Investigating the influence of temperature on herpes zoster visits and its lagged effect in Beijing, China
-
摘要:
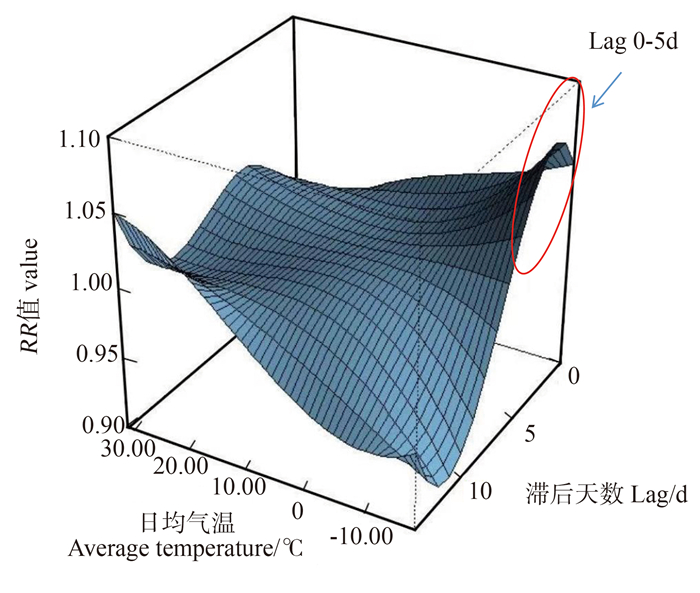
目的 基于分布滞后非线性模型评估北京市气温对带状疱疹就诊量的影响及其滞后效应。 方法 收集2016年1月―2021年12月北京市带状疱疹门诊病例就诊数据和同期气象数据。通过分布滞后非线性模型分析日均气温对北京市带状疱疹日就诊量的影响及其滞后效应。 结果 2016年1月―2021年12月北京市卫生健康大数据与政策研究中心电子病历共享工程数据库共报告带状疱疹门诊就诊患者488 100例。日均气温与带状疱疹日就诊量呈正相关(rs=0.098, P<0.05)。以日均气温的中位数12.59 ℃为参考值,高温和低温情况下的RR值均较高,低温影响出现于滞后早期(lag 0~5 d),而高温影响出现于后期(lag 3~5 d和12~14 d)。 结论 气温与北京市带状疱疹就诊量之间的关系呈非线性,低温对带状疱疹发病影响出现较早且显著,高温影响出现得更加持久,存在滞后效应。提示在极端温度下需加强预防带状疱疹发病。 Abstract:Objective To evaluate the effect of temperature on the number of herpes zoster visits and its lagged effect, in Beijing, China, using the distributed lag nonlinear model (DLNM). Methods Outpatient data for herpes zoster and meteorological data for the same period in Beijing, from January 2016 to December 2021, were collected. The influence of daily average temperature on the daily number of herpes zoster visits in Beijing, along with its lagged effect, was analyzed using the DLNM. Results From January 2016 to December 2021, a total of 488 100 outpatient visits for herpes zoster were reported in the "Electronic Medical Record Sharing Project Database" of the Beijing Health and Health Big Data and Policy Research Center. The daily average temperature was positively correlated with the daily number of herpes zoster outpatient visits (rs=0.098, P < 0.05). Taking the median daily average temperature of 12.59 ℃ as the reference value, the relative risks (RRs) were relatively high under both high and low temperatures. The low temperature effect occurred in the early lags (lag 0-5 d), while the high temperature effect occurred in the later lags (lag 3-5 d and 12-14 d). Conclusions The relationship between temperature and the number of herpes zoster outpatient visits in Beijing is nonlinear. The effect of low temperatures on the incidence of herpes zoster occurs early and is significant, while the effect of high temperatures is more prolonged, with a lagged effect. It suggests that attention should be paid to the prevention of herpes zoster during seasons of extreme temperatures. -
表 1 2016―2021年北京市带状疱疹门诊日就诊量与气象因素情况
Table 1. Statistics on daily outpatient visits for herpes zoster and meteorological factors in Beijing from 2016 to 2021
变量Variable 最小值Min P25 P50 P75 最大值Max x±s 带状疱疹日就诊量Daily outpatient visits for herpes zoster 28.00 134.00 239.00 287.00 470.00 222.67±89.02 日均气温Mean temperature/℃ -18.31 0.86 12.59 22.35 31.12 11.69±11.53 日均湿度Mean relative humidity/% 11.52 38.99 54.28 70.25 95.42 54.33±18.68 日累积降水Cumulative precipitation/mm 0 0 0 0.23 148.15 1.59±6.06 日均风速Mean wind velocity/(m·s-1) 2.20 3.92 4.86 6.29 17.17 5.42±2.19 表 2 2016―2021年北京市带状疱疹日就诊量与气象因素的Spearman相关系数矩阵
Table 2. Spearman correlation coefficient matrix between outpatient visits for herpes zoster and meteorological factors in Beijing from 2016 to 2021
变量
Variable带状疱疹日就诊量
Daily outpatient visits for herpes zoster日均气温
Mean temperature/℃日均湿度
Relative humidity/%日累积降水
Cumulative precipitation/mm日均风速
Mean wind velocity/(m·s-1)带状疱疹日就诊量Daily outpatient visits for herpes zoster 1.000 日均气温Mean temperature/℃ 0.098① 1.000 日均湿度Mean relative humidity/% 0.050① 0.407① 1.000 日累积降水Cumulative precipitation /mm -0.021 0.398① 0.545① 1.000 日均风速Mean wind velocity/(m·s-1) -0.072① -0.078① -0.494① -0.013 1.000 注:① P<0.05。
Note: ① P<0.05.表 3 不同时间自由度下相对危险度
Table 3. Relative risk table under different degrees of freedom over time
日均气温
Mean temperature/℃时间自由度=6
Degrees of freedom=6时间自由度=7
Degrees of freedom=7时间自由度=8
Degrees of freedom=8滞后天数
Lag daysRR值
value滞后天数
Lag daysRR值
value滞后天数
Lag daysRR值
value-10 0 1.02 0 1.03 0 1.02 5 1.01 5 1.01 5 1.01 10 0.97 10 0.96 10 0.96 0 0 1.01 0 1.01 0 1.01 5 1.00 5 1.00 5 1.00 10 1.00 10 1.00 10 1.00 10 0 1.00 0 1.00 0 1.00 5 1.00 5 1.00 5 1.00 10 1.00 10 1.00 10 1.00 20 0 0.98 0 0.98 0 0.98 5 1.00 5 1.00 5 1.00 10 1.00 10 1.00 10 1.00 30 0 0.94 0 0.95 0 0.94 5 1.00 5 1.01 5 1.01 10 1.00 10 1.00 10 1.00 -
[1] Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction[J]. Mayo Clin Proc, 2007, 82(11): 1341-1349. DOI: 10.4065/82.11.1341. [2] Choi JK, Park SH, Park S, et al. The changing epidemiology of herpes zoster over a decade in South Korea, 2006-2015[J]. Vaccine, 2019, 37(36): 5153-5160. DOI: 10.1016/j.vaccine.2019.07.086. [3] Yin D, Van Oorschot D, Jiang N, et al. A systematic literature review to assess the burden of herpes zoster disease in China[J]. Expert Rev Anti Infect Ther, 2021, 19(2): 165-179. DOI: 10.1080/14787210.2020.1792290. [4] Korostlil IA, Regan DG. Varicella-zoster virus in perth, western australia: Seasonality and reactivation[J]. PLoS One, 2016, 11(3): e0151319. DOI: 10.1371/journal.pone.0151319. [5] AL-Dahshan A, Chehab M, Ganesan N, et al. Epidemiology of herpes zoster in the State of qatar, 2012-2017[J]. Qatar Med J, 2020, 2020, (1): 1. DOI: 10.5339/qmj.2020.1. [6] Bhaskaran K, Gasparrini A, Hajat S, et al. Time series regression studies in environmental epidemiology[J]. Int J Epidemiol, 2013, 42(4): 1187. DOI: 10.1093/ije/dyt092. [7] Koshy E, Mengting L, Kumar H, et al. Epidemiology, treatment and prevention of herpes zoster: A comprehensive review[J]. Indian J Dermatol Venereol Leprol, 2018, 84: 251. DOI: 10.4103/ijdvl.IJDVL_1021_16. [8] Lai SW, Liao KF, Kuo YH, et al. The impacts of ambient temperature and ultraviolet radiation on the incidence of herpes zoster: an ecological study in Taiwan[J]. Int J Clin Pract, 2021, 75(4): e13854. DOI: 10.1111/ijcp.13854. [9] Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: Towards a global perspective[J]. BMJ Open, 2014, 4(6): e004833. DOI: 10.1136/bmjopen-2014-004833. [10] Kawai K, Vopham T, Drucker A, et al. Ultraviolet radiation exposure and risk of herpes zoster in three prospective cohort studies[J]. Mayo Clin Proc, 2019, 95(2): 283. DOI: 10.1016/j.mayocp.2019.08.022. -





 下载:
下载: