-
摘要:
目的 了解孕妇微量元素内暴露水平,探讨多种微量元素联合暴露与早产的关系。 方法 选取2012年3月―2016年2月于山西医科大学第一医院产科住院分娩的1 922对母婴作为研究对象,采用感耦合等离子体质谱法测定母血及脐带血中钒(Vanadium, V)、铬(Chromium, Cr)、锰(Manganese, Mn)、钴(Cobalt, Co)、镍(Nickel, Ni)、铜(Copper, Cu)、锌(Zinc, Zn)、硒(Selenium, Se)、钼(Molybdenum, Mo)的浓度,利用分位数g-计算(quartile g-computation, QGCOMP)分析多种微量元素联合暴露与早产的关系。 结果 与Cu低水平相比,母血Cu中水平是早产的危险因素(OR=1.58, 95% CI:1.01~2.49);与Se低水平相比,母血Se高水平是早产的保护因素(OR=0.50, 95% CI:0.26~0.96);与Mn低水平相比,脐带血Mn高水平是早产的危险因素(OR=1.70, 95% CI:1.04~2.78);与Zn低水平相比,脐带血Zn中水平(OR=0.41, 95% CI:0.26~0.66)和高水平(OR=0.54, 95% CI:0.33~0.88)均是早产的保护因素。QGCOMP分析 结果 显示,母血、脐带血中微量元素联合暴露对早产影响的总效应值分别为-0.53(95% CI:-0.86~-0.19)、-0.47(95% CI:-0.84~-0.09)。母血中微量元素联合暴露对降低孕妇早产发生贡献程度最大的是Cr,脐带血微量元素联合暴露中Zn的负向权重最大。 结论 微量元素联合暴露与早产的发生有关,Zn、Se和Cr高水平能够降低早产的发生风险。 Abstract:Objective To examine the association between trace elements co-exposure and risk of preterm birth. Methods A total of 1 922 mother infant pairs who joined a birth cohort in taiyuan from 2012 to 2016 were selected as the study population. The concentrations of Vanadium (V), Chromium (Cr), Manganese (Mn), Cobalt (Co), Nickel (Ni), Copper (Cu), Zinc (Zn), Selenium (Se), and Molybdenum (Mo) in maternal and umbilical cord blood were determined using inductively coupled plasma mass spectrometry (ICP-MS). We employed quartile g-computation (QGCOMP) to examine trace elements co-exposure in relation to preterm birth. Results An increased risk of preterm birth was associated with maternal Cu (OR=1.58, 95% CI: 1.01-2.49). High maternal exposure level of Se was associated with preterm birth (OR=0.50, 95% CI: 0.26-0.96). An increased risk of preterm birth was associated with cord blood Mn (OR=1.70, 95% CI: 1.04-2.78). Both medium (OR=0.41, 95% CI: 0.26-0.66) and high (OR=0.54, 95% CI: 0.33-0.88) cord blood level of Zn was associated with preterm birth. The QGCOMP showed that preterm birth was associated with maternal metal co-exposure (-0.53, 95% CI: -0.86--0.19) and cord metal co-exposure (-0.47, 95% CI: -0.84--0.09). Cr contributed the most to the reduction in preterm birth in maternal trace elements co-exposure and Zn contributed the most in cord trace elements co-exposure. Conclusions Our study suggested that trace elements are associated with preterm birth, and the decreasing risk is driven by Zn, Se and Cr. -
Key words:
- Trace elements /
- Co-exposure /
- Preterm birth
-
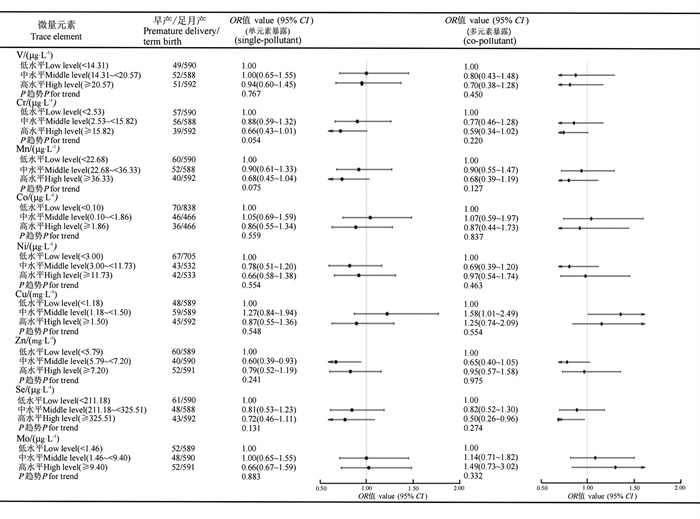
图 1 母血微量元素水平与早产的关系
V:钒;Cr:铬;Mn:锰;Co:钴;Ni:镍;Cu:铜;Zn:锌;Se:硒;Mo:钼;调整孕妇年龄、孕妇文化程度、孕期体育活动、孕前BMI、孕期增重、妊娠期高血压疾病、孕期主被动吸烟。
Figure 1. Relationship between maternal blood trace element levels and premature delivery
V: Vanadium; Cr: Chromium; Mn: Manganese; Co: Cobalt; Ni: Nickel; Cu: Copper; Zn: Zinc; Se: Selenium; Mo: Molybdenum; The adjustment factors were maternal age, maternal education level, pre-pregnancy BMI, pregnancy weight gain, gestational hypertension, and active and passive smoking during pregnanay.
图 2 脐带血微量元素水平与早产的关系
V:钒;Cr:铬;Mn:锰;Co:钴;Ni:镍;Cu:铜;Zn:锌;Se:硒;Mo:钼;调整孕妇年龄、孕妇文化程度、孕期体育活动、孕前BMI、孕期增重、妊娠期高血压疾病、孕期主被动吸烟。
Figure 2. Relationship between umbilical cord blood trace element levels and premature delivery
V: Vanadium; Cr: Chromium; Mn: Manganese; Co: Cobalt; Ni: Nickel; Cu: Copper; Zn: Zinc; Se: Selenium; Mo: Molybdenum; The adjustment factors were maternal age, maternal education level, pre-pregnancy BMI, pregnancy weight gain, gestational hypertension, and active and passive smoking during pregnanay.
图 3 母血和脐带血微量元素联合暴露与早产的关系
Cr:铬;Mo:钼;Zn:锌;Mn:锰;Cu:铜;Se:硒;Ni:镍;调整因素为孕妇年龄、孕妇文化程度、孕前BMI、孕期增重、妊娠期高血压、孕期主被动吸烟。
Figure 3. Relationship between combined exposure of trace elements in maternal blood and umbilical cord blood and premature birth
Cr: Chromium; Mo: Molybdenum; Zn: Zinc; Mn: Manganese; Cu: Copper; Se: Selenium; Ni: Nickel; The adjustment factors were maternal age, maternal education level, pre-pregnancy BMI, pregnancy weight gain, gestational hypertension, and active and passive smoking during pregnanay.
表 1 孕妇早产一般情况及影响因素分析
Table 1. Analysis of general situation and influencing factors of premature birth in pregnant woman
变量Variable 早产Premature delivery①(n=152) 足月产Term birth①(n=1 770) P值vaule 孕妇年龄/岁Maternal age/years 0.971② < 25 15(9.87) 120(6.78) 25~<30 52(34.21) 690(38.98) 30~45 85(55.92) 960(54.24) 孕妇文化程度Educational level of pregnant women 0.001② 初中及以下Junior high school and below 47(30.92) 306(17.29) 高中/中专/大专High school / technical secondary school/college 47(30.92) 587(33.16) 大学及以上University and above 58(38.16) 877(49.55) 孕前BMI Pre pregnancy BMI 0.697② 较低Lower 25(16.45) 235(13.28) 正常Normal 85(55.92) 1 129(63.78) 超重/肥胖Overweight/obese 42(27.63) 406(22.94) 孕期增重Weight gain during pregnancy 0.031② 不足Deficiency 44(28.95) 309(17.46) 适宜Suitable 43(28.29) 626(35.37) 增多Increase 65(42.76) 835(47.17) 孕期主被动吸烟Active and passive smoking during pregnancy 0.663③ 是Yes 130(85.53) 1 536(86.78) 否No 22(14.47) 234(13.22) 孕期体育活动/(h·周-1) Physical activity during pregnancy/(h·week-1) 0.003② < 7 61(40.13) 528(29.83) 7~<10 53(34.87) 624(35.25) ≥10 38(25.00) 618(34.92) 产次Parity 0.413③ 初产Primipara 106(69.74) 1 289(72.82) 多产Prolific 46(30.26) 481(27.18) 妊娠期高血压疾病Hypertensive disorder complicating pregnancy 0.001③ 是Yes 57(37.5) 121(6.84) 否No 95(62.5) 1 649(93.16) 妊娠期糖尿病Gestational diabetes mellitus 0.741③ 是Yes 64(42.11) 721(40.73) 否No 88(57.89) 1 049(59.27) 注:①以人数(占比/%)表示;②采用秩和检验;③采用χ2检验。
Note: ① Number of people (proportion/%); ② Rank sum test was used; ③ Test with χ2.表 2 早产和足月产孕妇微量元素水平
Table 2. Micronutrient levels in preterm and term pregnant women
微量元素Trace element 总人群Total population (n=1 922) 早产Premature delivery (n=152) 足月产Term birth (n=1 770) r 检出人数Number of people detected/% P50(P25, P75) 检出人数Number of people detected/% P50(P25, P75) 检出人数Number of people detected/% P50(P25, P75) 母血Maternal blood V/(μg·L-1) 1 554(80.85) 17.60(10.39, 22.68) 129(84.87) 17.64(11.96, 22.45) 1 425(80.51) 17.60(10.38, 22.70) 0.68 Cr/(μg·L-1) 1 443(75.08) 3(0.22, 29.59) 107(70.39) 4.72(0.10, 16.47) 1 336(75.48) 7.28(0.33, 30.90) 0.46 Mn/(μg·L-1) 1 768(91.99) 28.97(19.15, 39.81) 133(87.50) 24.94(17.53, 37.71) 1 635(92.37) 29.20(19.26, 40.10) 0.11 Co/(μg·L-1) 1 014(52.76) 0.33(0.05, 1.93) 82(53.95) 0.27(0.05, 1.42) 932(52.66) 0.34(0.05, 1.94) 0.45 Ni/(μg·L-1) 1 150(59.83) 6.48(1.50, 13.22) 85(55.92) 5.58(1.50, 12.66) 1 065(60.17) 6.62(1.50, 13.34) 0.39 Cu/(mg·L-1) 1 922(100.00) 1.35(1.09, 1.59) 152(100.00) 1.32(1.13, 1.52) 1 770(100.00) 1.35(1.09, 1.59) 0.33 Zn/(mg·L-1) 1 922(100.00) 6.47(5.35, 7.66) 152(100.00) 6.31(5.00, 7.82) 1 770(100.00) 6.48(5.39, 7.65) 0.28 Se/(μg·L-1) 1 922(100.00) 249.79(191.91, 376.59) 152(100.00) 233.29(181.28, 371.90) 1 770(100.00) 250.58(193.48, 378.01) 0.52 Mo/(μg·L-1) 1 600(83.25) 4.10(0.97, 11.19) 130(85.53) 4.04(0.93, 11.25) 1 470(83.05) 4.11(0.97, 11.18) 0.52 脐带血Umbilical cord blood V/(μg·L-1) 1 406(73.15) 15.41(2.00, 21.74) 117(76.97) 16.26(4.88, 21.27) 1 289(72.82) 15.37(2.00, 21.74) Cr/(μg·L-1) 1 656(86.16) 8.71(3.30, 42.93) 135(88.82) 8.67(3.23, 46.10) 1 521(85.93) 8.74(3.31, 41.63) Mn/(μg·L-1) 1 922(100.00) 54.63(42.16, 72.00) 152(100.00) 57.42(42.28, 79.14) 1 770(100.00) 54.41(42.13, 71.47) Co/(μg·L-1) 1 056(54.94) 0.26(0.05, 0.74) 87(57.24) 0.26(0.05, 1.17) 969(54.75) 0.26(0.05, 0.73) Ni/(μg·L-1) 973(50.62) 3.15(1.50, 12.51) 85(55.92) 6.17(1.50, 13.48) 888(50.17) 3.03(1.50, 12.47) Cu/(mg·L-1) 1 922(100.00) 0.52(0.44, 0.62) 152(100.00) 0.52(0.44, 0.60) 1 770(100.00) 0.52(0.44, 0.62) Zn/(mg·L-1) 1 922(100.00) 2.54(2.15, 2.99) 152(100.00) 2.30(1.93, 2.88) 1 770(100.00) 2.56(2.17, 3.01) Se/(μg·L-1) 1 922(100.00) 240.24(200.44, 295.76) 152(100.00) 229.20(194.02, 279.15) 1 770(100.00) 241.09(201.44, 297.99) Mo/(μg·L-1) 1 603(83.40) 2.10(0.79, 7.55) 128(84.21) 1.72(0.76, 7.68) 1 475(83.33) 2.17(0.79, 7.54) 注:V,钒;Cr,铬;Mn,锰;Co,钴;Ni,镍;Cu,铜;Zn,锌;Se,硒;Mo,钼。
Note: V, Vanadium; Cr, Chromium; Mn, Manganese; Co, Cobalt; Ni, Nickel; Cu, Copper; Zn, Zinc; Se, Selenium; Mo, Molybdenum. -
[1] Qiao J, Wang YY, Li XH, et al. A Lancet Commission on 70 years of women′s reproductive, maternal, newborn, child, and adolescent health in China [J]. Lancet, 2021, 397(10293): 2497-2536. doi: 10.1016/S0140-6736(20)32708-2. [2] Zhang WX, Chen H, Xia W, et al. Associations of plasma manganese with adverse pregnancy outcomes: nested case-control studies in a Chinese birth cohort [J]. Chemosphere, 2023, 345: 140550. doi: 10.1016/j.chemosphere.2023.140550. [3] Hao YX, Yan LL, Pang YM, et al. Maternal serum level of manganese, single nucleotide polymorphisms, and risk of spontaneous preterm birth: a nested case-control study in China[J]. Environ Pollut, 2020,262:114187. DOI: 10.1016/j.envpol.2020.114187. [4] Issah I, Duah MS, Arko-Mensah J, et al. Exposure to metal mixtures and adverse pregnancy and birth outcomes: a systematic review [J]. Sci Total Environ, 2024, 908: 168380. doi: 10.1016/j.scitotenv.2023.168380. [5] Gohari H, Khajavian N, Mahmoudian A, et al. Copper and zinc deficiency to the risk of preterm labor in pregnant women: a case-control study [J]. BMC Pregnancy Childbirth, 2023, 23(1): 366. doi: 10.1186/s12884-023-05625-2. [6] Ashrap P, Watkins DJ, Mukherjee B, et al. Performance of urine, blood, and integrated metal biomarkers in relation to birth outcomes in a mixture setting [J]. Environ Res, 2021, 200: 111435. doi: 10.1016/j.envres.2021.111435. [7] Kumari D, Garg S, Bhawrani P. Zinc homeostasis in immunity and its association with preterm births [J]. Scand J Immunol, 2022, 95(4): e13142. doi: 10.1111/sji.13142. [8] Barman M, Brantsæter AL, Nilsson S, et al. Maternal dietary selenium intake is associated with increased gestational length and decreased risk of preterm delivery [J]. Br J Nutr, 2020, 123(2): 209-219. doi: 10.1017/S0007114519002113. [9] McDougall AR, Dore G, Aboud L, et al. The effect of selenium supplementation in pregnant women on maternal, fetal, and newborn outcomes: a systematic review and Meta-analysis [J]. Am J Obstet Gynecol MFM, 2023, 5(11): 101160. doi: 10.1016/j.ajogmf.2023.101160. [10] Liu J, Ruan FY, Cao ST, et al. Associations between prenatal multiple metal exposure and preterm birth: comparison of four statistical models [J]. Chemosphere, 2022, 289: 133015. doi: 10.1016/j.chemosphere.2021.133015. [11] Freire C, Amaya E, Gil F, et al. Placental metal concentrations and birth outcomes: the environment and childhood (INMA) project [J]. Int J Hyg Environ Health, 2019, 222(3): 468-478. doi: 10.1016/j.ijheh.2018.12.014. [12] Eaves LA, Keil AP, Jukic AM, et al. Toxic metal mixtures in private well water and increased risk for preterm birth in North Carolina [J]. Environ Health, 2023, 22(1): 69. doi: 10.1186/s12940-023-01021-7. [13] Zhao L, Wang SL, Liu M, et al. Maternal urinary metal(loid)s and risk of preterm birth: a cohort study in the Tibetan Plateau [J]. Environ Pollut, 2023, 333: 122085. doi: 10.1016/j.envpol.2023.122085. [14] Huang H, Wei LM, Chen X, et al. Cord serum elementomics profiling of 56 elements depicts risk of preterm birth: evidence from a prospective birth cohort in rural Bangladesh [J]. Environ Int, 2021, 156: 106731. doi: 10.1016/j.envint.2021.106731. [15] Wang ZK, Huang SD, Zhang WL, et al. Chemical element concentrations in cord whole blood and the risk of preterm birth for pregnant women in Guangdong, China [J]. Ecotoxicol Environ Saf, 2022, 247: 114228. doi: 10.1016/j.ecoenv.2022.114228. -





 下载:
下载: