Association between novel blood lipid indicators and risk of diabetes among Shenzhen residents
-
摘要:
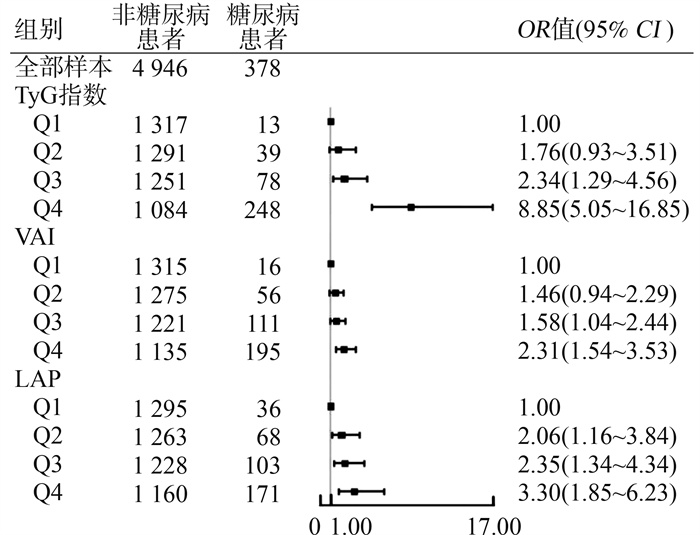
目的 探讨深圳市居民的新型血脂指数[如三酰甘油葡萄糖(triglyceride glucose, TyG)指数、脂质积累指数(lipid accumulation product, LAP)、内脏脂肪指数(visceral adiposity index, VAI)]与患糖尿病风险之间的关联, 为糖尿病早期预测提供参考。 方法 2021年4―10月于深圳市开展了一项居民心脑血管疾病及其危险因素的横断面调查, 采用多阶段分层整群随机抽样, 通过面对面问卷填写、体格检查和实验室检测的方法, 收集腰围(waist circumference, WC)、BMI、空腹血糖(fasting plasma glucose, FPG)、三酰甘油(triglyceride, TG)、高密度脂蛋白胆固醇(high-density lipoprotein cholesterol, HDL-C)等指标。根据研究对象新型血脂指数四分位数间距将其分为Q1、Q2、Q3和Q4组。采用logistic回归分析模型计算新型血脂指数与患糖尿病风险的OR值95% CI, 并采用限制性立方样条(restricted cubic spline, RCS)模型分析其潜在非线性的关联。 结果 本研究最终选取5 324名居民, 其中糖尿病患者378人(占7.10%), 非糖尿病患者4 946人(占92.90%)。Logistic回归分析模型经调整潜在混杂因素后, 对于TyG指数, Q4组(>8.94)比Q1组(≤8.16)患糖尿病风险更高(OR=8.85, 95% CI:5.05~16.81);对于LAP, Q4组(>34.82)比Q1组(≤12.69)患糖尿病风险亦增加(OR=3.30, 95% CI:1.85~6.23);对于VAI, Q4组(>1.85)患糖尿病风险为Q1组(≤0.93)的2.31倍(OR=2.31, 95% CI:1.54~3.53)。RCS模型结果显示, TyG指数、LAP和VAI与患糖尿病风险呈非线性关系(P < 0.05)。 结论 TyG指数、LAP和VAI与患糖尿病风险呈正相关, 可作为患糖尿病风险的评估指标。 Abstract:Objective This study aimed to explore the association between novel lipid indicators, triglyceride glucose (TyG) index, lipid accumulation product (LAP), and visceral adiposity index (VAI) and the risk of diabetes among residents in Shenzhen, providing a reference for the early prediction and warning of diabetes. Methods A cross-sectional survey on cardiovascular and cerebrovascular diseases and their risk factors among residents in Shenzhen was conducted from April to October 2021. Through multi-stage stratified cluster random sampling, face-to-face questionnaire filling, physical examinations, and laboratory tests were adopted to collect indicators such as waist circumference (WC), BMI, fasting plasma glucose (FPG), triglyceride (TG), and high-density lipoprotein cholesterol (HDL-C). According to the quartile intervals of the novel lipid indicators of the study subjects, they were divided into Q1, Q2, Q3, and Q4 groups. The odds ratio (OR) and its 95% confidence interval (95% CI) of the novel lipid indicators and diabetes were calculated using the logistic regression model, and the potential linear association was analyzed using the restricted cubic spline (RCS) model. Results Finally, 5 324 residents were selected in this study, among them, there were 378 diabetic patients (7.10%) and 4 946 non-diabetic patients (92.90%). After adjusting for potential confounding factors in the logistic regression model, for TyG, compared with the Q1 group (≤8.16), the risk of diabetes in the Q4 group (>8.94) increased (OR=8.85, 95% CI: 5.05-16.81); for LAP, compared with the Q1 group (≤12.69), the risk of diabetes in the Q4 group (>34.82) also increased (OR=3.30, 95% CI: 1.85-6.23); for VAI, the risk of diabetes in the Q4 group (>1.85) was 1.31 times than that of the Q1 group (≤0.93) (OR=2.31, 95% CI: 1.54-3.53). The results of the RCS model showed that the associations of TyG, LAP, and VAI with the risk of diabetes were nonlinear (P < 0.05). Conclusions TyG, LAP and VAI are positively correlated with the risk of diabetes and can be used as assessment indicators for the risk of diabetes. -
图 2 新型血脂指数与居民患糖尿病风险的限制性立方样条分析
A:三酰甘油葡萄糖指数与患糖尿病风险分析; B:内脏脂肪指数与患糖尿病风险分析; C:脂质积累指数与患糖尿病风险分析。
Figure 2. Respectively illustrate the variation trend of the OR value of diabetes as different new lipid indices increase. These curves are plotted using the restricted cubic spline method, visually demonstrating the nonlinear correlation between them
表 1 研究对象基线特征分析
Table 1. Characteristic differences between the diabetes group and the non-diabetes group among age, gender, educational level, marital status, lifestyle, medication usage, and various physiological indicators, etc., and presents the test statistics and P values
特征 合计①(n=5 324) 非糖尿病患者①(n=4 946) 糖尿病患者①(n=378) t/χ2/Z值 P值 年龄/岁 40.29±14.24 39.08±13.60 56.07±12.97 551.24 < 0.001 性别 14.66 < 0.001 男 2 60749.0) 2 376(48.2) 221(58.5) 女 2 717(51.0) 2 560(51.8) 157(41.5) 教育水平 133.56 < 0.001 初中及以下 1 562(29.34) 1 377(27.84) 185(48.94) 高中 1 152(21.64) 1 059(21.41) 93(24.60) 大学及以上 2 610(49.02) 2 510(50.75) 100(26.46) 婚姻状况 127.19 < 0.001 未婚 1 153(21.7) 1 143(23.1) 10(2.6) 已婚 3 96974.5) 3 639(73.6) 330(87.3) 其他 202(3.8) 164(3.3) 38(10.1) 吸烟 0.13 0.721 是 959(18.0) 875(17.7) 84(22.2) 否 4 365(82.0) 4 071(82.3) 294(77.8) 饮酒 4.68 0.035 是 1 937(36.4) 1 819(36.8) 118(31.2) 否 3 387(63.6) 3 127(63.2) 260(68.8) 体力活动 34.50 < 0.001 是 2 048(38.5) 1 849(23.1) 199(52.6) 否 3 276(61.5) 3 097(76.9) 179(47.4) 服用降压药 500.67 是 593(11.1) 419(8.5) 174(46.0) < 0.001 否 4 731(88.9) 4 527(91.5) 204(54.0) 服用降脂药 194.73 < 0.001 是 160(3.0) 104(2.1) 56(14.8) 否 5 164(97.0) 4 842(97.9) 322(85.2) 收缩压/mmHg 122.62±17.16 121.64±16.55 135.47±19.62 384.76 < 0.001 舒张压/mmHg 77.97±10.65 77.56±10.45 83.29±11.75 138.12 < 0.001 TyG指数 8.59±0.60 8.54±0.57 9.22±0.67 493.17 < 0.001 LAP 24.59(12.7, 44.1) 23.33(12.1, 41.9) 45.50(29.2, 72.1) 176.13 < 0.001 VAI 1.39(0.9, 2.2) 1.36(0.9, 2.1) 2.02(1.3, 3.0) 84.53 < 0.001 WC/cm 82.13±10.45 81.53±10.28 89.94±9.51 237.37 < 0.001 体重/kg 62.87±12.23 62.54±12.21 67.23±11.79 7.67 < 0.001 BMI/(kg·m-2) 23.70±3.56 23.53±3.50 25.83±3.55 150.20 < 0.001 注:TyG, 三酰甘油葡萄糖; LAP, 脂质积累指数; VAI, 内脏脂肪指数; WC, 腰围。
①以人数(占比/%)或x±s或M(P25, P75)表示。 -
[1] Deng RX, Chen WJ, Zhang ZP, et al. Association between visceral obesity index and diabetes: a systematic review and Meta-analysis[J]. J Clin Endocrinol Metab, 2024, 109(10): 2692-707. DOI: 10.1210/clinem/dgae303. [2] Liu AB, Lin YX, Meng TT, et al. Associations of the cardiometabolic index with insulin resistance, prediabetes, and diabetes in U.S. adults: a cross-sectional study[J]. BMC Endocr Disord, 2024, 24(1): 217. DOI: 10.1186/s12902-024-01676-4. [3] Natsume Y, Yamada T, Iida T, et al. Investigation of d-allulose effects on high-sucrose diet-induced insulin resistance via hyperinsulinemic-euglycemic clamps in rats[J]. Heliyon, 2021, 7(9): e08013. DOI: 10.1016/j.heliyon.2021.e08013. [4] Hill MA, Yang Y, Zhang LP, et al. Insulin resistance, cardiovascular stiffening and cardiovascular disease[J]. Metabolism, 2021, 119: 154766. DOI: 10.1016/j.metabol.2021.154766. [5] Deng H, Hu P, Li HX, et al. Novel lipid indicators and the risk of type 2 diabetes mellitus among Chinese hypertensive patients: findings from the Guangzhou heart study[J]. Cardiovasc Diabetol, 2022, 21(1): 212. DOI: 10.1186/s12933-022-01660-z. [6] Tao LC, Xu JN, Wang TT, et al. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations[J]. Cardiovasc Diabetol, 2022, 21(1): 68. DOI: 10.1186/s12933-022-01511-x. [7] 孙文宇, 乔晶, 孟敏敏, 等. 甘油三酯葡萄糖指数与2型糖尿病胰岛素抵抗及血管并发症的相关性[J]. 临床内科杂志, 2023, 40(10): 681-685. DOI: 10.3969/j.issn.1001-9057.2023.10.008.Sun WY, Qiao J, Meng MM, et al. Correlation between triglyceride glucose index and insulin resistance and vascular complications in type 2 diabetes mellitus[J]. J Clin Intern Med, 2023, 40(10): 681-685. DOI: 10.3969/j.issn.1001-9057.2023.10.008. [8] 康娟, 刘文徽, 常青, 等. 三酰甘油-葡萄糖指数及其衍生指数与老年男性代谢相关脂肪性肝病的相关性分析[J]. 解放军医学杂志, 2023, 48(11): 1344-1352. DOI: 10.11855/j.issn.0577-7402.0544.2023.1012.Kang J, Liu WH, Chang Q, et al. Association between triglyceride glucose index and its related derivative index and metabolic associated fatty liver disease in the elderly men[J]. Med J Chin PLA, 2023, 48(11): 1344-1352. DOI: 10.11855/j.issn.0577-7402.0544.2023.1012. [9] Alizargar J, Bai CH, Hsieh NC, et al. Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients[J]. Cardiovasc Diabetol, 2020, 19(1): 8. DOI: 10.1186/s12933-019-0982-2. [10] Pranata R, Huang I, Irvan, et al. The association between triglyceride-glucose index and the incidence of type 2 diabetes mellitus-a systematic review and dose-response Meta-analysis of cohort studies[J]. Endocrine, 2021, 74(2): 254-262. DOI: 10.1007/s12020-021-02780-4. [11] Wang BY, Zhang M, Liu Y, et al. Utility of three novel insulin resistance-related lipid indices for predicting type 2 diabetes mellitus among people with normal fasting glucose in rural China[J]. J Diabetes, 2018, 10(8): 641-652. DOI: 10.1111/1753-0407.12642. [12] Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects[J]. Metab Syndr Relat Disord, 2008, 6(4): 299-304. DOI: 10.1089/met.2008.0034. [13] Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp[J]. J Clin Endocrinol Metab, 2010, 95(7): 3347-3351. DOI: 10.1210/jc.2010-0288. [14] Vasques AC, Novaes FS, de Oliveira MDAS, et al. TyG index performs better than HOMA in a Brazilian population: a hyperglycemic clamp validated study[J]. Diabetes Res Clin Pract, 2011, 93(3): e98-e100. DOI: 10.1016/j.diabres.2011.05.030. [15] Yan GY, Li F, Elia C, et al. Association of lipid accumulation product trajectories with 5-year incidence of type 2 diabetes in Chinese adults: a cohort study[J]. Nutr Metab, 2019, 16: 72. DOI: 10.1186/s12986-019-0399-7. [16] Ahn N, Baumeister SE, Amann U, et al. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes[J]. Sci Rep, 2019, 9(1): 9693. DOI: 10.1038/s41598-019-46187-8. [17] Wu JS, Gong LL, Li QF, et al. A novel visceral adiposity index for prediction of type 2 diabetes and pre-diabetes in Chinese adults: a 5-year prospective study[J]. Sci Rep, 2017, 7(1): 13784. DOI: 10.1038/s41598-017-14251-w. [18] Han MH, Qin P, Li QM, et al. Chinese visceral adiposity index: a reliable indicator of visceral fat function associated with risk of type 2 diabetes[J]. Diabetes Metab Res Rev, 2021, 37(2): e3370. DOI: 10.1002/dmrr.3370. [19] Hameed EK, AbdulQahar ZH. Visceral adiposity index in female with type 2 diabetic mellitus and its association with the glycemic control[J]. Diabetes Metab Syndr, 2019, 13(2): 1241-1244. DOI: 10.1016/j.dsx.2019.01.039. [20] Molina MN, Ferder L, Manucha W. Emerging role of nitric oxide and heat shock proteins in insulin resistance[J]. Curr Hypertens Rep, 2016, 18(1): 1. DOI: 10.1007/s11906-015-0615-4. [21] Yang Q, Vijayakumar A, Kahn BB. Metabolites as regulators of insulin sensitivity and metabolism[J]. Nat Rev Mol Cell Biol, 2018, 19(10): 654-672. DOI: 10.1038/s41580-018-0044-8. -





 下载:
下载: