Association of silent information regulator 1 gene polymorphisms, pre-pregnancy body mass index, early pregnancy weight gain with preeclampsia
-
摘要:
目的 探讨沉默信息调节因子1(silent information regulator 1, SIRT1)基因多态性及其与孕前BMI、孕早期增重的交互作用对子痫前期(pre-eclampsia, PE)发生风险的影响。 方法 2020年10月―2023年10月在中南大学湘雅三医院和湖南省妇幼保健院产科开展病例对照研究,将诊断为PE的孕妇作为病例组,同期在这2所医院产检且血压正常的孕妇作为对照组。对研究对象进行问卷调查,并采集血液样本进行基因分型检测。采用logistic回归分析孕前BMI、孕早期增重和SIRT1基因多态性与PE发生的关联,并采用叉生分析和多因素logistic回归探讨SIRT1基因多态性与孕前BMI、孕早期增重的交互作用对PE发生的影响。 结果 共纳入研究对象602例(病例组202例,对照组400例)。孕前BMI过高孕妇发生PE的风险是孕前BMI正常孕妇的5.21倍(OR=5.21, 95% CI: 3.15~8.63),孕早期增重过多的孕妇发生PE的风险是孕早期增重适宜孕妇的3.38倍(OR=3.38, 95% CI: 2.20~5.18)。SIRT1基因rs2236319位点(加性模型:aOR=1.40, 95% CI: 1.01~1.95)、rs3740051位点(显性模型:aOR=1.59, 95% CI: 1.06~2.37;加性模型:aOR=1.51, 95% CI: 1.08~2.11)、rs10823108位点(显性模型:aOR=1.50, 95% CI: 1.01~2.23;加性模型:aOR=1.43, 95% CI: 1.02~1.99)与PE的发生风险增加相关。SIRT1基因rs11599176位点(共显性模型:aOR=0.65, 95% CI: 0.43~0.98;显性模型:aOR=0.62, 95% CI: 0.42~0.93;加性模型:aOR=0.66, 95% CI: 0.47~0.92)与PE的发生风险降低相关。未观察到SIRT1基因多态性与孕前BMI、孕早期增重对PE的影响存在交互作用。 结论 孕前BMI过高以及孕早期增重过多可能导致PE的发生风险增加。SIRT1基因rs11599176、rs2236319、rs3740051和rs10823108位点多态性与PE的发病可能有关。此外,SIRT1基因多态性与孕前BMI、孕早期增重对PE发生的影响均不存在交互作用。 -
关键词:
- 子痫前期 /
- 沉默信息调节因子1基因 /
- 交互作用
Abstract:Objective To explore the association of silent information regulator 1 (SIRT1) gene polymorphisms, pre-pregnancy BMI, and early pregnancy weight gain with pre-eclampsia (PE). Methods From October 2020 to October 2023, a case-control study was carried out in the obstetrics departments of The Third Xiangya Hospital of Central South University and Hunan Provincial Maternal and Child Health Care Hospital, in which pregnant women diagnosed with PE were selected as the case group, and pregnant women with normal blood pressure during prenatal examination in these two hospitals were selected as the control group during the same period. Questionnaires were conducted on the study subjects, and blood samples were collected for genotyping testing. Logistic regression analysis was conducted on the association between pre-pregnancy BMI, early pregnancy weight gain, and SIRT1 gene polymorphism with the occurrence of PE. Crossover analysis and multiple logistic regression were used to explore the interaction between SIRT1 gene polymorphism with pre-pregnancy BMI and early pregnancy weight gain on the occurrence of PE. Results There were 602 subjects (202 cases, 400 controls). The risk of PE in pregnant women with high pre-pregnancy BMI was 5.21 times higher than that of pregnant women with normal pre-pregnancy BMI (OR=5.21, 95% CI: 3.15-8.63), and the risk of PE in pregnant women with excessive early pregnancy weight gain was 3.38 times higher than that of pregnant women with suitable early pregnancy weight gain (OR=3.38, 95% CI: 2.20-5.18). The SIRT1 gene loci rs2236319 (additive model: aOR=1.40, 95% CI: 1.01-1.95), rs3740051 (dominant model: aOR=1.59, 95% CI: 1.06-2.37; additive model: aOR=1.51, 95% CI: 1.08-2.11), and rs10823108 (dominant model: aOR=1.50, 95% CI: 1.01-2.23; additive model: aOR=1.43, 95% CI: 1.02-1.99) were associated with an increased risk of PE occurrence. The gene loci rs11599176 was associated with a reduced risk of PE (codominant model: aOR=0.65, 95% CI: 0.43-0.98; dominant model: aOR=0.62, 95% CI: 0.42-0.93; additive model: aOR=0.66, 95% CI: 0.47-0.92). No significant interaction was observed between SIRT1 gene polymorphism and pre-pregnancy BMI or early pregnancy weight gain regarding their effects on PE. Conclusions A high pre-pregnancy BMI and excessive early pregnancy weight gain are associated with an increased risk of PE. Polymorphisms of the SIRT1 gene at rs11599176, rs2236319, rs3740051, and rs10823108 may be associated with the occurrence of PE. In addition, there is no interaction between SIRT1 gene polymorphisms and pre-pregnancy BMI or early pregnancy weight gain on the occurrence of PE. -
Key words:
- Pre-eclampsia /
- Silent information regulator 1 gene /
- Interaction
-
表 1 研究对象基本情况
Table 1. Basic information about the research subjects
变量Variable 病例组
Case group①(n=202)对照组
Control group①(n=400)χ2值value P值value 妊娠年龄/岁Gestational age /years 33.89 <0.01 <30 58(28.71) 202(50.50) 30~<35 88(43.57) 148(37.00) ≥35 56(27.72) 50(12.50) 居住地Place of residence 24.33 <0.01 城镇Town 170(84.16) 383(95.75) 农村Countryside 32(15.84) 17(4.25) 文化程度Education 21.32 <0.01 初中及以下Junior high school and below 18(8.91) 8(2.00) 高中或中专High school or technical secondary school 35(17.33) 45(11.25) 大专或本科及以上College degree or above 149(73.76) 347(86.75) 家庭人均年收入/万元Per capita annual household income /10 000 yuan 0.76 0.684 <4 23(11.39) 39(9.75) 4~8 49(24.26) 90(22.50) >8 130(64.35) 271(67.75) 妊娠并发症史History of pregnancy complications 8.63 0.003 无No 164(81.19) 359(89.75) 有Yes 38(18.81) 41(10.25) 不良妊娠史History of adverse pregnancy 2.89 0.089 无No 105(51.98) 237(59.25) 有Yes 97(48.02) 163(40.75) 孕期贫血史History of anemia during pregnancy 4.28 0.038 无No 164(81.19) 350(87.50) 有Yes 38(18.81) 50(12.50) 孕次Pregnancy 1.92 0.166 0 73(36.14) 168(42.00) ≥1 129(63.86) 232(58.00) 产次Parity 0.01 0.932 0 123(60.89) 245(61.25) ≥1 79(39.11) 155(38.75) 孕期吸烟史History of smoking during pregnancy 1.49 0.223 无No 196(97.03) 394(98.50) 有Yes 6(2.97) 6(1.50) 孕期二手烟暴露Exposure to secondhand smoke during pregnancy 7.84 0.005 无No 138(68.32) 226(56.50) 有Yes 64(31.68) 174(43.50) 孕期饮酒Drinking alcohol during pregnancy 2.96 0.086 无No 196(97.03) 375(93.75) 有Yes 6(2.97) 25(6.25) 孕期服用叶酸Taking folic acid during pregnancy 0.53 0.468 无No 2(0.99) 7(1.75) 有Yes 200(99.01) 393(98.25) 孕期饮茶Drinking tea during pregnancy 8.62 0.003 无No 166(82.18) 362(90.50) 有Yes 36(17.82) 38(9.50) 注:①以人数(占比/%)表示。
Note:① Number of people (proportion/%).表 2 孕前BMI、孕早期增重与PE的关联分析
Table 2. Analysis of the association between pre-pregnancy BMI, early pregnancy weight gain, and PE
变量Variable 病例组
Case group①(n=202)对照组
Control group①(n=400)OR值value(95% CI) aOR值value(95% CI)② 孕前BMI Pre-pregnancy BMI BMI过低BMI lower than the normal value 14(6.93) 79(19.75) 0.46(0.25~0.85) 0.60(0.31~1.17) BMI正常Normal BMI 110(54.46) 286(71.50) 1.00 1.00 BMI过高BMI higher than the normal value 78(38.61) 35(8.75) 5.80(3.67~9.14) 5.21(3.15~8.63) 孕早期增重Early pregnancy weight gain 增重不足Insufficient weight gain 18(8.91) 51(12.75) 1.02(0.57~1.84) 0.90(0.45~1.80) 增重适宜Appropriate weight gain 93(46.04) 269(67.25) 1.00 1.00 增重过多Excessive weight gain 91(45.05) 80(20.00) 3.29(2.25~4.82) 3.38(2.20~5.18) 注:PE,子痫前期。
①以人数(占比/%)表示;②调整妊娠年龄、居住地、文化程度、妊娠并发症史、孕期贫血史、孕期二手烟暴露、孕期饮茶等混杂的多因素logistic回归分析。
Note: PE, pre-eclampsia.
① Number of people (proportion/%); ② Multivariate logistic regression analysis adjusting for confounding factors such as gestational age, place of residence, educational level, history of pregnancy complications, history of anemia during pregnancy, exposure to second-hand smoke during pregnancy, and tea consumption during pregnancy.表 3 对照组人群基因型哈迪-温伯格平衡检验
Table 3. Hardy-Weinberg equilibrium test for the genotype of the control group population
基因位点Gene loci 实际频数
Actual frequency理论频数
Theoretical frequencyχ2值value P值value rs2273773(TT/TC/CC) 216/120/64 190/171/38 35.70 <0.01 rs2394443(GG/GC/CC) 268/80/52 237/142/21 75.81 <0.01 rs10823103(GG/AG/AA) 290/97/13 286/104/9 1.86 0.173 rs10997870(GG/GT/TT) 293/96/11 291/100/9 0.83 0.360 rs11596401(CC/TC/TT) 300/80/20 289/102/9 18.61 <0.01 rs11599176(AA/GA/GG) 197/176/27 203/164/33 2.19 0.140 rs2236319(AA/GA/GG) 219/162/19 225/150/25 2.56 0.109 rs4746720(TT/CT/CC) 116/207/77 120/198/81 0.81 0.368 rs12413112(GG/AG/AA) 282/105/13 280/110/11 0.69 0.406 rs12778366(TT/TC/CC) 285/103/12 283/107/10 0.52 0.472 rs1467568(AA/AG/GG) 293/74/33 272/116/12 51.64 <0.01 rs3740051(AA/GA/GG) 235/149/16 239/140/20 1.63 0.201 rs3758391(TT/CT/AA) 290/94/16 284/106/10 5.24 0.022 rs7069102(CC/CG/GG) 289/96/15 284/106/10 3.66 0.060 rs7896005(AA/AG/GG) 291/96/13 287/103/9 2.05 0.153 rs33955981(TT/TC/CC) 299/59/42 270/117/13 99.05 <0.01 rs10823108(GG/GA/AA) 221/162/17 228/148/24 3.59 0.058 rs10997868(CC/CA/AA) 291/98/11 289/102/9 0.62 0.433 rs2236318(TT/TA/AA) 302/90/8 301/92/7 0.18 0.671 rs33957861(CC/TC/TT) 283/103/14 280/110/11 1.43 0.231 rs1885472(GG/GC/CC) 289/97/14 285/105/10 2.58 0.108 表 4 沉默信息调节因子1基因多态性与子痫前期的关联分析
Table 4. Association analysis of silent information regulator 1 gene polymorphism and pre-eclampsia
基因位点
Gene loci遗传模型
Genetic model基因型
Genotype病例组
Case group(n=202)对照组
Control group(n=400)OR值value(95% CI)⑤ aOR值value(95% CI)⑥ rs11599176 共显性模型Codominant model AA 125(61.88) 197(49.25) 1.00 1.00 GA 69(34.16) 176(44.00) 0.62(0.43~0.88) 0.65(0.43~0.98) GG 8(3.96) 27(6.75) 0.47(0.21~1.06) 0.45(0.18~1.15) 显性模型Dominant model AA 125(61.88) 197(49.25) 1.00 1.00 GA+GG 77(38.12) 203(50.75) 0.60(0.42~0.84) 0.62(0.42~0.93) 隐性模型Recessive model AA+GA 194(96.04) 373(93.25) 1.00 1.00 GG 8(3.96) 27(6.75) 0.57(0.25~1.28) 0.54(0.22~1.37) 超显性模型Overdominant model AA+GG 133(65.84) 224(56.00) 1.00 1.00 GA 69(34.16) 176(44.00) 0.66(0.46~0.94) 0.70(0.47~1.05) 加性模型Additive model① 0.64(0.48~0.86) 0.66(0.47~0.92) rs2236319 共显性模型Codominant model AA 99(49.01) 219(54.75) 1.00 1.00 GA 88(43.56) 162(40.50) 1.20(0.85~1.71) 1.40(0.93~2.11) GG 15(7.43) 19(4.75) 1.75(0.85~3.85) 1.97(0.85~4.59) 显性模型Dominant model AA 99(49.01) 219(54.75) 1.00 1.00 GA+GG 103(50.99) 181(45.25) 1.26(0.90~1.77) 1.46(0.98~2.17) 隐性模型Recessive model AA+GA 187(92.57) 381(95.25) 1.00 1.00 GG 15(7.43) 19(4.75) 1.61(0.80~3.24) 1.68(0.74~3.82) 超显性模型Overdominant model AA+GG 114(56.44) 238(59.50) 1.00 1.00 GA 88(43.56) 162(40.50) 1.13(0.81~1.60) 1.30(0.87~1.94) 加性模型Additive model② 1.26(0.95~1.66) 1.40(1.01~1.95) rs3740051 共显性模型Codominant model AA 103(50.99) 235(58.75) 1.00 1.00 GA 85(42.08) 149(37.25) 1.30(0.91~1.85) 1.51(0.99~2.29) GG 14(6.93) 16(4.00) 2.00(0.94~4.24) 2.29(0.94~5.59) 显性模型Dominant model AA 103(51.0) 235(58.75) 1.00 1.00 GA+GG 99(49.0) 165(41.25) 1.37(0.97~1.92) 1.59(1.06~2.37) 隐性模型Recessive model AA+GA 188(93.07) 384(96.00) 1.00 1.00 GG 14(6.93) 16(4.00) 1.79(0.85~3.74) 1.91(0.80~4.57) 超显性模型Overdominant model AA+GG 117(57.92) 251(62.75) 1.00 1.00 GA 85(42.08) 149(37.25) 1.22(0.87~1.73) 1.40(0.94~2.10) 加性模型Additive model③ 1.35(1.02~1.79) 1.51(1.08~2.11) rs10823108 共显性模型Codominant model GG 99(49.01) 221(55.25) 1.00 1.00 GA 89(44.06) 162(40.50) 1.23(0.86~1.74) 1.45(0.96~2.18) AA 14(6.93) 17(4.25) 1.83(0.87~3.88) 1.97(0.82~4.77) 显性模型Dominant model GG 99(49.01) 221(55.25) 1.00 1.00 GA+AA 103(50.99) 179(44.75) 1.28(0.92~1.80) 1.50(1.01~2.23) 隐性模型Recessive model GG+GA 188(93.07) 383(95.75) 1.00 1.00 AA 14(6.93) 17(4.25) 1.68(0.81~3.47) 1.66(0.71~3.92) 超显性模型Overdominant model GG+AA 113(55.94) 238(59.50) 1.00 1.00 GA 89(44.06) 162(40.50) 1.16(0.82~1.63) 1.35(0.91~2.02) 加性模型Additive model④ 1.28(0.97~1.70) 1.43(1.02~1.99) 注:①加性模型下,rs11599176位点基因型为AA时赋值1,为GA时赋值2,为GG时赋值3;②加性模型下,rs2236319位点基因型为AA时赋值1,为GA时赋值2,为GG时赋值3;③加性模型下,rs3740051位点基因型为AA时赋值1,为GA时赋值2,为GG时赋值3;④加性模型下,rs10823108位点基因型为GG时赋值1,为GA时赋值2,为AA时赋值3;⑤单因素logistic回归分析;⑥调整妊娠年龄、居住地、文化程度、妊娠并发症史、孕期贫血史、孕期二手烟暴露、孕期饮茶、孕前BMI和孕早期增重等混杂因素的多因素logistic回归分析。
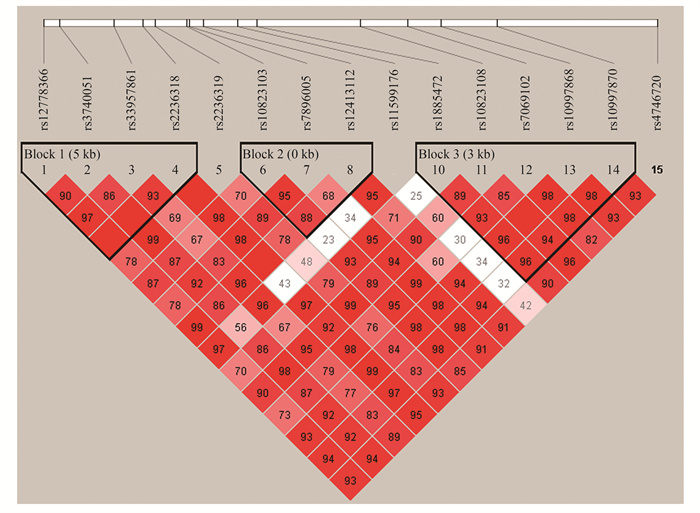
Note: ① In the additive model, assign 1 for rs11599176 locus genotype AA, 2 for GA, 3 for GG; ② In the additive model, assign 1 for rs2236319 locus genotype AA, 2 for GA, 3 for GG; ③ In the additive model, assign 1 for rs3740051 locus genotype AA, 2 for GA, 3 for GG; ④ In the additive model, assign 1 for rs10823108 locus genotype GG, 2 for GA, 3 for AA; ⑤ Univariate logistic regression analysis; ⑥ Multivariate logistic regression analysis adjusting for confounding factors like gestational age, residence, education level, pregnancy complication history, anemia history during pregnancy, second-hand smoke exposure during pregnancy, tea drinking during pregnancy, pre-pregnancy BMI and early pregnancy weight gain.表 5 沉默信息调节因子1基因各位点连锁不平衡检验
Table 5. Linkage disequilibrium test of SNPs in the silent information regulator 1 gene
r2 rs12778366 rs3740051 rs33957861 rs2236318 rs2236319 rs12778366 ― 0.048 0.925 0.029 0.040 rs3740051 ― ― 0.044 0.052 0.883 rs33957861 ― ― ― 0.026 0.032 rs2236318 ― ― ― ― 0.057 rs2236319 ― ― ― ― ― rs10823103 ― ― ― ― ― rs7896005 ― ― ― ― ― rs12413112 ― ― ― ― ― rs11599176 ― ― ― ― ― rs1885472 ― ― ― ― ― rs10823108 ― ― ― ― ― rs7069102 ― ― ― ― ― rs10997868 ― ― ― ― ― rs10997870 ― ― ― ― ― rs4746720 ― ― ― ― ― r2 rs10823103 rs7896005 rs12413112 rs11599176 rs1885472 rs12778366 0.027 0.021 0.968 0.484 0.017 rs3740051 0.047 0.052 0.044 0.036 0.047 rs33957861 0.016 0.025 0.919 0.489 0.016 rs2236318 0.808 0.818 0.029 0.011 0.779 rs2236319 0.035 0.054 0.041 0.030 0.044 rs10823103 ― 0.903 0.027 0.004 0.874 rs7896005 ― ― 0.017 0.008 0.886 rs12413112 ― ― ― 0.477 0.018 rs11599176 ― ― ― ― 0.005 rs1885472 ― ― ― ― ― rs10823108 ― ― ― ― ― rs7069102 ― ― ― ― ― rs10997868 ― ― ― ― ― rs10997870 ― ― ― ― ― rs4746720 ― ― ― ― ― r2 rs10823108 rs7069102 rs10997868 rs10997870 rs4746720 rs12778366 0.052 0.019 0.030 0.029 0.121 rs3740051 0.885 0.049 0.052 0.051 0.219 rs33957861 0.059 0.023 0.021 0.024 0.113 rs2236318 0.048 0.784 0.846 0.820 0.111 rs2236319 0.970 0.042 0.048 0.046 0.241 rs10823103 0.054 0.876 0.933 0.921 0.108 rs7896005 0.060 0.946 0.945 0.932 0.123 rs12413112 0.053 0.013 0.030 0.030 0.117 rs11599176 0.045 0.007 0.008 0.007 0.050 rs1885472 0.054 0.858 0.903 0.891 0.121 rs10823108 ― 0.051 0.065 0.252 0.252 rs7069102 ― ― 0.905 0.893 0.104 rs10997868 ― ― ― 0.962 0.126 rs10997870 ― ― ― ― 0.124 rs4746720 ― ― ― ― ― 注:“―”表示重复数据不再次展示。
Note: "―" for the non-representation of duplicate data.表 6 沉默信息调节因子1基因单倍型与子痫前期的关联分析
Table 6. Association analysis of silent information regulator 1 gene haplotype and pre-eclampsia
单倍型块
Haplotype block单倍型
Haplotype频率
Frequency/%对照组
Control group/%病例组
Case group/%χ2值value P值value OR值value(95% CI) Block 1 TACT 46.5 48.2 43.2 2.648 0.104 0.81(0.64~1.04) TGCT 24.0 22.3 27.3 3.789 0.052 1.32(1.00~1.74) CATT 14.7 15.4 13.2 1.038 0.308 0.86(0.61~1.22) TACA 13.7 13.2 14.9 0.650 0.420 1.16(0.82~1.64) Block 2 GAG 68.5 68.5 68.4 0.002 0.964 0.98(0.75~1.27) AGG 15.2 14.4 16.8 1.142 0.285 1.20(0.86~1.66) GAA 14.9 15.5 13.6 0.800 0.371 0.86(0.61~1.21) Block 3 GGCCG 57.0 59.1 57.0 4.308 0.038 0.75(0.59~0.96) GACCG 25.6 24.0 25.6 2.968 0.085 1.27(0.97~1.66) CGGAT 15.1 14.2 16.8 1.411 0.235 1.20(0.86~1.67) 注:Block 1,rs12778366-rs3740051-rs33957861-rs2236318;Block 2,rs10823103-rs7896005-rs12413112;Block 3,rs1885472-rs10823108-rs7069102-rs10997868-rs10997870。
Note: Block 1, rs12778366-rs3740051-rs33957861-rs2236318; Block 2, rs10823103-rs7896005-rs12413112; Block 3, rs1885472-rs10823108-rs7069102-rs10997868-rs10997870.表 7 沉默信息调节因子1基因与孕前BMI的相加交互作用
Table 7. The additive interaction of silent information regulator 1 gene and pre-pregnancy BMI
基因位点
Gene loci孕前
BMIPre-pregnancy BMIaOR值value(95% CI)① P值value RERI API S rs11599176 -0.35(-4.67, 3.96) -0.09(-1.19, 1.02) 0.90(0.24, 3.38) AA(-) 正常(-) Normal 1.00 GA+GG(+) 正常(-) Normal 0.61(0.36~1.02) 0.061 AA(-) 过高(+) Higher than normal 4.80(2.29~10.07) <0.01 GA+GG(+) 过高(+) Higher than normal 4.06(1.82~9.05) 0.001 rs4746720 1.96(-2.11, 6.02) 0.40(-0.31, 1.10) 2.02(0.35, 11.72) TT(-) 正常(-) Normal 1.00 CT+CC(+) 正常(-) Normal 0.68(0.40~1.16) 0.161 TT(-) 过高(+) Higher than normal 3.23(1.15~9.06) 0.026 CT+CC(+) 过高(+) Higher than normal 4.87(2.40~9.87) <0.01 rs12778366 5.95(-5.04, 16.95) 0.60(0.10, 1.09) 2.92(0.71, 12.02) TT(-) 正常(-) Normal 1.00 TC+CC(+) 正常(-) Normal 0.78(0.44~1.40) 0.408 TT(-) 过高(+) Higher than normal 4.32(2.30~8.09) <0.01 TC+CC(+) 过高(+) Higher than normal 10.06(3.36~30.13) <0.01 rs3740051 -5.76(-14.74, 3.23) -0.98(-2.83, 0.86) 0.46(0.16, 1.33) AA(-) 正常(-) Normal 1.00 GA+GG(+) 正常(-) Normal 1.93(1.15~3.25) 0.013 AA(-) 过高(+) Higher than normal 10.67(4.72~24.14) <0.01 GA+GG(+) 过高(+) Higher than normal 5.85(2.76~12.39) <0.01 rs2236318 -2.76(-8.04, 2.52) -0.71(-2.53, 1.12) TT(-) 正常(-) Normal 1.00 TA+AA(+) 正常(-) Normal 1.05(0.59~1.87) 0.870 TT(-) 过高(+) Higher than normal 6.60(3.48~12.53) <0.01 TA+AA(+) 过高(+) Higher than normal 3.90(1.49~10.18) 0.005 注:RERI, 交互作用超额相对危险度; API, 交互作用归因比; S, 交互作用指数。
①调整妊娠年龄、居住地、文化程度、妊娠并发症史、孕期贫血史、孕期二手烟暴露、孕期饮茶和孕早期增重等混杂的OR。
Note: RERI, relative excess risk of interaction; API, attributable proportions of interaction; S, the synergy index.
① OR adjusting for confounding factors such as gestational age, place of residence, educational level, history of pregnancy complications, history of anemia during pregnancy, exposure to second-hand smoke during pregnancy, tea consumption during pregnancy and early pregnancy weight gain.表 8 沉默信息调节因子1基因与孕早期增重的相加交互作用
Table 8. The additive interaction of silent information regulator 1 gene and early pregnancy weight gain
基因位点
Gene loci孕早期增重
Early pregnancy weight gainaOR值value(95% CI)① P值value RERI API S rs11599176 -0.17(-2.21, 1.88) -0.07(-0.95, 0.81) 0.89(0.22, 3.56) AA(-) 正常(-) Normal 1.00 GA+GG(+) 正常(-) Normal 0.58(0.33~1.04) 0.067 AA(-) 过多(+) More than normal 2.96(1.56~5.61) 0.001 GA+GG(+) 过多(+) More than normal 2.37(1.22~4.59) 0.011 rs4746720 -1.89(-5.69, 1.91) -0.67(-2.05, 0.71) 0.49(0.16, 1.49) TT(-) 正常(-) Normal 1.00 CT+CC(+) 正常(-) Normal 0.94(0.51~1.75) 0.853 TT(-) 过多(+) More than normal 4.76(2.02~11.22) <0.01 CT+CC(+) 过多(+) More than normal 2.81(1.43~5.54) 0.003 rs12778366 -1.42(-4.24, 1.40) -0.49(-1.67, 0.68) 0.57(0.18, 1.79) TT(-) 正常(-) Normal 1.00 TC+CC(+) 正常(-) Normal 1.23(0.64~2.36) 0.426 TT(-) 过多(+) More than normal 4.07(2.31~7.19) <0.01 TC+CC(+) 过多(+) More than normal 2.88(1.40~5.94) 0.004 rs3740051 2.76(-1.12, 6.65) 0.47(0.07, 0.88) 2.34(0.81, 6.72) AA(-) 正常(-) Normal 1.00 GA+GG(+) 正常(-) Normal 1.20(0.68~2.14) 0.545 AA(-) 过多(+) More than normal 2.86(1.53~5.33) 0.001 GA+GG(+) 过多(+) More than normal 5.83(2.81~12.10) <0.01 rs2236318 -1.01(-3.72, 1.71) -0.36(-1.49, 0.78) 0.65(0.19, 2.23) TT(-) 正常(-) Normal 1.00 TA+AA(+) 正常(-) Normal 1.06(0.55~2.05) 0.724 TT(-) 过多(+) More than normal 3.77(2.18~6.52) <0.01 TA+AA(+) 过多(+) More than normal 2.82(1.31~6.10) 0.008 注:RERI, 交互作用超额相对危险度; API, 交互作用归因比; S, 交互作用指数。
①调整妊娠年龄、居住地、文化程度、妊娠并发症史、孕期贫血史、孕期二手烟暴露、孕期饮茶和孕前BMI等混杂的OR。
Note: RERI, relative excess risk of interaction; API, attributable proportions of interaction; S, the synergy index.
① OR adjusting for confounding factors such as gestational age, place of residence, educational level, history of pregnancy complications, history of anemia during pregnancy, exposure to second-hand smoke during pregnancy, tea consumption during pregnancy and pre-pregnancy BMI.表 9 沉默信息调节因子1基因与孕前BMI的相乘交互作用
Table 9. The multiplicative interaction of silent information regulator 1 gene and pre-pregnancy BMI
因素1 Factor 1 因素2 Factor 2 β值value OR值value (95% CI)① P值value rs11599176 孕前BMI Pre-pregnancy BMI -0.155 0.86(0.57~1.30) 0.464 rs4746720 孕前BMI Pre-pregnancy BMI 0.158 1.17(0.81~1.69) 0.396 rs12778366 孕前BMI Pre-pregnancy BMI 0.166 1.18(0.75~1.88) 0.484 rs3740051 孕前BMI Pre-pregnancy BMI -0.175 0.84(0.56~1.25) 0.390 rs2236318 孕前BMI Pre-pregnancy BMI -0.320 0.73(0.45~1.18) 0.194 注:①调整妊娠年龄、居住地、文化程度、妊娠并发症史、孕期贫血史、孕期二手烟暴露、孕期饮茶和孕早期增重等混杂的多因素logistic回归分析。
Note: ① Multivariate logistic regression analysis adjusting for confounding factors such as gestational age, place of residence, educational level, history of pregnancy complications, history of anemia during pregnancy, exposure to second-hand smoke during pregnancy, tea consumption during pregnancy and early pregnancy weight gain.表 10 沉默信息调节因子1基因与孕早期增重的相乘交互作用
Table 10. The multiplicative interaction of silent information regulator 1 gene and early pregnancy weight gain
因素1 Factor1 因素2 Factor2 β值value OR值value (95% CI)① P值value rs11599176 孕早期增重Early pregnancy weight gain 0.250 1.28(0.89~1.85) 0.180 rs4746720 孕早期增重Early pregnancy weight gain -0.092 0.91(0.67~1.25) 0.567 rs12778366 孕早期增重Early pregnancy weight gain -0.062 0.94(0.63~1.40) 0.762 rs3740051 孕早期增重Early pregnancy weight gain 0.167 1.18(0.83~1.69) 0.357 rs2236318 孕早期增重Early pregnancy weight gain -0.051 0.95(0.62~1.45) 0.811 注:①调整妊娠年龄、居住地、文化程度、妊娠并发症史、孕期贫血史、孕期二手烟暴露、孕期饮茶和孕前BMI等混杂的多因素logistic回归分析。
Note: ① Multivariate logistic regression analysis adjusting for confounding factors such as gestational age, place of residence, educational level, history of pregnancy complications, history of anemia during pregnancy, exposure to second-hand smoke during pregnancy, tea consumption during pregnancy and pre-pregnancy BMI. -
[1] Magee LA, Nicolaides KH, von Dadelszen P. Preeclampsia[J]. N Engl J Med, 2022, 386(19): 1817-1832. DOI: 10.1056/nejmra2109523. [2] Magee LA, Brown MA, Hall DR, et al. The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice[J]. Pregnancy Hypertens, 2022, 27: 148-169. DOI: 10.1016/j.preghy.2021.09.008. [3] Chappell LC, Cluver CA, Kingdom J, et al. Pre-eclampsia[J]. Lancet, 2021, 398(10297): 341-354. DOI: 10.1016/S0140-6736(20)32335-7. [4] Hu XQ, Zhang LB. Mitochondrial dysfunction in the pathogenesis of preeclampsia[J]. Curr Hypertens Rep, 2022, 24(6): 157-172. DOI: 10.1007/s11906-022-01184-7. [5] Jacobsen DP, Fjeldstad HE, Olsen MB, et al. Microchimerism and pregnancy complications with placental dysfunction[J]. Semin Immunopathol, 2025, 47(1): 21. DOI: 10.1007/s00281-025-01045-w. [6] Bakrania BA, Spradley FT, Drummond HA, et al. Preeclampsia: linking placental ischemia with maternal endothelial and vascular dysfunction[J]. Compr Physiol, 2020, 11(1): 1315-1349. DOI: 10.1002/cphy.c200008. [7] Rana S, Burke SD, Karumanchi SA. Imbalances in circulating angiogenic factors in the pathophysiology of preeclampsia and related disorders[J]. Am J Obstet Gynecol, 2022, 226(2S): S1019-S1034. DOI: 10.1016/j.ajog.2020.10.022. [8] Liu ZZ, Wang CJ, Pei JN, et al. SIRT1 : a novel protective molecule in pre-eclampsia[J]. Int J Med Sci, 2022, 19(6): 993-1002. DOI: 10.7150/ijms.73012. [9] Wątroba M, Szewczyk G, Szukiewicz D. The role of sirtuin-1 (SIRT1) in the physiology and pathophysiology of the human placenta[J]. Int J Mol Sci, 2023, 24(22): 16210. DOI: 10.3390/ijms242216210. [10] Xie XW, Liu JY, Gao JY, et al. The crosstalk between cell death and pregnancy related diseases: a narrative review[J]. Biomed Pharmacother, 2024, 176: 116815. DOI: 10.1016/j.biopha.2024.116815. [11] Tossetta G, Fantone S, Piani F, et al. Modulation of NRF2/KEAP1 signaling in preeclampsia[J]. Cells, 2023, 12(11): 1545. DOI: 10.3390/cells12111545. [12] Mitanchez D, Jacqueminet S, Lebbah S, et al. Relative contribution of gestational weight gain, gestational diabetes, and maternal obesity to neonatal fat mass[J]. Nutrients, 2020, 12(11): 3434. DOI: 10.3390/nu12113434. [13] Zhang SM, Qiu X, Qin JB, et al. Effects of maternal pre-pregnancy BMI and gestational weight gain on the development of preeclampsia and its phenotypes: a prospective cohort study in China[J]. J Clin Med, 2022, 11(19): 5521. DOI: 10.3390/jcm11195521. [14] 中华医学会妇产科学分会妊娠期高血压疾病学组. 妊娠期高血压疾病诊治指南(2020)[J]. 中华妇产科杂志, 2020, 55(4): 227-238. DOI: 10.3760/cma.j.cn112141-20200114-00039.Hypertensive Disorders in Pregnancy Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Diagnosis and treatment of hypertension and pre-eclampsia in pregnancy: a clinical practice guideline in China(2020)[J]. Chin J Obstet Gynecol, 2020, 55(4): 227-238. DOI: 10.3760/cma.j.cn112141-20200114-00039. [15] 中国医疗保健国际交流促进会营养与代谢管理分会, 中国营养学会临床营养分会, 中华医学会糖尿病学分会, 等. 中国超重/肥胖医学营养治疗指南(2021)[J]. 中国医学前沿杂志(电子版), 2021, 13(11): 1-55. DOI: 10.12037/YXQY.2021.11-01.Nutrition and Metabolism Management Branch of China Healthcare International Exchange Promotion Association, Clinical Nutrition Branch of China Nutrition Society, diabetes Branch of Chinese Medical Association, et al. Guidelines for medical nutrition treatment of overweight/obesity in China (2021)[J]. Chinese Journal of the Frontiers of Medical Science, 2021, 13(11): 1-55. DOI: 10.12037/YXQY.2021.11-01. [16] 中华人民共和国国家卫生健康委员. 妊娠期妇女体重增长推荐值标准: WS/T 801—2022[S]. 北京: 中国标准出版社, 2022: 1-4.National Health Commission of the People's Republic of China. The recommended weight gain standards for pregnant women: WS/T 801-2022[S]. Beijing: China Standards Press, 2022: 1-4. [17] Shao YW, Qiu J, Huang H, et al. Pre-pregnancy BMI, gestational weight gain and risk of preeclampsia: a birth cohort study in Lanzhou, China[J]. BMC Pregnancy Childbirth, 2017, 17(1): 400. DOI: 10.1186/s12884-017-1567-2. [18] Liu XM, Du J, Wang GX, et al. Effect of pre-pregnancy body mass index on adverse pregnancy outcome in north of China[J]. Arch Gynecol Obstet, 2011, 283(1): 65-70. DOI: 10.1007/s00404-009-1288-5. [19] Vinturache A, Moledina N, McDonald S, et al. Pre-pregnancy body mass index (BMI) and delivery outcomes in a Canadian population[J]. BMC Pregnancy Childbirth, 2014, 14: 422. DOI: 10.1186/s12884-014-0422-y. [20] Bodnar LM, Ness RB, Markovic N, et al. The risk of preeclampsia rises with increasing prepregnancy body mass index[J]. Ann Epidemiol, 2005, 15(7): 475-482. DOI: 10.1016/j.annepidem.2004.12.008. [21] 王芳, 王素萍, 张亚玮, 等. 孕前体质指数和孕期增重与妊娠期高血压疾病的关系[J]. 中国妇幼保健, 2014, 29(35): 5766-5769. DOI: 10.7620/zgfybj.j.issn.1001-4411.2014.35.10.Wang F, Wang SP, Zhang YW, et al. Relationship between BMI before pregnancy, body weight gain during pregnancy and hypertensive disorder complicating pregnancy[J]. Maternal and Child, 2014, 29(35): 5766-5769. DOI: 10.7620/zgfybj.j.issn.1001-4411.2014.35.10. [22] Bodnar LM, Himes KP, Abrams B, et al. Early-pregnancy weight gain and the risk of preeclampsia: a case-cohort study[J]. Pregnancy Hypertens, 2018, 14: 205-212. DOI: 10.1016/j.preghy.2018.10.005. [23] Gaillard R, Durmuş B, Hofman A, et al. Risk factors and outcomes of maternal obesity and excessive weight gain during pregnancy[J]. Obesity, 2013, 21(5): 1046-1055. DOI: 10.1002/oby.20088. [24] Ruhstaller KE, Bastek JA, Thomas A, et al. The effect of early excessive weight gain on the development of hypertension in pregnancy[J]. Am J Perinatol, 2016, 33(12): 1205-1210. DOI: 10.1055/s-0036-1585581. [25] Khadir F, Rahimi Z, Vaisi-Raygani A, et al. Variants and haplotypes of SIRT1 (rs7895833, rs7069102, and rs2273773) are associated with the risk of preeclampsia and affect the trace elements and antioxidant enzymes levels[J]. Biochem Genet, 2024, 62(4): 2667-2685. DOI: 10.1007/s10528-023-10548-w. [26] Clark SJ, Falchi M, Olsson B, et al. Association of sirtuin 1 (SIRT1) gene SNPs and transcript expression levels with severe obesity[J]. Obesity, 2012, 20(1): 178-185. DOI: 10.1038/oby.2011.200. [27] Hou YT, Su BZ, Chen P, et al. Association of SIRT1 gene polymorphism and its expression for the risk of alcoholic fatty liver disease in the Han population[J]. Hepatol Int, 2018, 12(1): 56-66. DOI: 10.1007/s12072-017-9836-8. [28] Lin R, Yan DJ, Zhang YX, et al. Common variants in SIRT1 and human longevity in a Chinese population[J]. BMC Med Genet, 2016, 17(1): 31. DOI: 10.1186/s12881-016-0293-3. [29] Zeng ZP, Liao RF, Chen Q, et al. The association between SIRT1 genetic variation and type 2 diabetes mellitus is influenced by dietary intake in elderly Chinese[J]. Iran J Public Health, 2018, 47(9): 1272-1280. [30] Kedenko L, Lamina C, Kedenko I, et al. Genetic polymorphisms at SIRT1 and FOXO1 are associated with carotid atherosclerosis in the SAPHIR cohort[J]. BMC Med Genet, 2014, 15: 112. DOI: 10.1186/s12881-014-0112-7. [31] Zhou J, He YW, Fu L, et al. Gene polymorphisms of SIRT1 in patients with rheumatoid arthritis[J]. Int J Rheum Dis, 2022, 25(2): 210-217. DOI: 10.1111/1756-185X.14257. [32] Pang SC, Zhang ZJ, Zhou Y, et al. Genetic variants of SIRT1 gene promoter in type 2 diabetes[J]. Int J Endocrinol, 2023, 2023: 6919275. DOI: 10.1155/2023/6919275. [33] Song XF, Wang HD, Wang C, et al. Association of sirtuin gene polymorphisms with susceptibility to coronary artery disease in a north Chinese population[J]. Biomed Res Int, 2022, 2022: 4294008. DOI: 10.1155/2022/4294008. [34] Zou T, Liu JY, Qin Q, et al. Role of rs873601 polymorphisms in prognosis of lung cancer patients treated with platinum-based chemotherapy[J]. Biomedicines, 2023, 11(12): 3133. DOI: 10.3390/biomedicines11123133. [35] Maszlag-Török R, Boros FA, Vécsei L, et al. Gene variants and expression changes of SIRT1 and SIRT6 in peripheral blood are associated with Parkinson's disease[J]. Sci Rep, 2021, 11(1): 10677. DOI: 10.1038/s41598-021-90059-z. [36] Yue XG, Yang ZG, Zhang Y, et al. Correlations between SIRT1 gene polymorphisms and diabetic kidney disease[J]. R Soc Open Sci, 2018, 5(6): 171871. DOI: 10.1098/rsos.171871. [37] Huang GC, Wang YK, Qin LY, et al. Association and functional analysis of angiotensin-converting enzyme 2 genetic variants with the pathogenesis of pre-eclampsia[J]. Front Endocrinol (Lausanne), 2022, 13: 926512. DOI: 10.3389/fendo.2022.926512. -





 下载:
下载: