriage of Streptococcus pneumoniae in children under five years of age prior to pneumococcal vaccine introduction in Southeast Asia: a systematic review and meta-analysis (2001-2019)[J]. J Microbiol Immunol Infect, 2022, 55(1): 6-17. DOI: 10.1016/j.jmii.2021.08.002. [2] Chaguza C, Senghore M, Bojang E, et al. Within-host microevolution of Streptococcus pneumoniae is rapid and adaptive during natural colonisation[J]. Nat Commun, 2020, 11(1): 3442. DOI: 10.1038/s41467-020-17327-w. [3] Subramanian K, Henriques-Normark B, Normark S. Emerging concepts in the pathogenesis of the Streptococcus pneumoniae: from nasopharyngeal colonizer to intracellular pathogen[J]. Cell Microbiol, 2019, 21(11): e13077. DOI: 10.1111/cmi.13077. [4] Kielbik K, Pietras A, Jablonska J, et al. Impact of pneumococcal vaccination on nasopharyngeal carriage of Streptococcus pneumoniae and microbiota profiles in preschool children in South East Poland[J]. Vaccines, 2022, 10(5): 791. DOI: 10.3390/vaccines10050791. [5] Hu JY, Sun XD, Huang ZY, et al. Streptococcus pneumoniae and Haemophilus influenzae type b carriage in Chinese children aged 12-18 months in Shanghai, China: a cross-sectional study[J]. BMC Infect Dis, 2016, 16: 149. DOI: 10.1186/s12879-016-1485-3. [6] 邝兆威. 东莞地区学龄前儿童肺炎链球菌携带的调查分析[J]. 国际检验医学杂志, 2016, 37(14): 1973-1974. DOI: 10.3969/j.issn.1673-4130.2016.14.029.Kuang ZW. Investigation and analysis on preschool children carrying Streptococcus pneumoniae in Dongguan area[J]. Int J Lab Med, 2016, 37(14): 1973-1974, 1976. DOI: 10.3969/j.issn.1673-4130.2016.14.029. [7] Paudel G, Amatya N, Saud B, et al. Nasal colonization by potential bacterial pathogens in healthy kindergarten children of Nepal: a prevalence study[J]. Germs, 2022, 12(1): 86-98. DOI: 10.18683/germs.2022.1309. [8] Kartasasmita CB, Hadinegoro SR, Kurniati N, et al. Epidemiology, nasopharyngeal carriage, serotype prevalence, and antibiotic resistance of Streptococcus pneumoniae in Indonesia[J]. Infect Dis Ther, 2020, 9(4): 723-736. DOI: 10.1007/s40121-020-00330-5. [9] Gupta P, Awasthi S, Gupta U, et al. Nasopharyngeal carriage of Streptococcus pneumoniae serotypes among healthy children in northern India[J]. Curr Microbiol, 2022, 80(1): 41. DOI: 10.1007/s00284-022-03114-x. [10] Shahid S, Nisar MI, Jehan F, et al. Co-carriage of Staphylococcus aureus and Streptococcus pneumoniae among children younger than 2 years of age in a rural population in Pakistan[J]. Clin Epidemiol Glob Health, 2023, 21: None. DOI: 10.1016/j.cegh.2023.101293. [11] 王旭麟, 陈敏琪, 李文宇, 等. 幼儿园儿童肺炎链球菌携带的聚集性及影响因素分析[J]. 中国当代儿科杂志, 2021, 23(4): 363-368. DOI: 10.7499/j.issn.1008-8830.2011078.Wang XL, Chen MQ, Li WY, et al. Clustering and influencing factors of Streptococcus pneumoniae carriage among kindergarten children[J]. Chin J Contemp Pediatr, 2021, 23(4): 363-368. DOI: 10.7499/j.issn.1008-8830.2011078. [12] 陈燕辉, 陈晓媚, 杨晓华, 等. 2016年中山市6~13岁学龄儿童鼻咽部肺炎链球菌携带情况及药物敏感性分析[J]. 实用预防医学, 2018, 25(5): 554-556. DOI: 10.3969/j.issn.1006-3110.2018.05.011.Chen YH, Chen XM, Yang XH, et al. Prevalence and drug susceptibility of Streptococcus pneumoniae isolated in the nasopharynx of school children aged 6-13 years in Zhongshan City, 2016[J]. Pract Prev Med, 2018, 25(5): 554-556. DOI: 10.3969/j.issn.1006-3110.2018.05.011. [13] Pan H, Cui BL, Huang YC, et al. Nasal carriage of common bacterial pathogens among healthy kindergarten children in Chaoshan region, southern China: a cross-sectional study[J]. BMC Pediatr, 2016, 16(1): 161. DOI: 10.1186/s12887-016-0703-x. [14] Mustapha MM, Marsh JW, Shutt KA, et al. Transmission dynamics and microevolution of Neisseria meningitidis during carriage and invasive disease in high school students in Georgia and Maryland, 2006-2007[J]. J Infect Dis, 2021, 223(12): 2038-2047. DOI: 10.1093/infdis/jiaa674. [15] Olof S, Lorraine E, Idosa BA, et al. Prevalence and persistence of Neisseria meningitidis carriage in Swedish university students[J]. Epidemiol Infect, 2023, 151: e25. DOI: 10.1017/S0950268823000018. [16] Kovács E, Sahin-Tóth J, Tóthpál A, et al. Co-carriage of Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis among three different age categories of children in h ungary[J]. PLoS One, 2020, 15(2): e0229021. DOI: 10.1371/journal.pone.0229021. [17] Esposito S, Terranova L, Patria MF, et al. Streptococcus pneumoniae colonisation in children and adolescents with asthma: impact of the heptavalent pneumococcal conjugate vaccine and evaluation of potential effect of thirteen-valent pneumococcal conjugate vaccine[J]. BMC Infect Dis, 2016, 16: 12. DOI: 10.1186/s12879-016-1335-3. [18] Starkl P, Watzenboeck ML, Popov LM, et al. IgE effector mechanisms, in concert with mast cells, contribute to acquired host defense against Staphylococcusaureus [J]. Immunity, 2020, 53(4): 793-804. e9. DOI: 10.1016/j.immuni.2020.08.002. [19] Francois Watkins LK, Milucky JL, McGee L, et al. Nasopharyngeal carriage of Streptococcus pneumoniae among young children in Haiti before pneumococcal conjugate vaccine introduction[J]. J Infect Dis, 2021, 224(12 Suppl 2): S248-S257. DOI: 10.1093/infdis/jiab119. [20] Lam T, Chew D, Zhao H, et al. Species-resolved metagenomics of kindergarten microbiomes reveal microbial admixture within sites and potential microbial hazards[J]. Front Microbiol, 2022, 13: 871017. DOI: 10.3389/fmicb.2022.871017. [21] Tilahun M, Fiseha M, Ebrahim E, et al. High prevalence of asymptomatic nasopharyngeal carriage rate and multidrug resistance pattern of Streptococcus pneumoniae among pre-school children in north showa Ethiopia[J]. Infect Drug Resist, 2022, 15: 4253-4268. DOI: 10.2147/IDR.S377186. -





 下载:
下载: